Figure 1.
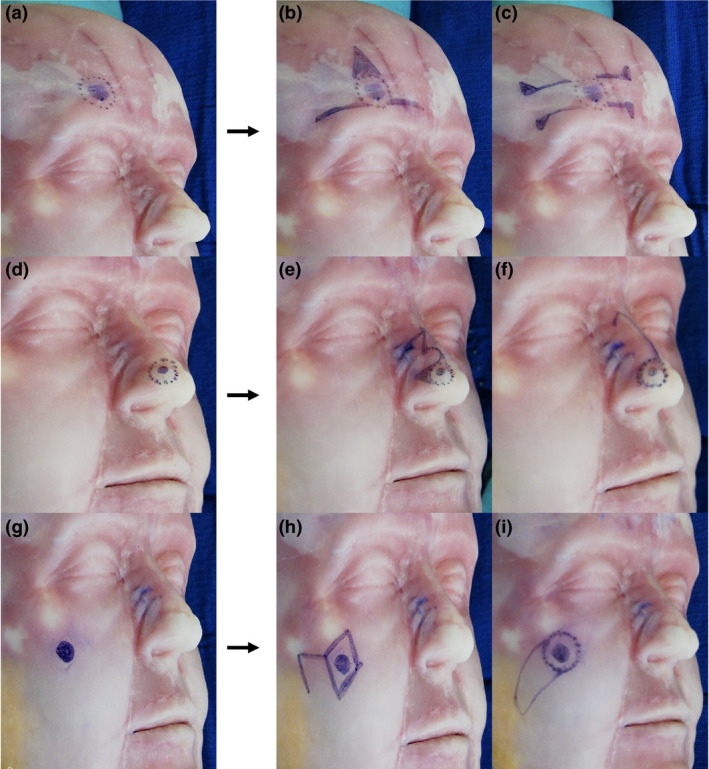
Example of how surgical trainees practise dermatologic surgery with a simulator (Diaphanous Zsa Zsa, DermSurg Scientific). In this example, surgical trainees were given a hypothetical case scenario in which the patient was going to have a wide‐margin excision surgery for a basal cell carcinoma in three different locations: forehead, nose and cheek. After the session, trainees and professor have a discussion session to improve flap designs and repair methods of the hypothetical case. (a) A 1‐cm cutaneous malignancy in the forehead above the right eyebrow is drawn with a 4‐mm excision margin. (b) O‐T flap is designed for reconstruction. Standing cutaneous deformity (SCD) was drawn for excision. (c) Bilateral unipedicle advancement flaps are combined to repair defect resulting in horizontally oriented H‐shaped wound closure (H‐plasty). Burrow triangles were drawn for excision for flap advancement. (d) A 0.70‐cm cutaneous malignancy in the nose involving lateral wall and alar lobule was drawn with a 4‐mm excision margin. (e) Design of a bilobed flap for reconstruction with SCD was drawn. (f) A modified rotation dorsal flap is drawn. A back cut for flap advancement is shown. (g) A 0.9‐cm cutaneous malignancy in the mandibular location is drawn. (h) The classic rhombic flap (Limberg) with a 4‐mm margin is designed to repair the defect. (i) An island advancement flap with a skin pedicle is designed to repair the defect.
