Abstract
The pandemic of novel Coronavirus (SARS-CoV-2) is currently spreading rapidly across the United States. We provide a comprehensive overview of COVID-19 epidemiology across the state of Texas, which includes vast rural & vulnerable communities that may be disproportionately impacted by the spread of this new disease. All 254 Texas counties were included in this study. We examined the geographic variation of COVID-19 from March 1 through April 8, 2020 by extracting data on incidence and case fatality from various national and state datasets. We contrasted incidence and case fatality rates by county-level demographic and healthcare resource factors. Counties which are part of metropolitan regions, such as Harris and Dallas, experienced the highest total number of confirmed cases. However, the highest incidence rates per 100,000 population were in found in counties of Donley (353.5), Castro (136.4), Matagorda (114.4) and Galveston (93.4). Among counties with greater than 10 cases, the highest CFR were observed in counties of Comal (10.3%), Hockley (10%), Hood (10%), and Castro (9.1%). Counties with the highest CFR (> 10%) had a higher proportion of non-Hispanic Black residents, adults aged 65 and older, and adults smoking, but lower number of ICU beds per 100,000 population, and number of primary care physicians per 1000 population. Although the urban areas of Texas account for the majority of COVID-19 cases, the higher case-fatality rates and low health care capacity in rural areas need attention.
Keywords: COVID-19, Texas, Geographic distribution, Epidemiology, Incidence and case-fatality rates
Introduction
While the current pandemic of novel coronavirus (SARS-CoV-2) has engulfed the world, the United States is one of the hardest hit countries. With the 428,654 cases till 8th April, the US has seen 14,704 deaths [1]. In the state of Texas, the first case of the COVID-19 was detected on March 5th, 2020, and the first death attributed to COVID-19 was ten days later on March 15th. As of April 8th, there have been 9777 confirmed cases and 189 deaths attributed to COVID-19 [1]. Furthermore, it is predicted that Texas will have about 5,847 (95% CI 4249−7668) deaths attributed to COVID-19 by August 4th 2020 [3].
The month of ‘April 2020’ represents a challenging time in disease prevention and control for the state of Texas, which is expected to experience highest morbidity as well as mortality in last week of April. Public health capacity represents the most critical factor for preventing spread as well as deaths from COVID-19. Understanding the geographic areas with the highest disease burden will allow policy makers, public health professionals, and healthcare providers to appropriately allocate resources and adequately prepare for the disease pandemic. This will also help understand the epidemiology of novel coronavirus. Here, we present the overall incidence of confirmed COVID-19 cases and case-fatality rates in Texas, stratified by counties.
Methods
Study Design and Setting
Using counties as the units of analysis, we examined the geographic variation of COVID-19 in Texas from March 1 through April 8, 2020. We obtained county-level data on COVID-19 confirmed cases and mortality from the Johns Hopkins 2019 Novel Coronavirus Data Repository (https://github.com/CSSEGISandData/COVID-19), [1, 2]. We linked county-level COVID-19 with county-level data on socio-demographic, access to healthcare, and hospital critical care infrastructure factors derived from the 2014 County Health Rankings, 2014 American Community Survey, 2010 Census, and 2017–2019 Centers for Medicare & Medicaid Services hospital reports. This study was considered exempt by Institutional Review Board review because we used publicly available, de-identified secondary data.
Statistical Analysis
We calculated measures of disease morbidity and mortality at the county level: (1) confirmed COVID case incidence rate per 100,000 population through April 8, 2020, and (2) case-fatality rate among confirmed cases. We compared the distributions for county-level characteristics between quintiles of incidence and case fatality rates using Kruskal–Wallis tests. We performed all statistical analysis using SAS version 9.4 and executed all mapping using ArcGIS version 10.5.
