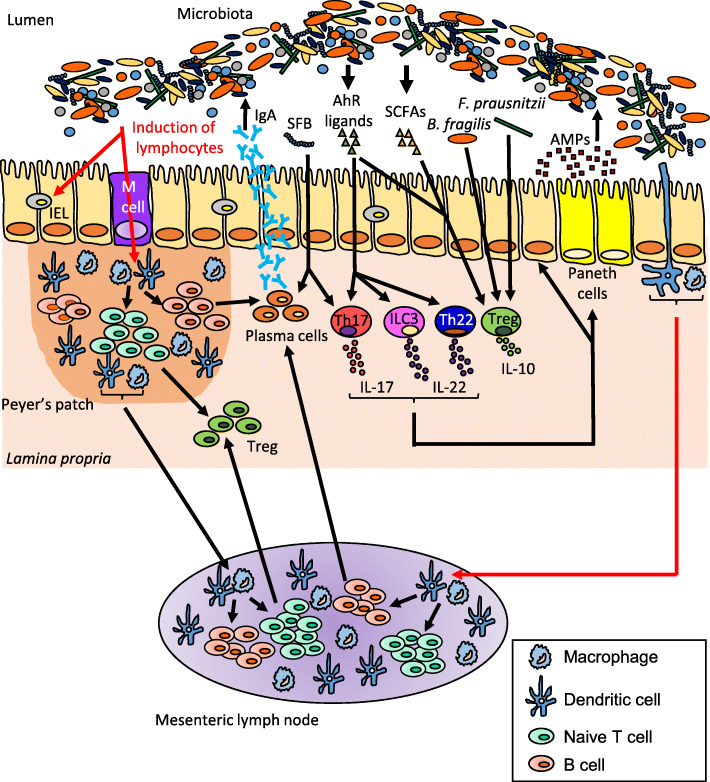
Fig. 1.
The gut microbiota modulates the intestinal immune response. The gut microbiota influences the development of T cell subsets, intraepithelial lymphocytes (IELs) and are critical for the induction of plasma cells which produce immunoglobulin A (IgA). Dendritic cells (DCs) sample microbial antigens that pass through the epithelial barrier via microfold (M) cells or capture antigens from the lumen directly by extending dendrites between the intestinal epithelial cells. Some of these DCs migrate to the mesenteric lymph nodes and induce naïve T cells differentiation into regulatory T-cell (Treg) by production of transforming growth factor β (TGF-β) and retinoic acid. Segmented filamentous bacteria (SFB) exhibit pro-inflammatory effects by inducing IL-17 and IgA production, whereas Bacteroides fragilis, Faecalibacterium prausnitzii and short-chain fatty acids (SCFAs) exhibit anti-inflammatory effects via recruitment of Treg that produce the immunosuppressive cytokine IL-10. The intestinal flora also regulates immune response by the production of aryl hydrocarbon receptor (AhR) ligands able to activate AhR, highly expressed on IELs, Th17, Th22, innate lymphoid cells group 3 (ILC3) that produce IL-17 and/or IL-22. These cytokines induce secretion of antimicrobial peptides (AMPs) from Paneth cells and intestinal epithelial cells. AMPs shape the microbiota and are also involved in colonization resistance against pathogens