Abstract
Introduction
There is limited evidence about the association between calcium and phosphate levels and mortality stratified by intact parathyroid hormone (iPTH) level.
Methods
We investigated whether differences in iPTH level affect the relationship between calcium and phosphate levels and all-cause mortality in hemodialysis patients with secondary hyperparathyroidism (SHPT). Calcium and phosphate levels were categorized as low (< 8.5 mg/dL, < 4.0 mg/dL), medium (≥ 8.5–< 9.5 mg/dL, ≥ 4.0–< 7.0 mg/dL), and high (≥ 9.5 mg/dL, ≥ 7.0 mg/dL), respectively. iPTH levels were grouped into < 300 or ≥ 300 pg/mL. Adjusted incidence rate ratios (aIRRs) were analyzed by weighted Poisson regression.
Results
For calcium, patients with higher iPTH (≥ 300 pg/mL) had significantly higher all-cause mortality rates in the high than in the medium category (aIRR 1.99, 95% confidence interval [CI] 1.16–3.42), and tended to have a higher mortality rate in the low category (aIRR 2.04, 95% CI 0.94–4.42). Patients with lower iPTH (< 300 pg/mL) had higher mortality rates in the high than in the medium category (aIRR 1.65, 95% CI 1.39–1.96). For phosphate, the mortality rate was significantly higher in the high than in the medium category in patients with higher and lower iPTH (aIRR 3.23, 95% CI 1.63–6.39 for iPTH ≥ 300 pg/mL; aIRR 1.58, 95% CI 1.06–2.36 for iPTH < 300 pg/mL).
Conclusion
High calcium and phosphate levels were associated with increased risk of mortality irrespective of iPTH level.
Electronic supplementary material
The online version of this article (10.1007/s10157-020-01879-8) contains supplementary material, which is available to authorized users.
Keywords: Calcium, Chronic kidney disease–mineral and bone disorder, Hemodialysis, Parathyroid hormone, Phosphate, Mortality
Introduction
Chronic kidney disease (CKD) may involve secondary hyperparathyroidism (SHPT) characterized mainly by abnormal metabolism of calcium and phosphate, and increased production and secretion of parathyroid hormone (PTH). The resulting osteoporosis and blood vessel calcification due to the abnormal mineral metabolism influences the onset of cardiovascular events that worsen the patient’s prognosis [1]. In the management of abnormal mineral metabolism, patients are treated according to target control values of phosphate, calcium, and PTH levels [2, 3].
Associations between elevated phosphate and calcium levels and increased mortality rates have been shown in the Worldwide Dialysis Outcomes and Practice Pattern Study (DOPPS) in hemodialysis patients [4] and in a study by Block et al. that reported real-world findings in the United States [5]. Similar findings were reported from Japanese studies in dialysis patients with SHPT (the Mineral and Bone Disorder Outcomes Study for Japanese CKD Stage 5D Patients [MBD-5D]) [6] and an exhaustive survey in maintenance hemodialysis patients [7]. In addition, Tentori et al. evaluated the relationships between calcium and phosphate levels and mortality rates in a population with an intact PTH (iPTH) level of ≥ 300 pg/mL and < 300 pg/mL, reporting that in the subpopulation with iPTH ≥ 300 pg/mL, the mortality rate was higher in patients with high calcium levels, suggesting a U-shaped relationship between phosphate level and mortality rate, and that in the subpopulation with iPTH < 300 pg/mL, the mortality rate tended to be higher in patients with low calcium levels [4]. However, the relationships between phosphate and calcium levels and mortality rates depending on SHPT severity have not been thoroughly assessed in Japan.
We therefore aimed to explore any associations between SHPT severity and calcium and phosphate levels and mortality rates with iPTH as an index using a marginal structural model in the MBD-5D study, a prospective observational study in SHPT patients on maintenance hemodialysis.
Methods
MBD-5D study
The MBD-5D study was a multicenter, prospective, case-cohort study following maintenance hemodialysis patients with SHPT [8]. A total of 8229 patients were registered from 86 facilities in Japan, and followed for 3 years (from January 2008 to December 2010). Data for prescribed drugs and mineral and bone disorder (MBD)-related serum markers (serum calcium, phosphate, and iPTH) were recorded every 3 months and data for other time-dependent variables were recorded every 6 months.
Of the total number of patients in the cohort, 40% were randomly selected into the subcohort (n = 3276), for which data were collected prospectively. Data from patients who died and had not been included in the subcohort were collected retrospectively. The study protocol was approved by the central ethics committee at Kobe University’s School of Medicine (No. 754). Informed consent was not mandatory according to the ethical guidelines for epidemiological research in Japan. The study is registered at ClinicalTrials.gov (NCT00995163).