Results
Incidence Rates in Texas, Through April 8th 2020
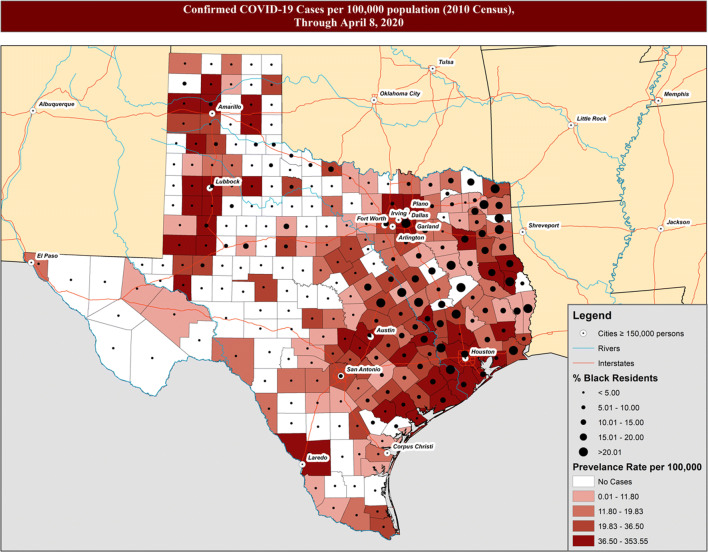
In Fig. 1, we present the incidence of confirmed COVID-19 cases in Texas through the beginning of April, the first month of community spread. There were total of 9777 confirmed cases corresponding to incidence rate (IR) of 38.9 (95% Confidence Interval (CI) 38.1–39.7) per 100,000 population. Harris county experienced the highest total number of confirmed cases with 2341 people testing positive through April 8, 2020, followed by Dallas county reporting 1324 cases. However, among counties with greater than 10 cases, the highest incidence rates were in following four counties: (1) Donley (IR 353.5; 95% CI 188.3–603.8), (2) Castro (IR 136.4; 95% CI 68.1–24.4), (3) Matagorda (IR: 114.4; 95% CI 82.5–154.6), and (4) Galveston (IR 93.4; 95% CI 82.6–105.1).
Fig. 1.
Incidence of confirmed COVID-19 cases per 100,000 population overlaid with percentage of black residents, through April 8, 2020
We compared the distribution of county-level demographics and community resources by quintiles of COVID-19 IRs (Table 1), including counties with no cases, in order to understand similarities or dissimilarities between counties yet to experience spread of the disease. We observed that counties with the highest IR (36.5–353.5 per 100,000 population) had a higher proportion of non-Hispanic Black residents (median: 6.3%; IQR: 3.2–12.1, p value < 0.01), a lower proportion of adults aged 65 and older (13.2%; IQR: 10.1–15.4, p value < 0.01), higher number of ICU beds per 100,000 population (1.1; IQR: 0–2.4, p value < 0.01), lower number of people who could not visit due to cost (proxy for insurance) (18.5; IQR: 14.6–22.1, p value 0.02), a higher unemployment rate (6.0; IQR: 5.3–6.9, p value < 0.01), and a lower proportion of smoking in population (16.9%; IQR: 14.0–21.7, p value < 0.01) as compared to counties with lower IRs.
Table 1.
County-Level Characteristics Comparisons by Quintiles of COVID-19 Incidence Rates, Among Texas Counties through April 8, 2020
| Incidence rate per 100,000 population | 0.00 (No cases) | 0.01–11.80 | 11.80–19.83 | 19.83–36.50 | 36.50–353.55 | p valuea |
|---|---|---|---|---|---|---|
| No. of counties | 87 | 41 | 43 | 41 | 42 | |
| Presented as median (IQR)b | ||||||
| Race | ||||||
| % NH-White | 63.6 (44.2–78.4) | 71.8 (43.9–79.2) | 64.7 (43.4–75.9) | 60.4 (52.3–66.7) | 57.3 (46.2–66.0) | 0.21 |
| % NH-Black | 1.4 (0.6–4.2) | 3.4 (1.2–9.3) | 5.7 (1.8–10.7) | 6.9 (2.3–14.3) | 6.3 (3.2–12.1) | < 0.01 |
| % Hispanic | 30.5 (16.1–51.5) | 20.5 (10.9–48.2) | 18.7 (13.3–50.2) | 24.2 (19.5–33.1) | 30.9 (18.5–44.3) | 0.28 |
| % Female sex | 50.1 (48.2–50.8) | 50.5 (49.3–50.8) | 50.8 (49.9–51.0) | 50.5 (49.2–50.8) | 50.2 (49.3–50.8) | 0.04 |
