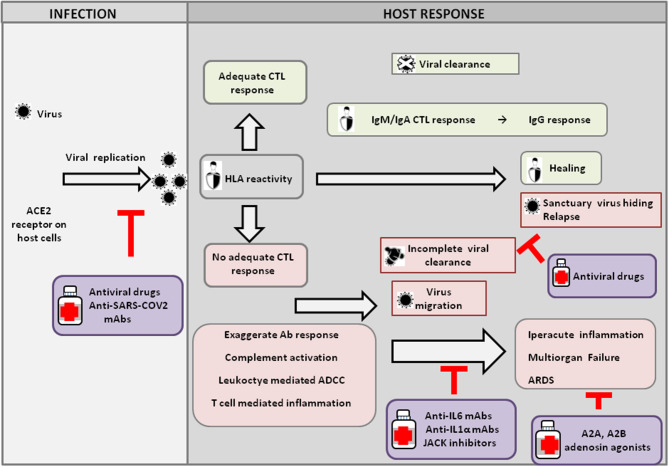
Figure 1.
Host response and possible outcomes of SARS-CoV-2 infection. Viral infection seems to occur mainly upon SARS-CoV2 engagement of angiotensin I converting enzyme 2 (ACE2), which acts as a functional receptor for the spike glycoprotein of the coronavirus. The HLA genetic system acts as a key player in determining the anti-viral immune response. In particular, the ability of HLA to trigger an adequate cytotoxic T-lymphocyte (CTL) response will result in viral clearance and host healing, along with the development of the IgM, IgA, and IgG humoral response. Conversely, an inadequate HLA asset will result in an inefficient CTL response and, consequently, incomplete viral clearance. In this context, various factors underlie increased COVID-19 severity, including an exaggerated Ab response, complement activation, leukocyte-mediated antibody-dependent cell-mediated cytotoxicity (ADCC), and T-cell-mediated inflammation, as discussed in the text. Without a protective immune response, the virus is able to migrate, propagating into other ACE2-expressing tissues, while the damaged lung cells induce high inflammation, triggering the cytokine storm that represents the main cause of the acute respiratory distress syndrome (ARDS) and subsequent multiorgan failure. Incomplete viral clearance can also lead to virus hiding in sanctuary sites and patient relapse with symptoms arising in new districts. In the purple boxes, different therapeutic approaches aimed at targeting either the virus or endogenous host players are represented.