Participants
The target population of the MBD-5D study was patients with SHPT who had received maintenance hemodialysis. Patients with SHPT were defined as those who had iPTH ≥ 180 pg/mL (according to the Japanese guidelines at that time [3], such patients needed treatment to lower iPTH levels), or those who were treated with intravenous calcitriol or maxacalcitol and/or an oral vitamin D receptor activator (VDRA; falecalcitriol). All the eligible patients receiving maintenance hemodialysis at one of the participating facilities as of January 2008 were enrolled. Patients who had been receiving hemodialysis for less than 3 months were excluded. Although the study protocol did not specify the management of patients, we assumed that these patients had been managed according to Japanese guidelines.
Exposures, outcomes, and covariates
The primary outcome was all-cause mortality. The secondary outcome was cardiovascular mortality, which was defined as death due to cerebrovascular disease, heart failure, myocardial infarction, sudden death, arrhythmia, aortic disease, or other cardiovascular disease. The MBD-related serum markers were considered time-dependent variables, which were updated every 3 months. Serum calcium and phosphate levels were categorized into 3 groups: low (< 8.5 mg/dL [< 2.12 mmol/L], < 4.0 mg/dL [< 1.29 mmol/L]), medium (≥ 8.5–< 9.5 mg/dL [≥ 2.12–< 2.37 mmol/L], ≥ 4.0–< 7.0 mg/dL [≥ 1.29–< 2.26 mmol/L]), and high (≥ 9.5 mg/dL [≥ 2.37 mmol/L], ≥ 7.0 mg/dL [≥ 2.26 mmol/L]), respectively. The medium range for serum calcium and serum phosphate was defined based on the positive stratification for mortality in the previous report.6 Serum iPTH levels were grouped into < 300 or ≥ 300 pg/mL [9]. In this study, we examined the effect of serum calcium or serum phosphate on clinical outcomes, depending on the level of iPTH. Therefore, serum calcium and phosphate were categorized into 6 classes (3 levels of serum calcium or phosphate by 2 levels of iPTH).
When albumin levels were < 4.0 g/dL, serum calcium levels were corrected for albumin concentration by the modified Payne method [10] (which is commonly used in Japan): corrected calcium = calcium + (4.0 − albumin). Serum whole PTH levels measured with a third-generation PTH assay were converted to iPTH levels: iPTH = whole PTH × 1.7 [3].
Covariates included fixed patients’ characteristics (age, sex, primary kidney disease, diabetes, dialysis duration, cardiovascular disease, pulmonary disease, liver disease, malignancy, and history of parathyroidectomy) and time-dependent variables that were updated at each visit (MBD-related drugs coded as follows: VDRAs, oral/intravenous/none; phosphate binders, calcium carbonate/non–calcium-containing drugs/both/none; and calcimimetics, yes/no], serum albumin level, hemoglobin level, body mass index, Kt/V, and dialysate calcium concentration). In Japan, calcimimetics (cinacalcet hydrochloride) became available in January 2008.
Statistical analysis
To estimate the average causal effect of MBD markers on mortality, we used marginal structural models [11, 12] to account for time-dependent confounders such as MBD treatments, by weighting with the inverse of the probability of having a history of a pattern of identifiable MBD markers.
For each 3-month period ending at visit t, the incidence of a clinical outcome was modeled based on the patterns of MBD markers in the previous 3 months (visit t − 1). The probability of having a pattern of identifiable MBD markers was calculated using pooled multinomial logistic regression models, in which the dependent variable was the pattern of MBD marker at visit t − 1 and the independent variables were time-dependent covariates at visit t − 2 and the baseline covariates mentioned above. Stabilized weights, in which the patterns of MBD markers at visit t − 2 were used as the numerator, were computed.
We used weighted Poisson regression to estimate adjusted incidence rates (aIRs) and adjusted incidence rate ratios (aIRRs). The weights were calculated as a cumulative product of the stabilized weights. Data were truncated if the cumulative stabilized weight was greater than 100 or less than 0.01. Periods of follow-up of cases in the subcohort before death and subcohort controls were further weighted by the inverse of the sampling fraction (1/0.4 = 2.5), while periods of follow-up in which the outcome events occurred were not (because the sampling fraction of cases was 1.0) [13, 14]. Within-patient correlation was assessed by using robust variances with an independent working correlation matrix. As sensitivity analysis, serum iPTH levels were grouped into < 240 or ≥ 240 pg/mL (sensitivity analysis 1 for serum calcium, and sensitivity analysis 3 for serum phosphate), serum calcium levels were categorized into 3 groups: low (< 8.4 mg/dL [< 2.10 mmol/L]), medium (≥ 8.4–< 10.0 mg/dL [≥ 2.10–< 2.49 mmol/L]), and high (≥ 10.0 mg/dL [≥ 2.49 mmol/L]) (sensitivity analysis 2), and serum phosphate levels were categorized into 3 groups: low (< 3.5 mg/dL [< 1.13 mmol/L]), medium (≥ 3.5–< 6.0 mg/dL [≥ 1.13–< 1.94 mmol/L]), and high (≥ 6.0 mg/dL [≥ 1.94 mmol/L]) (sensitivity analysis 4).