| % Age 65+ | 17.6 (14.7–22.4) | 16.4 (13.4–19.5) | 15.5 (12.5–19.0) | 13.6 (11.5–17.1) | 13.2 (10.1–15.4) | < 0.01 |
| ICUc beds per 100,000 population | 0 (0–0) | 0 (0–18.1) | 0 (0–22.7) | 0 (0–25.6) | 11.0 (0–24.9) | < 0.01 |
| PCPd per 1,000 population | 2.8 (0–8.4) | 1.2 (0.8–1.7) | 0.8 (0.4–1.5) | 0.6 (0.2–1.5) | 0.7 (0.1–2.5) | 0.08 |
| % Could not visit due to cost | 23.4 (22.9–29) | 22.6 (16.3–25.7) | 22.9 (18.9–26.8) | 17.6 (15.3–21.6) | 18.5 (14.6–22.1) | 0.02 |
| Unemployment rate | 5.3 (4.4–6.6) | 6.4 (5.5–7.7) | 6.8 (6.0–7.7) | 5.8 (5.2–6.5) | 6.0 (5.3–6.9) | < 0.01 |
| % Adult obesity | 29.5 (28.8–30.1) | 29.8 (29.2–31.1) | 29.5 (28.2–32.3) | 29.3 (28.2–31.7) | 29.6 (28.9–30.4) | 0.43 |
| % Adult smoking | 29.4 (21.9–37.7) | 23.1 (20.9–27.7) | 22.5 (17.9–28.2) | 19.1 (16.2–22.0) | 16.9 (14.0–21.7) | < 0.01 |
Among Texas Counties through April 8, 2020
aSignificance determined using Kruskal–Wallis tests, p values < 0.05
bIQR = interquartile range
cICU = intensive care unit, ICU bed tally does not include Veterans Affairs hospitals, which are sure to play a role in treating COVID-19 patients, because VA hospitals do not file cost reports to CMS
dPCP = primary care physicians
Case-Fatality Rates of COVID-19 in Texas, Through April 8th 2020
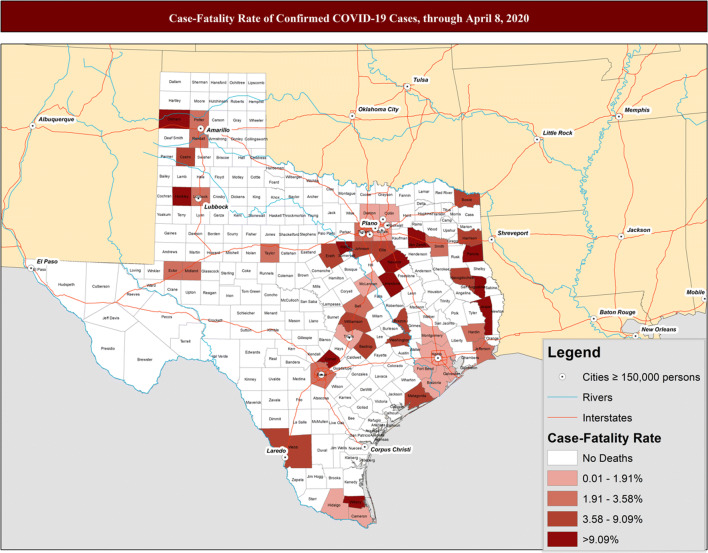
We present the case-fatality rates per county in Fig. 2. Among the 9777 confirmed cases, 189 died (1.9% case fatality rate (CFR); 95% CI 1.7–2.2%) due to complications from COVID-19. With 31 deaths, Harris county experienced the highest fatality, followed by Dallas county reporting 20 deaths. However, both Harris (1.3; 95% CI 0.9–1.9) and Dallas (1.5; 95% CI 0.9–2.3) counties experienced comparatively lower CFR. Among counties with greater than 10 cases, the highest CFR were in: (1) Comal (CFR: 10.3; 95% CI 2.2–27.4), (2) Hockley (CFR: 10; 95% CI 0.3–44.5), (3) Hood (CFR: 10; 95% CI 0.3–44.5), and (4) Castro (CFR: 9.1; 95% CI 0.2–41.2).
Fig. 2.
Case-fatality rates for confirmed COVID-19 cases, through April 8, 2020
We also compared the distribution of county-level demographics and community resources by quintiles of COVID-19 CFRs (Table 2), including counties with no deaths, to understand mortality trends of the disease. We observed that counties with the highest CFR (> 10%) had a higher proportion of non-Hispanic Black residents (median: 3.4%; IQR: 1.7–16.9, p value < 0.01), a higher proportion of adults aged 65 and older (16.6%; IQR: 13.4–19.1, p value < 0.01), lower number of ICU beds per 100,000 population (0; IQR: 0–18.8, p value < 0.01), lower number of PCP per 1,000 population (1.2; IQR: 0.5–1.6, p value < 0.01), and a higher proportion of adults smoking in population (22.5%; IQR: 19–26.5, p value < 0.01) as compared to counties with lower CFRs.
