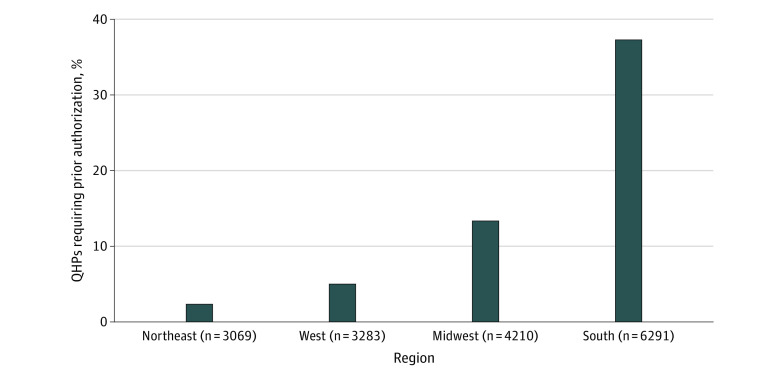
Figure 1. Percentage of Qualified Health Plans (QHPs) That Required Prior Authorization for HIV Pre-exposure Prophylaxis in 2019.
Of the 16 853 unique Affordable Care Act–compliant plans offered in the individual Affordable Care Act Marketplace during 2019, 18.9% of QHPs required prior authorization for combined tenofovir disoproxil fumarate and emtricitabine (the medication used for HIV pre-exposure prophylaxis). This percentage varied by region, with 2.3%, 6.2%, 13.3%, and 37.3% of plans requiring prior authorization in the Northeast, West, Midwest, and South, respectively.