The results were summarized as point estimates and 95% confidence intervals (95% CIs) with P values. P values for interaction were also computed. SAS version 9.4 (SAS Institute Inc., Cary, NC) was used for all analyses.
Results
Baseline characteristics and outcomes
Table 1 shows the characteristics of the study patients summarized by visits per 3 months. Median age was 62 years and 62% of the patients were male. Median duration of dialysis was 10.2 years (interquartile range 3.8–14.4). The underlying disease was chronic glomerulonephritis in 45% of patients. Most patients had been prescribed medications to treat MBD: intravenous VDRAs in 53% of the total visits and phosphate binders in 86%. Calcimimetics, which were not available in Japan at the beginning of this study, were prescribed in 20% of visits. The all-cause and cardiovascular disease-related mortality rate was 4.9 and 1.8 per 100 person-years, respectively.
Table 1.
Baseline patient characteristics of the study population
| Characteristic | Value |
|---|---|
| Sex, male | 62% |
| Age (years) | 62 (55–71) |
| Dialysis duration (years) | 10.2 (3.8–14.4) |
| Body mass index (kg/m2) | 21.2 (18.8–23.1) |
| Serum albumin (g/dL) | 3.7 (3.5–3.9) |
| Hemoglobin (g/dL) | 10.5 (9.8–11.2) |
| Intact parathyroid hormone (pg/mL) | 206 (124–320) |
| Calcium (mg/dL) | 9.5 (9.0–10.0) |
| Phosphate (mg/dL) | 5.4 (4.5–6.2) |
| Cause of end-stage renal disease | |
| Glomerulonephritis | 45% |
| Diabetic nephropathy | 25% |
| Comorbidities | |
| Cardiovascular disease | 61% |
| Malignancy | 5% |
| History of parathyroidectomy | 6% |
| Vitamin D receptor activators | |
| Intravenous | 53% |
| Oral | 30% |
| None | 17% |
| Phosphate binders | |
| Calcium-based | 40% |
| Non-calcium-based | 20% |
| Both | 26% |
| None | 14% |
| Cinacalcet | 20% |
Data are expressed as median (interquartile range) or proportion
According to the characteristics of subgroups by iPTH and calcium (Table S1), patients with higher iPTH levels tended to have been on dialysis for longer and prescribed intravenous VDRA more frequently. These trends became more apparent as serum calcium level increased. When the subgroups were analyzed by iPTH and phosphate, those patients with higher serum phosphate levels were more likely to be younger and receiving a VDRA (Table S2).
Mortality and serum calcium levels stratified by serum iPTH levels
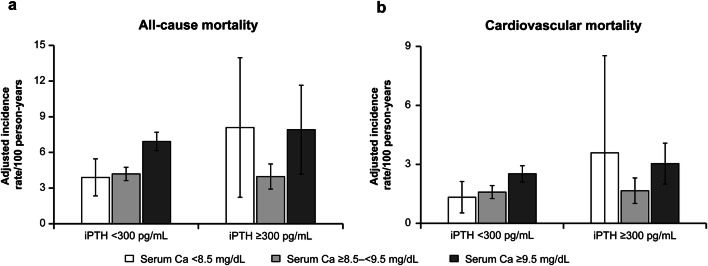
Among the group with iPTH < 300 pg/mL, all-cause mortality rates in patients with high calcium levels (≥ 9.5 mg/dL) were higher than those in patients with medium levels (aIRR 1.65, 95% CI 1.39–1.96, P < 0.001) (Fig. 1, Tables 2, S3). However, among those with iPTH ≥ 300 pg/mL, we observed a U-shaped pattern in the aIRs. The interaction effect was marginally insignificant (P = 0.119). The aIRs increased not only among patients with high serum calcium levels but also among those with lower levels (Fig. 1). Similar trends were also observed regarding cardiovascular disease-related mortality, although the CIs were wider due to the small number of events (Fig. 1, Tables 2, S3).
Fig. 1.
