The current global crisis produced by the SARS-CoV-2 pandemic is unprecedented. Even the 1918 influenza pandemic (Spanish flu) did not halt the planet so abruptly and deeply as it ran during World War I.
At the end of 2019, China reported an outbreak of atypical pneumonia in Wuhan, a large city of 12 million people located along the Yangtse river, 500 km west of Shanghai on the coast. By mid-January 2020, Chinese media announced that a novel coronavirus was responsible for the emerging respiratory illness, named COVID-19. Thousands of people had become sick, and local hospitals collapsed.1
Chinese health authorities decided to proceed with strict social disconnecting measures and lockdown the city of Wuhan, in an attempt to stop further human transmission.2 Despite all efforts to contain virus spread, COVID-19 cases began to be reported in other Chinese regions. Soon thereafter, there were reports at neighboring countries, such as Thailand, Japan, and South Korea. By the end of January, cases had been identified in persons arriving from China in the European Union and the United States.3–5 The first case in Spain was reported on 31 January in a German tourist visiting the Canary islands.
Human coronaviruses are well-known agents of seasonal respiratory tract infections, overall causing less than 15% of winter colds. To date, four endemic human coronaviruses have been identified. Whereas CoV-229E and CoV-OC43 were first reported in the 1960s, CoV-NL63 was described in 2003 and CoV-HKU1 in 2005.6 Like SARS-CoV-2, CoV-OC43 and HKU1 are beta-coronaviruses and share some cross-immunity.
Besides endemic human coronavirus infections, another two human coronaviruses had caused serious epidemics during recent years. At the end of 2002, China reported an outbreak of severe acute respiratory syndrome (SARS) that was produced by a new coronavirus, named SARS-CoV.7 Tracing of contacts led to containment of virus spread. By the summer of 2003, infection had been confirmed in 8096 persons, of whom 774 (9%) had died. Since then, no more cases of SARS have been reported elsewhere.7
In 2012, severe atypical pneumonia linked to a new coronavirus (MERS-CoV) was first described in Saudi Arabia. To date, 2519 confirmed cases have been reported in more than 25 countries, mostly in the Middle East, with 866 deaths (34.3%).8
The landing in Europe of SARS-CoV-2 infection was first acknowledged by a huge outbreak in North Italy beginning in the second half of February 2020. Since then, hundreds, and soon thousands, of cases begun to be reported on a daily basis.9 In the absence of effective antivirals and/or vaccines, closing of schools and universities, cancellation of public events, travel restrictions, closing of industries, shops, borders, and ultimately universal home confinement was ordered. Weeks behind, a similar crisis was reproduced in most European countries, although with distinct intensities.
In Spain, the COVID-19 outbreak emerged with high numbers in the first week of March. Within 8 weeks, roughly 250,000 cases and 25,000 deaths had accumulated. The number of deaths is striking, with the highest mortality rate worldwide (544 per million population). For comparison, reported COVID-19 deaths rates for Italy, France, and Germany were 485, 386, and 83 per million, respectively.10 Furthermore, in the absence of viral testing for all suspected cases due to shortage of diagnostic tests, these figures underestimate the real numbers, especially for the denominator of infected cases. Indeed, recent modeling analyses have highlighted that up to 15% of the 47 million Spanish population could had been infected by the end of March 2020.11 Current serosurveys in Spain have provided rates of prior exposure between 5% and 20%, with variations depending of study populations (i.e. greater rates in health care workers) and locations (i.e. greater in large urban cities, such as Madrid and Barcelona).
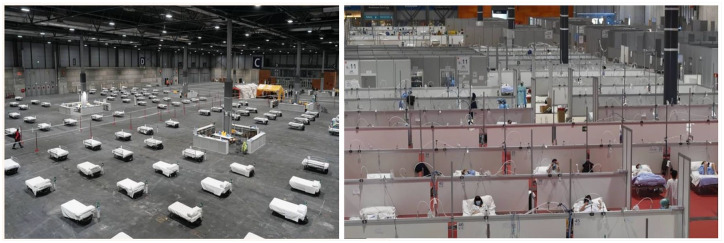
By the first week of April, the current scenario in Madrid, Spain, was unbelievable. Streets empty, industries closed, minimal transportation, and most people confined at home. In contrast, hospitals were overwhelmed, especially emergency rooms and intensive care units, whereas new large exhibition facilities had been medicalized and began hosting of hundreds of sick people (Figure 1). Noise around, all news on TV, social networks, and internet were filled with COVID-19.