Table 2.
County-Level Characteristics Comparisons by Quintiles of COVID-19 Case-Fatality Rate, Among Texas Counties through April 8, 2020
| 0.00% (No Deaths) | 0.6–2.0% | 2.1–3.9% | 4.0–9.9% | > 10% | p valuea | |
|---|---|---|---|---|---|---|
| 206 | 12 | 12 | 13 | 11 | ||
| Presented as median (IQR)b | ||||||
| Race | ||||||
| % NH-White | 63.0 (45.9–76.0) | 51.4 (32.6–60.6) | 51.8 (46.1–64.2) | 63.2 (56.9–66.0) | 70.7 (59.6–81.9) | 0.05 |
| % NH-Black | 3.0 (0.9–6.9) | 10.4 (6.1–16.4) | 7.0 (6.0–16.1) | 8.8 (2.6–17.6) | 3.4 (1.7–16.9) | < 0.01 |
| % Hispanic | 26.0 (16.1–48.5) | 26.1 (22.0–39.9) | 24.8 (17.5–37.3) | 23.6 (17.9–33.1) | 12.2 (8.3–25.4) | 0.28 |
| % Female sex | 50.3 (48.6–50.8) | 50.7 (50.3–51.0) | 50.7 (50.4–51.1) | 50.6 (49.5–50.8) | 50.7 (49.7–50.8) | 0.15 |
| % Age 65+ | 16.6 (13.8–20.3) | 9.5 (8.5–11.4) | 11.2 (10.2–13.2) | 12.7 (10.9–13.9) | 16.6 (13.4–19.1) | < 0.01 |
| ICUc beds per 100,000 population | 0 (0–0) | 22.7 (16.7–25.7) | 35.8 (25.8- 82.7) | 16.3 (12.0- 23.1) | 0 (0–18.8) | < 0.01 |
| PCPd per 1,000 population | 1.3 (0.4–4.1) | 0.1 (0–0.2) | 0.4 (0.2–0.5) | 0.4 (0.2–1.0) | 1.2 (0.5–1.6) | < 0.01 |
| % Could not visit due to cost | 22.6 (16.3–26.4) | 18.7 (14.25–22.5) | 17.8 (15.9–20.7) | 19.8 (14.6–22.6) | 17.6 (11.6–21.0) | 0.11 |
| Unemployment rate | 5.9 (4.8–7.0) | 6.7 (6.0–7.4) | 6.1 (4.7–7.1) | 6.4 (5.5–6.8) | 6.1 (5.6–9.9) | 0.18 |
| % Adult obesity | 29.6 (28.8–31.2) | 28.9 (26.1–29.9) | 28.7 (28.1–31.8) | 29.8 (28.6–31.2) | 29.7 (29.1–31.0) | 0.22 |
| % Adult smoking | 22.1 (18.5–28.2) | 14 (11.0–15.5) | 19.5 (17.6–21.7) | 18.35 (13.4–22.5) | 22.5 (19–26.5) | < 0.01 |
aSignificance determined using Kruskal–Wallis tests, p values < 0.05
bIQR = interquartile range
cICU = intensive care unit, ICU bed tally does not include Veterans Affairs hospitals, which are sure to play a role in treating COVID-19 patients, because VA hospitals do not file cost reports to CMS
dPCP = primary care physicians
Trend of Cumulative Cases of COVID-19 Through April 8th 2020 by Race
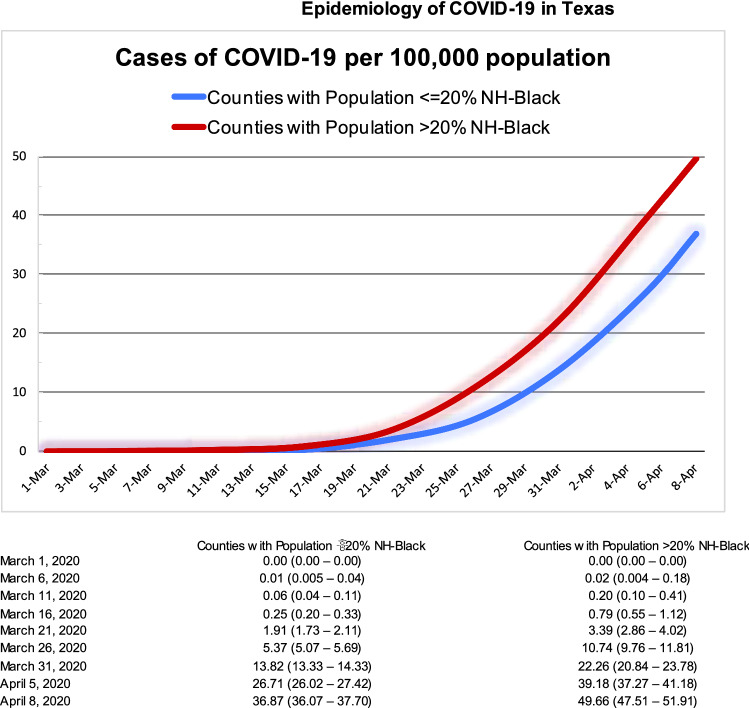
In Fig. 3, we present the trend of cumulative cases of COVID-19 per 100,000 population comparing counties with population of ≤20% non-Hispanic-Blacks with those having > 20% non-Hispanic-Blacks. By 8th April, counties with population of > 20% non-Hispanic-Blacks experienced significantly higher incidence rate of 49.66 (95% CI 47.51–51.91), compared to the rate of 36.87 (95% CI 36.07–37.70) in counties with population of ≤ 20% Non-Hispanic-Blacks.
Fig. 3.
Cumulative cases of COVID-19 per 100,000 population and associated 95% confidence intervals
Discussion
To date, this is the first study to describe the epidemiology of COVID-19 in the state of Texas, with geographic trends and explaining possible county-level differences that are correlated with higher incidence and case fatality rates. As expected, we observed that metropolitan areas of Houston, Dallas-Fort Worth, Austin, San Antonio, El Paso and Lubbock had the overall highest number of confirmed cases as well as incidence rates in Texas. In terms of fatality, it seems that the metropolitan areas of Houston and