Adjusted incidence rate for all-cause mortality (a) and cardiovascular mortality (b) stratified by levels of serum intact parathyroid hormone and serum calcium. Ca calcium, iPTH intact parathyroid hormone. Incidence rate ratios were adjusted for patients’ characteristics (age, sex, primary kidney disease, diabetes, dialysis duration, cardiovascular disease, pulmonary disease, liver disease, malignancy, and history of parathyroidectomy) and time-dependent variables (vitamin D receptor activators, phosphate binders, calcimimetics, serum albumin level, hemoglobin level, body mass index, Kt/V, and dialysate calcium concentration)
Table 2.
Adjusted incidence rate ratios for all-cause and cardiovascular mortality for patients with serum calcium levels stratified by serum intact parathyroid hormone levels
| Outcomes | Serum calcium (mg/dL) | aIRR (95% CI) | Interaction | |
|---|---|---|---|---|
| iPTH < 300 pg/mL | iPTH ≥ 300 pg/mL | |||
| All-cause mortality | < 8.5 | 0.93 (0.61–1.41) | 2.04 (0.94–4.42) | P = 0.119 |
| P = 0.740 | P = 0.070 | |||
| ≥ 8.5–< 9.5 | Ref | Ref | ||
| ≥ 9.5 | 1.65 (1.39–1.96) | 1.99 (1.16–3.42) | ||
| P < 0.001 | P = 0.012 | |||
| Cardiovascular mortality | < 8.5 | 0.84 (0.44–1.57) | 2.16 (0.52–9.03) | P = 0.366 |
| P = 0.580 | P = 0.293 | |||
| ≥ 8.5–< 9.5 | Ref | Ref | ||
| ≥ 9.5 | 1.58 (1.22–2.06) | 1.83 (1.09–3.07) | ||
| P < 0.006 | P = 0.0230 | |||
Incidence rate ratios were adjusted for patients’ characteristics (age, sex, primary kidney disease, diabetes, dialysis duration, cardiovascular disease, pulmonary disease, liver disease, malignancy, and history of parathyroidectomy) and time-dependent variables (vitamin D receptor activators, phosphate binders, calcimimetics, serum albumin level, hemoglobin level, body mass index, Kt/V, and dialysate calcium concentration)
aIRR adjusted incidence rate ratio, CI confidence interval, iPTH intact parathyroid hormone, ref reference
In the sensitivity analysis, all-cause mortality rate in patients with high calcium levels (≥ 9.5 mg/dL) were higher than those in patients with medium levels in each iPTH level (cutoff value of iPTH 240 pg/mL), and the interaction effect was significant (P = 0.085) (Fig. S1, Table S4). Among the group with iPTH < 300 pg/mL, all-cause mortality rate in patients with low serum calcium level (< 8.4 mg/dL) and high serum calcium level (≥ 10.0 mg/dL) were higher than those in patients with medium levels, and the interaction effect was significant (P = 0.041) (Fig. S2, Table S5).
Mortality and serum phosphate levels stratified by serum iPTH levels
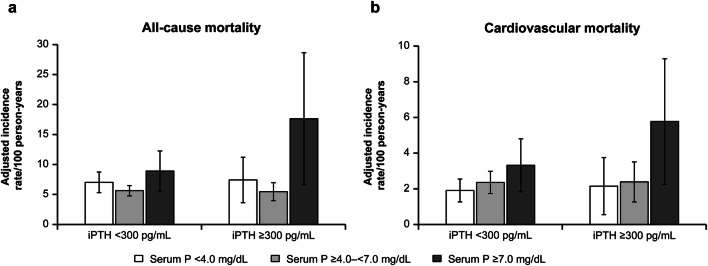
The aIRs were higher among patients with high serum phosphate levels (Fig. 2). This pattern was more apparent when serum iPTH level was higher: the aIRR (95% CI) among patients with serum phosphate ≥ 7.0 mg/dL was 1.58 (1.06–2.36) when serum iPTH was < 300 pg/mL, and 3.23 (1.63–6.39) when serum iPTH was ≥ 300 pg/mL (Fig. 2, Tables 3, S6). The interaction effect was not statistically significant. The aIRs of cardiovascular disease-related mortality showed a similar trend (Fig. 2, Table S6). There was no significant interaction effect on clinical outcomes between serum iPTH and serum phosphate levels (Table 3).
Fig. 2.
Adjusted incidence rate for all-cause mortality (a) and cardiovascular mortality (b) stratified by levels of serum intact parathyroid hormone and serum phosphate. iPTH intact parathyroid hormone, P phosphate. Incidence rate ratios were adjusted for patients’ characteristics (age, sex, primary kidney disease, diabetes, dialysis duration, cardiovascular disease, pulmonary disease, liver disease, malignancy, and history of parathyroidectomy) and time-dependent variables (vitamin D receptor activators, phosphate binders, calcimimetics, serum albumin level, hemoglobin level, body mass index, Kt/V, and dialysate calcium concentration)
Table 3.
