As coronavirus disease 2019 (COVID-19) struck many countries worldwide in early 2020, the Taiwan government responded rapidly to minimize imported cases and community spread in Taiwan [1]. Many hospitals took proactive measures, including quarantine strategies at the entrances [2]. However, as shown by several reports, SARS-CoV-2 might be transmitted by asymptomatic carriers [3,4]; also symptomatic individuals may evade hospital entrance quarantine measures. On 19th February 2020 the Central Epidemic Command Center (CECC) reported a Taiwanese case who was admitted for pneumonia, with a diagnosis of COVID-19 made three weeks after her admission [5]. Many medical staff who had cared for the case were consequently quarantined. This case highlights the need to maintain a high level of suspicion for COVID-19, particularly in patients whose pneumonia does not respond to antibiotic treatment.
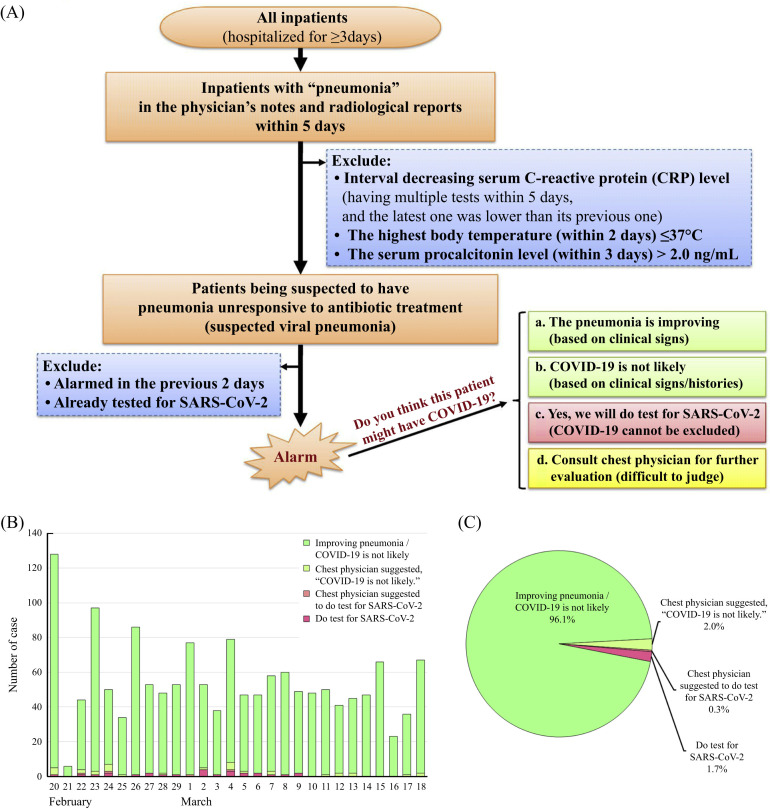
In order to identify inpatients whose pneumonia did not show marked improvement with antibiotic treatment and to alert the primary care medical teams on a daily basis, a prospective active surveillance system was developed with Information Technology Services (Figure 1 A). Each morning all inpatients with pneumonia were identified by searching electronic medical records (medical notes and radiologic reports), with the keyword “pneumonia”. Patients with an improving clinical course were then excluded, including those with interval decreasing serum C-reactive protein levels and those with no fever (>37°C) for >48 h. Patients with a recent serum procalcitonin level more than 2.0 ng/mL were also excluded because bacterial pneumonia is more likely. Patients whose oropharyngeal or nasopharyngeal swab had tested negative for SARS-CoV-2 were also excluded. To avoid an excessive number of alarms, patients in the alarm lists from the previous two days were also excluded; in other words, a patient with persistent non-improvement only alarmed every third day. The alarms were integrated into the Critical Value Notification System, which was originally used to report high-risk or life-threating examination results. Each morning, alarms were sent to the primary care medical teams, including attending physicians, residents, and nurse practitioners, as well as the head nurses via the hospital information system and short message service. To facilitate prompt management, the primary care medical teams were required to reply to the alarms within an hour by answering a multiple-choice question, “Do you think this patient might have COVID-19?” The infection control team analysed the replies and took action daily.
Figure 1.
(A) The algorithm of the Prospective Surveillance Electronic System of Inpatients with Pneumonia Unresponsive to Antibiotics. (B) The numbers of different replies to the alarms from 20th February to 18th March 2020. (C) Distribution of the replies to the alarms from 20th February to 18th March 2020.
Between 20th February and 18th March 2020, around 300 inpatients with pneumonia were found daily; after applying exclusions, an average of 54 alarms were sent (Figure 1B). Although COVID-19 was considered unlikely in most alarm cases, a small proportion (approximately 2% of alarm cases) were tested for SARS-CoV-2 (Figure 1C). Until now, no COVID-19 case had been diagnosed in an existing inpatient.
Our surveillance system demonstrated the utility of information technology to facilitate infection control. The algorithm efficiently excluded about 80% of cases from the alarm list, so that we could focus on a small proportion of cases with higher probability. This model, detecting the cases with poor response to the current antibiotic treatment, might be applied in the antibiotic stewardship program in the future.
We believe the current system still requires improvement. Firstly, we only used “pneumonia” as the keyword to search for cases, so those having reverse semantics, such as “no pneumonia” and “pneumonia is excluded”, in medical records were also included. This problem might be solved by using artificial intelligence with semantic analysis. However, the system load is a concern because the surveillance system works during the busiest hours for information systems. Secondly, the exclusion criteria used in the algorithm was somewhat arbitrary, and requires further testing. For example, some experts might argue about the CRP criteria used and suggest the exclusion of those having a 50% decrease in CRP level. However, stricter exclusion criteria would bring more false alarms. As our surveillance system aimed to remind the physicians about the possibility of COVID-19 in cases with pneumonia obviously unresponsive to antibiotics, it was important to keep a reasonable number of alarms to avoid fatigue.
“To be prepared for war is one of the most effectual means of preserving the peace.” Although our hospital has strict quarantine measures for patients and visitors entering the hospital, there remains a risk of nosocomially-acquired COVID-19. Early identification of undiagnosed cases (whether the infection was undiagnosed at the time of admission or acquired after admission) can facilitate prompt action to minimize nosocomial spread, thereby protecting staff and patients.
Acknowledgement
The authors thank our colleagues for their efforts against COVID-19.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 2.Lee I.K., Wang C.C., Lin M.C., Kung C.T., Lan K.C., Lee C.T. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J Hosp Infect. 2020;105:102–103. doi: 10.1016/j.jhin.2020.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taiwan Centers for Disease Control Taiwan confirms one more confirmed cases; CECC continues to undertake contact tracing and investigation before illness onset. 2020. https://www.cdc.gov.tw/En/Bulletin/Detail/huV-BPgkJ7UJ5D98o1Bdpg?typeid=158