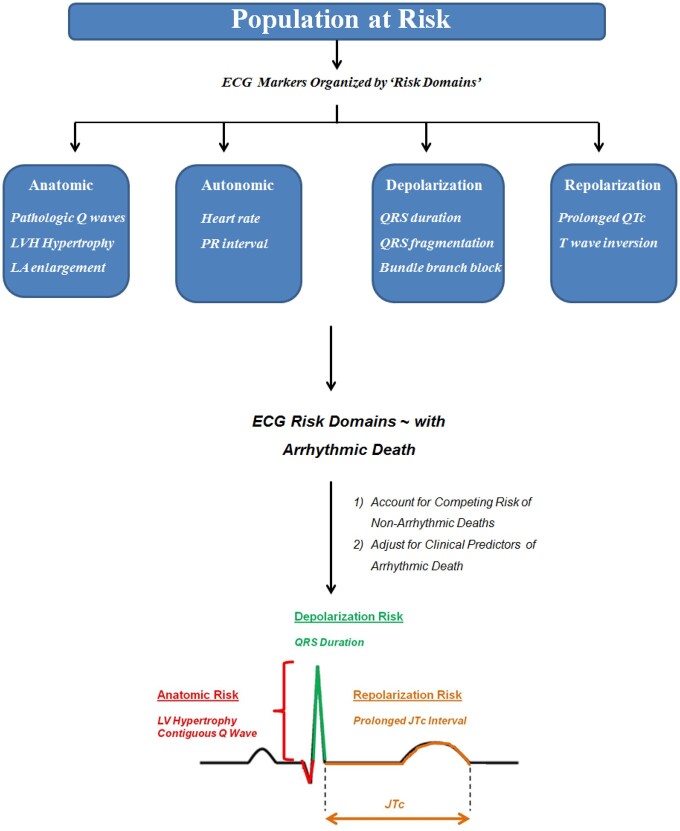
Figure 1.
A pathophysiology-based approach to electrocardiographic prediction of sudden arrhythmic death risk. In this study, we assessed the association between several easily measurable electrocardiographic markers and the risk of sudden of arrhythmic death in patients with coronary heart disease and relatively preserved left ventricular function. Electrocardiographic markers were organized into pathophysiology-based ‘risk domains’ including markers reflecting anatomic risk, autonomic function, as well as depolarization and repolarization abnormalities. In models (1) accounting for the competing risk of non-arrhythmic deaths and (2) adjusted for clinical risk factors associated with arrhythmic death (age, sex, race/ethnicity, hypertension, diabetes mellitus, atrial fibrillation, left ventricular ejection fraction, New York Heart Association functional class, and β-blocker use), four electrocardiographic markers were independently associated with arrhythmic death: left ventricular hypertrophy, contiguous Q waves, QRS duration, and a prolonged JTc interval. ECG, electrocardiographic; LA, left atrial; LVH, left ventricular hypertrophy; NYHA, New York Heart Association functional class.