Adjusted incidence rate ratios for all-cause and cardiovascular mortality for patients with serum phosphate levels stratified by serum intact parathyroid hormone levels
| Outcomes | Serum phosphate (mg/dL) | aIRR (95% CI) | Interaction | |
|---|---|---|---|---|
| iPTH < 300 pg/mL | iPTH ≥ 300 pg/mL | |||
| All-cause mortality | < 4.0 | 1.25 (0.94–1.66) | 1.36 (0.76–2.42) | P = 0.207 |
| P = 0.129 | P = 0.298 | |||
| ≥ 4.0–< 7.0 | Ref | Ref | ||
| ≥ 7.0 | 1.58 (1.06–2.36) | 3.23 (1.63–6.39) | ||
| P = 0.026 | P < 0.001 | |||
| Cardiovascular mortality | < 4.0 | 0.81 (0.53–1.24) | 0.90 (0.37–2.17) | P = 0.366 |
| P = 0.329 | P = 0.815 | |||
| ≥ 4.0–< 7.0 | Ref | Ref | ||
| ≥ 7.0 | 1.41 (0.84–2.36) | 2.41 (1.11–5.21) | ||
| P = 0.192 | P = 0.025 | |||
aIRR adjusted incidence rate ratio, CI confidence interval, iPTH intact parathyroid hormone, ref reference
Incidence rate ratios were adjusted for patients’ characteristics (age, sex, primary kidney disease, diabetes, dialysis duration, cardiovascular disease, pulmonary disease, liver disease, malignancy, and history of parathyroidectomy) and time-dependent variables (vitamin D receptor activators, phosphate binders, calcimimetics, serum albumin level, hemoglobin level, body mass index, Kt/V, and dialysate calcium concentration)
In the sensitivity analysis, all-cause mortality rate and cardiovascular morality rate in patients with high phosphate levels (≥ 6.0 mg/dL) were consistently higher than those in patients with medium levels in each iPTH level (cutoff value of iPTH 240 pg/mL) (Fig. S3, Table S7). Among the group with iPTH < 300 pg/mL, all-cause mortality rate in patients with high serum phosphate level (≥ 6.0 mg/dL) were attenuated (Fig. S4, Table S8).
Discussion
This analysis showed that in maintenance hemodialysis patients with SHPT, severely affected patients, with iPTH ≥ 300 pg/mL and with high or low calcium levels (U shape), tended to have higher mortality rates, whereas in mildly affected patients with iPTH < 300 pg/mL, the mortality rates were higher only in patients with high calcium levels. Analysis by phosphate level showed that both severely and mildly affected patients with high phosphate levels had higher mortality rates; however, no significant difference was found with low phosphate levels.
With regard to the relationship between calcium levels and prognosis in hemodialysis patients, high calcium levels have consistently been shown to be associated with increased mortality rates [4–7]. Reports focusing on the relationship between calcium levels and prognosis depending on PTH level include those from the WW-DOPPS and United States Renal Data System (USRDS) studies. The WW-DOPPS study reported that patients with either high or low calcium levels had high mortality rates, both in the subpopulation with iPTH ≥ 300 pg/mL and that with iPTH < 300 pg/mL [4]. A study by Block et al. using the USRDS assessed the relationship between calcium levels and mortality rates or combined events of death and cardiovascular hospitalization by iPTH level, showing that the risk increased with high calcium levels (≥ 10 mg/dL) compared with corrected calcium levels in the control target range (8.4–10.0 mg/dL) at all iPTH levels, but not showing any change in the risk with low calcium levels (< 8.4 mg/dL) [15].
In our study, the risk of death increased significantly with high calcium levels (≥ 9.5 mg/dL) at all iPTH levels, and tended to increase with low calcium levels (< 8.5 mg/dL) in the iPTH ≥ 300 pg/mL stratum, but not in the < 300 pg/mL stratum. In the subpopulation with calcium levels < 8.5 mg/dL, patients with iPTH ≥ 300 pg/mL compared with those with iPTH < 300 pg/mL were characterized by shorter duration of hemodialysis, a higher proportion of untreated cases of VDRA, a higher male:female ratio, and a higher incidence of diabetic nephropathy. The aIRs for all-cause mortality and cardiovascular mortality in the subpopulation with iPTH ≥ 300 pg/mL and serum calcium < 8.5 mg/dL were more than double those in the subpopulation with iPTH < 300 pg/mL and serum calcium level < 8.5 mg/dL (Table S1). The poor prognosis for patients with iPTH ≥ 300 pg/mL and serum calcium < 8.5 mg/dL is attributable to any possible unmeasured confounding factors associated with the poor prognosis, as well as to the limitations on cinacalcet prescriptions and the inability to use VDRA optimally. Hypocalcemia may have strongly affected the worse prognosis in SHPT patients with iPTH ≥ 300 pg/mL and serum calcium < 8.5 mg/dL. In these patients, it seems necessary to use a calcimimetic and VDRA in combination in order to control mineral parameters appropriately.