Figure 1.
Medicalized exhibition halls for COVID-19 built within 1 week in Madrid, Spain (March 2020).
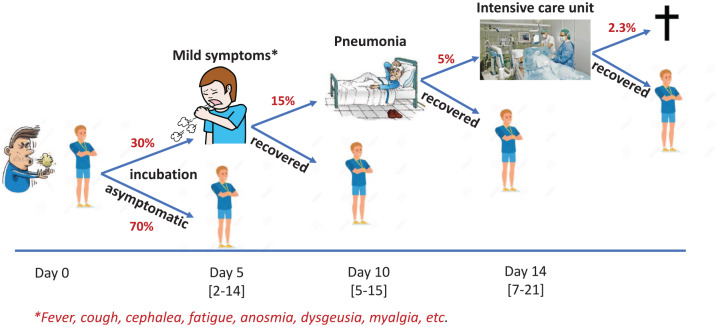
Several features of the Spanish experience merit special attention. First, a disproportionate number of health care providers (doctors, nurses, etc.) were infected early (15% of total cases) or were resting in quarantine, leaving their jobs when they were needed more than ever. A shortage of diagnostic tests and personal protective equipment (masks, gloves, etc.) also contributed to this. Second, a large number of deaths were of people older than 75 years (>75% of total deaths), many of them living in nursing homes. Third, the high contagiousness of the coronavirus accounted for large chains of transmission during crowded gatherings and demonstrations arranged before the country lockdown took place on 14 March. As shown in Figure 2, prevention measures for strategic populations were not addressed in time, and this contributed to the high death toll in Spain.
Figure 2.
Stratification of strategic community populations for COVID-19.
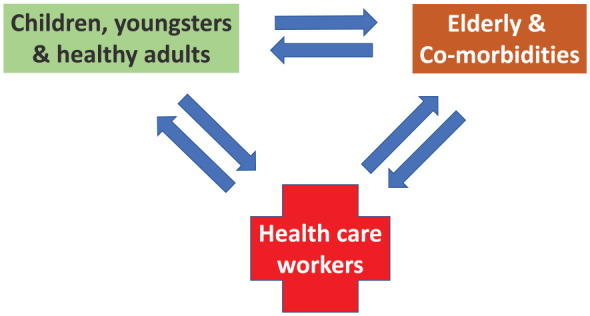
After attending many individuals infected with SARS-CoV-2, it is clear that COVID-19 is not flu. Overall symptoms are more intense and last longer (Figure 3). By the end of March 2020, up to 6100 COVID-19 patients were in intensive care units in Spain. Although older age was by far the most important prognostic factor, severe cases also occurred in young adults without co-morbidities. A genetic predisposition for developing acute respiratory distress is currently being investigated. Hypothetically, the innate immune response in a subset of individuals might show hyper-inflammatory responsiveness to SARS-CoV-2 infection, leading to the characteristic cytokine storm that characterizes severe COVID-19.12
Figure 3.
Clinical course of SARS-CoV-2 infection.
Stepwise escalation of employees being sent home was arranged in the earliest days of the outbreak by some enterprises with success.13 After 6 weeks, a progressive de-escalation and back-to-work strategy is currently ongoing with caution following a plateau and drop in numbers. Herd immunity still has not been reached, but active SARS-CoV-2 cases are very low after 6 weeks of strict home confinement and travel bans (Figure 4). Anyway, in order to minimize the risk of a COVID-19 rebound, it would be important to have access to specific antibody tests for deferring as much as possible risky exposure for individuals without prior viral infection, especially the elderly population and those with co-morbidities. Hopefully any new COVID-19 wave will not be as the first COVID-19 ‘tsunami’ wave, as hospitals are now well prepared (Figure 5).
Figure 4.
