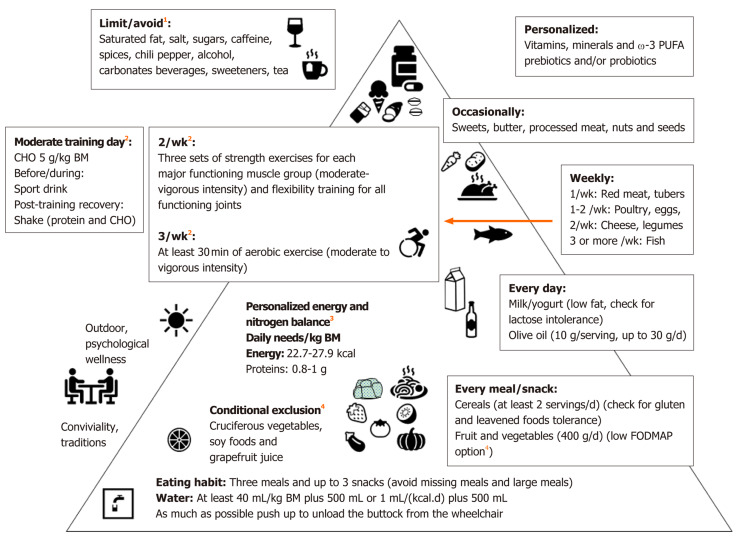
Figure 1.
Mediterranean diet based and exercise pyramid for individuals with spinal cord injury. Dietary advice from the previous indications for veterans[70], individuals with spinal cord injury with or without neurogenic bowel dysfunction[14,36,50,63,69,73], chronic kidney disease[71], chronic pain[72] and irritable bowel syndrome[18]. 1Limit/avoid: Potential undeliverable effects[11,36,79,94-96]; 2Exercise recommendations, derived from the integration of two recent papers[101,102] devoted to adults with spinal cord injury, are aimed to improve muscle strength, cardiorespiratory fitness, flexibility and cardiometabolic health. As a general rule, the exercise intensity should progress with time from moderate to vigorous at a rate (weeks-months) dependent from the initial level of fitness of the individual. However, personalized training is deliverable associated with sport-type-targeted nutritional recommendations (including timing and supplementation) for Paralympic athletes[64]; 3Personalized energy and nitrogen balance[50,64]: Ideal body mass 10%-15% and 5%-10% lower that for quadriplegia and paraplegia, respectively; Energy: 22.7 kcal/(kg·d) and 27.9 kcal/(kg·d) for quadriplegia and paraplegia, respectively and 30-40 kcal/(kg·d) in the presence of pressure ulcers; Proteins: Stage II pressure ulcers: 1.2-1.5 g/(kg·d), Stage III and IV pressure ulcers: 1.5-2.0 g/(kg·d); Paralympic athletes: 1.2-1.7 g/(kg·d); 4Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols: Banana, blueberry, strawberry, grape, melon, kiwi, cucumber, eggplant, green beans, lettuce, spinach, chives, pumpkin, tomato, zucchini. Cranberry juice may be associated with reduced urinary tract infection but could induce food-drug interactions, which can be observed also with other foods and beverages (conditional exclusion)[70,90]. BM: Body mass; w-3 PUFA: Omega-3 polyunsaturated fatty acids; CHO: Carbohydrates; FODMAP: Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.