With regard to the relationship between phosphate levels and prognosis in hemodialysis patients, this analysis, in line with previous studies [4–7], demonstrated increased mortality and cardiovascular deaths due to high phosphate levels. With regard to the relationship between low phosphate levels and mortality, an exhaustive survey in Japan7 showed increased risk of death with low phosphate levels (< 3.5 mg/dL), whereas a study by Block et al. [5] and a report by Fukagawa et al. from the MBD-5D study [6] found no increased mortality rates due to low phosphate levels. In our study, the risk of death did not change with low phosphate levels (< 4.0 mg/dL) in either of the iPTH strata (≥ 300 pg/mL and < 300 pg/mL). The risks with low phosphate levels might be attenuated by multi-adjusted factors such as undernutrition and frailty, which patients with low phosphate levels have.
This study has several strengths. First, the MBD-5D study was performed as a prospective case-cohort study, which enabled detailed and repeated data collection with few missing data and powerful outcome evaluations avoiding systematic biases. Second, participants of this study were restricted to hemodialysis patients with SHPT, who were generally at risk of abnormal MBD parameters. Therefore, the results of this study can be applied to patients requiring treatment for CKD-MBD.
The study has several limitations. First, it is not possible to measure unknown confounding factors. Second, it is unknown whether the causes of deviation of calcium and phosphate levels from the medium level categories are due to the natural disease course, medication, or other reasons; therefore, it is unclear whether the outcome varies depending on the reason for the parameter deviation. Third, in the study, we collected data on MBD parameters and MBD treatment every 3 months, and the changes that might occur during the 3-month periods were unknown; the influence of any such changes on outcomes therefore remains unknown. Fourth, the duration of observational periods and number of outcomes of each subgroup were not sufficient to analyze the effect modifications. Therefore, further study is required to confirm our results. Fifth, we performed the time-dependent analyses for 3-month intervals to evaluate the relationship between MBD parameters and mortality, these analyses might not predict the longer-term outcomes adequately.
Conclusion
In patients with SHPT on hemodialysis, high calcium and phosphate levels were found to be associated with increased risk of death irrespective of the iPTH level.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank the MBD-5D study advisory investigators, Masashi Suzuki (Shinrakuen Hospital), Yoshindo Kawaguchi (Shiomidai Hospital), Akira Saito (Shonan Tobu Sougo Hospital), Yoshiki Nishizawa (Osaka City University Graduate School of Medicine), Yusuke Tsukamoto (Itabashi Chuo Medical Center), Satoshi Kurihara (Tsukinomori Clinic), Takashi Akiba (Tokyo Women’s Medical University), Eriko Kinugasa (Showa University Northern Yokohama Hospital), Yuzo Watanabe (Kasugai Municipal Hospital), Yoshihiro Tominaga (Nagoya Daini Red Cross Hospital), Takashi Shigematsu (Wakayama Medical University), Masaaki Inaba (Osaka City University Graduate School of Medicine), Jun Minakuchi (Kawashima Hospital), Hideki Hirakata (Fukuoka Red Cross Hospital), Keitaro Yokoyama (Jikei University School of Medicine), Naoki Kimata (Tokyo Women’s Medical University), Fumihiko Koiwa (Showa University Fujigaoka Hospital), Ryoichi Ando (Musashino Red Cross Hospital), Junichiro J. Kazama (Niigata University), Takatoshi Kakuta (Tokai University School of Medicine), Hirotaka Komaba (Tokai University School of Medicine), Daijo Inaguma (Nagoya Daini Red Cross Hospital), Eiji Ishimura (Osaka City University Graduate School of Medicine), Hideki Tahara (Osaka City University Graduate School of Medicine), Kazuhiko Tsuruya (Kyushu University), Akira Fujimori (Konan Hospital), and Ryo Kido (Inagi Municipal Hospital).