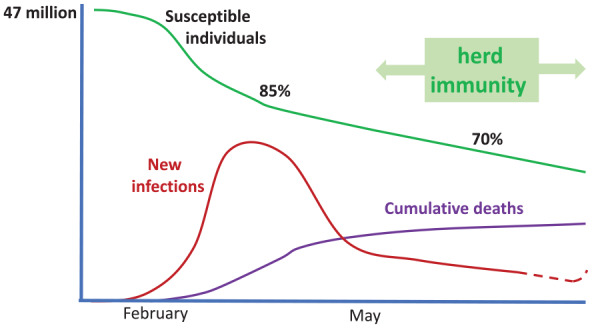
Projection of SARS-CoV-2 infection in Spain.
Figure 5.
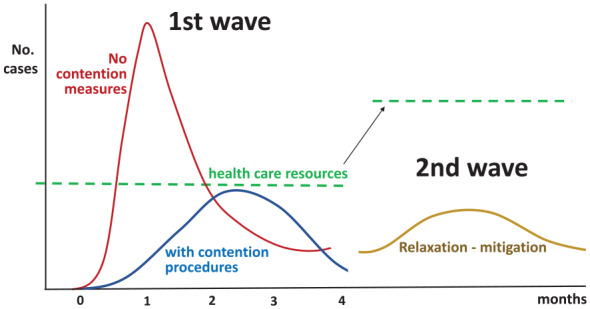
Dynamics of COVID-19 in a community.
Impact of social disconnecting and health care resource capacity preparedness.
Since a vaccine is not envisioned before the end of the year in the best scenario, and sheltering uninfected people at home indefinitely is not possible, the acquisition of natural infection gradually by people seems the best way to minimize the impact of COVID-19. With adequate health vigilance and support, the death toll will largely be minimized next winter, especially for the elderly. No doubt, a major lesson from COVID-19 regards the need to revisit the care of the older sick population, both in terms of improving their medical management and addressing isolation and loneliness.14 All the suffering from this hard time of COVID-19 could be worth it. This aim would be in line with a refreshment of our deeper medical vocation,15 in which patients and society trust and have applauded every night during these weeks.
Footnotes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Vicente Soriano  https://orcid.org/0000-0002-4624-5199
https://orcid.org/0000-0002-4624-5199
Contributor Information
Vicente Soriano, UNIR Health Sciences School, Madrid, 28040, Spain.
Pablo Barreiro, Hospital Carlos III-La Paz, Madrid, Spain.
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lau H, Khosrawipour V, Kocbach P, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med 2020; 27: taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hodcroft E. Preliminary case report on the SARS-CoV-2 cluster in the UK, France, and Spain. Swiss Med Wkly 2020; 150. [DOI] [PubMed] [Google Scholar]
- 4. Holshue ML, De Bolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382: 929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lau H, Khosrawipour V, Kocbach P, et al. The association between international and domestic air traffic and the coronavirus (COVID-19) outbreak. J Microbiol Immunol Infect. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Killerby M, Biggs H, Haynes A, et al. Human coronavirus circulation in the United States 2014-2017. J Clin Virol 2018; 101: 52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peiris J, Guan Y, Yuen K. Severe acute respiratory syndrome. Nat Med 2004; 10(Suppl. 12): 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Memish Z, Perlman S, Van Kerkhove M, et al. Middle East respiratory syndrome. Lancet 2020; 395: 1063–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khosrawipour V, Lau H, Khosrawipour T, et al. Failure in initial stage containment of global COVID-19 epicenters. J Med Virol 2020 Apr 16. doi: 10.1002/jmv.25883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flaxman S, Mishra S, Gandy A, et al. Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. Imperial College COVID-19 Team Response DOI: 10.25561/77731 [DOI] [Google Scholar]
- 12. Pedersen S, Ho Y-C. SARS-CoV-2: a storm is raging. J Clin Invest 2020; 130: 2202–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Soriano V, Corral O. Keeping alive enterprises whereas embracing unprecedented COVID-19 restrictions. Ther Adv Infect Dis 2020; 7: 2049936120920175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fallon A, Dukelow T, Kennelly S, et al. COVID-19 in nursing homes. QJM 2020. doi: 10.1093/qjmed/hcaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med 2020. doi: 10.1056/NEJMp2003149. [DOI] [PubMed] [Google Scholar]