Dallas are doing fairly well. The counties with highest CFRs, such as Comal, Hockley, are located in peripheral parts of cities as well as in rural Texas. Counties with case-fatality rates of more than 10% have significantly lower health care resources, specifically intensive care unit beds and active primary care physicians. Additionally, it is concerning that the counties which have not yet experienced any COVID-19 deaths are very similar to the counties with the highest case-fatality rates with respect to sociodemographic factors and healthcare resources.
As per the data published by the Chinese Center for Disease Control and Prevention, it is estimated that around 19% of COVID-19 patients (severe 14% and critical 5%) eventually require ICU admission [4]. Although Texas has an estimated 6,199 ICU beds available for critically ill patients, we observed that the case-fatality rates were higher in counties with low to none ICU beds available. The need of transport from rural areas can cause significant delays in appropriate treatments and might be the cause of high CFRs in these areas. Availability of ICU beds and provision of highest standards of critical care are paramount for lowering the total mortality.
Moreover, we observed that the counties having higher proportion of black population are experiencing significantly higher incidence rates. It might be possible that the black population is being hit high disproportionately by SARS-CoV-2 infection. It is likely that the lower socio-economic status and higher prevalence of chronic medical conditions are causing these communities to suffer more. Policymakers and public health professionals will need to take extra measures to protect these vulnerable communities, who are also more likely experiencing higher economic hardships because of this pandemic.
The coming weeks are critical for Texans. It is important that everyone practices social distancing and help communities by preventing further spread of disease. While urban areas of Texas account for the majority of COVID-19 cases, the higher case-fatality rates and low health care capacity in rural areas will be the defining factor. The policymakers, public health and medical professionals will need to strategize and appropriately allocate resources to the above mentioned under-resourced areas as well as take specific measures for protecting vulnerable populations.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SK and JM. The first draft of the manuscript was written by SK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
There is no funding support for this work.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CSSEGISandData. (2020). CSSEGISandData/COVID-19. https://github.com/CSSEGISandData/COVID-19 (Original work published 2020)
- 2.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Team, I. C.-19 health service utilization forecasting, & Murray, C. J. (2020). Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. MedRxiv, 2020.03.27.20043752 10.1101/2020.03.27.20043752.
- 4.Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72, 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]