The following investigators also participated in this study: Nobuo Hashimoto (H N MEDIC), Mari Ishida (Kitasaito Hospital), Toshiyuki Date (Date Clinic), Kiyotaka Yabuki (Yabuki Hospital), Hideki Tanida (Tendo Onsen Yabuki Clinic), Fumitoshi Yamauchi (San-ai Hospital), Mikihiko Fujishima (Yahaba Clinic), Tomohito Matsunaga (Eijinkai Hospital), Jun Urae (Ishinomaki Clinic), Hiroshi Kawaguchi (Iwaki Urological Hospital), Ikuo Takahashi (Kisen Hospital), Yoshiko Tanaka (Shinjuku Ishikawa Clinic), Hideo Kobayashi (Suda Clinic), Maki Takahashi (Suda Naika Clinic), Tatsuya Nonaka (Seishokai Memorial Hospital), Hideto Emoto (Tokai Hospital), Kyosuke Nishio (Shinkoiwa Clinic), Atsushi Hayama (Moriyama Rehabilitation Hospital), Toshio Shinoda (Kawakita General Hospital Dialysis Center), Takashi Kono (Mihama Narita Clinic), Takahiro Mochizuki (Kameda Medical Center), Yasuo Kimura (Shin-kashiwa Clinic), Noriyoshi Murotani (Chiba Social Insurance Hospital), Satoshi Yamaguchi (Asahi Hospital), Taichi Nakanishi (Kurihama Clinic), Kiyoshi Ozawa (Yokosuka Clinic), Takashi Nagaoka (Sagamihara Clinic), Takao Suga (Bousei Hiratsuka Clinic), Masakazu Suda (Suda Medical Clinic), Yoshikazu Goto (Saiyu Soka Hospital), Michio Kuwahara (Shuwa General Hospital Hemodialysis Clinic), Hiromi Shimoyama (Yuai Clinic), Kimihiko Matsuyama (Misato Kenwa Clinic), Kazue Ueki (Toho Hospital), Kyoko Ito (Heisei Hidaka Clinic), Katsuhiko Miyamoto (Seseragi Hospital), Takashi Ishizu (Tukuba Central Hospital), Shuichi Kikuchi (Ohba Renal Clinic), Masaki Kobayashi (Tokyo Medical University Ibaraki Medical Center), Mitsuyoshi Furuhashi (Maruyama Hospital), Masanori Wakabayashi (Bousei Dai-ichi Clinic), Kazuyoshi Nakamura (Fujidaiichi Clinic), Hirotake Kasuga (Kaikoukai Central Clinic), Itsuo Yokoyama (Nagoya Memorial Foundation Narumi Clinic), Chikao Yamazaki (Masuko Clinic SUBARU), Kijun Nagata (Sawada Hospital), Yasumasa Kawade (Suzuka Kidney Clinic), Toshiaki Kawanaka (Ishikiriseiki Hospital), Yoshihiro Tsujimoto (Inoue Hospital), Mikio Okamura (Ohno Memorial Hospital), Shigeki Okada (Okada Clinic), Senji Okuno (Kidney Center Shirasagi Clinic), Harumi Nagayama (Nagayama Hemodialysis Clinic), Shuji Okazaki (Nagayama Hospital), Yoshinori Tone (Fujii Clinic), Ibuki Yajima (Ibuki Clinic), Kouji Shibuya (Sumiyoshigawa Hospital), Kunihiko Yoshiya (Hara Genitourinary Hospital), Morihiro Kondou (Otowa Kinen Hospital), Satoru Yamazaki (Tojinkai Hospital), Ryoichi Miyazaki (Fujita Memorial Hospital), Katsuhiko Arimoto (Shigei Medical Research Hospital), Misaki Moriishi (Nakajima Tsuchiya Clinic), Takahito Nasu (Tokuyama Central Hospital), Seiichi Obayashi (Kinashi Obayashi Hospital), Yuzuru Sato (Sato Junkankika Naika), Takao Tanaka (Ohji Hospital), Hidetoshi Nakamura (Kokura Daiichi Hospital), Nobuhiko Koga (Shin-Koga Clinic), Harumichi Higashi (St. Mary’s Hospital), Kougi Yuu (Takahashi Naika Clinic), Asako Kitamura (Chikuho Social Insurance Hospital), Tomoji Matsumae (Murakami Memorial Hospital), Katsushige Abe (Jinikai Hospital), Masahiro Kawatomi (Kawatomi Internal Medicine Clinic), Chisa Nogami (Kumamoto Urological Hospital), Etsuo Yoshidome (Ikeda Hospital), Shinyu Miyagi (Okinawa Daiichi Hospital), Satoshi Nakazato (Chibana Clinic), Yoshiki Shiohira (Tomishiro Central Hospital), and Kiyoyuki Tokuyama (Tokuyama Clinic).
Funding
The MBD-5D study was funded by Kyowa Kirin Co., Ltd.
Compliance with ethical standards
Conflict of interest
SA, YE, TN, and MW are employees of Kyowa Kirin Co., Ltd. (KKC). KY has received consulting fees from Torii Pharmaceutical, and lecture fees from KKC, Torii Pharmaceutical, and Ono Pharmaceutical. CM and YO do not have any conflicts of interest to declare. S. Fukuma has acted as a scientific advisor for KKC. MF has received consulting fees from KKC and Ono Pharmaceutical; lecture fees from KKC, Bayer, Torii Pharmaceutical, and Ono Pharmaceutical; and grants from KKC and Bayer. S. Fukuhara has acted as a scientific advisor for and has received grants from KKC. TA has received consulting fees from KKC, Astellas Pharma, Bayer, Fuso Pharmaceutical, Japan Tobacco, Ono Pharmaceutical, Sanwa Chemical, Otsuka, GSK and NIPRO, and lecture fees from KKC, Chugai Pharmaceutical, Bayer, Kissei Pharmaceutical, Torii Pharmaceutical, and Ono Pharmaceutical.
Ethical approval
The study protocol was approved by the central ethics committee at Kobe University's School of Medicine (No. 754).
Informed consent
Informed consent was not mandatory according to the ethical guidelines for epidemiological research in Japan. The study is registered at ClinicalTrials.gov (NCT00995163).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shinji Asada and Keitaro Yokoyama have contributed equally to this work.
References
- 1.Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: improving global outcomes (KDIGO) Kidney Int. 2006;69:1945–1953. doi: 10.1038/sj.ki.5000414. [DOI] [PubMed] [Google Scholar]
- 2.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Working Group. KDIGO clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD) Kidney Int Suppl. 2017;2017(7):1–59. doi: 10.1016/j.kisu.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guideline Working Group, Japanese Society for Dialysis Therapy Clinical practice guideline for the management of secondary hyperparathyroidism in chronic dialysis patients. Ther Apher Dial. 2008;12:514–525. doi: 10.1111/j.1744-9987.2008.00648.x. [DOI] [PubMed] [Google Scholar]
- 4.Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2008;52:519–530. doi: 10.1053/j.ajkd.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–2218. doi: 10.1097/01.ASN.0000133041.27682.A2. [DOI] [PubMed] [Google Scholar]
- 6.Fukagawa M, Kido R, Komaba H, Onishi Y, Yamaguchi T, Hasegawa T, et al. Abnormal mineral metabolism and mortality in hemodialysis patients with secondary hyperparathyroidism: evidence from marginal structural models used to adjust for time-dependent confounding. Am J Kidney Dis. 2014;63:979–987. doi: 10.1053/j.ajkd.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Taniguchi M, Fukagawa M, Fujii N, Hamano T, Shoji T, Yokoyama K, et al. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Ther Apher Dial. 2013;17:221–228. doi: 10.1111/1744-9987.12030. [DOI] [PubMed] [Google Scholar]
- 8.Fukuhara S, Akizawa T, Fukagawa M, Onishi Y, Yamaguchi T, Hasegawa T, et al. Mineral and bone disorders outcomes study for Japanese chronic kidney disease stage 5D patients: rationale and study design. Ther Apher Dial. 2011;15:169–175. doi: 10.1111/j.1744-9987.2010.00906.x. [DOI] [PubMed] [Google Scholar]
- 9.Chertow GM, Pupim LB, Block GA, Correa-Rotter R, Drueke TB, Floege J, et al. Evaluation of cinacalcet therapy to lower cardiovascular events (EVOLVE): rationale and design overview. Clin J Am Soc Nephrol. 2007;2:898–905. doi: 10.2215/CJN.04381206. [DOI] [PubMed] [Google Scholar]
- 10.Payne RB, Little AJ, Williams RB, Milner JR. Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J. 1973;4:643–646. doi: 10.1136/bmj.4.5893.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–570. doi: 10.1097/00001648-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Bradbury BD, Brookhart MA, Winkelmayer WC, Critchlow CW, Kilpatrick RD, Joffe MM, et al. Evolving statistical methods to facilitate evaluation of the causal association between erythropoiesis-stimulating agent dose and mortality in nonexperimental research: strengths and limitations. Am J Kidney Dis. 2009;54:554–560. doi: 10.1053/j.ajkd.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 13.Barlow WE, Ichikawa L, Rosner D, Izumi S. Analysis of case-cohort designs. J Clin Epidemiol. 1999;52:1165–1172. doi: 10.1016/S0895-4356(99)00102-X. [DOI] [PubMed] [Google Scholar]
- 14.Cole SR, Hudgens MG, Tien PC, Anastos K, Kingsley L, Chmiel JS, Jacobson LP. Marginal structural models for case-cohort study designs to estimate the association of antiretroviral therapy initiation with incident AIDS or death. Am J Epidemiol. 2012;175:381–390. doi: 10.1093/aje/kwr346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Block GA, Kilpatrick RD, Lowe KA, Wang W, Danese MD. CKD-mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin J Am Soc Nephrol. 2013;8:2132–2140. doi: 10.2215/CJN.04260413. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.