Abstract
Purpose
To report successful management of acute ocular graft-versus-host disease (oGVHD) by self-retained cryopreserved amniotic membrane (AM).
Observations
A 69-year-old male developed acute oGVHD following hematopoietic stem cell transplantation (HSCT) with severe dryness, pain, photophobia, and blurred vision, the right eye worse than the left eye. Despite topical artificial tears, corticosteroids, and bandage contact lens (BCL) for two weeks, his right eye deteriorated with increasing redness and blurred vision and presented with diffuse conjunctival inflammation, severe superficial punctate keratitis, and corneal and limbal epithelial defect. Hence, self-retained cryopreserved AM was applied in the right eye while conventional therapy was continued in the left eye. Placement of self-retained AM for 3-days resulted in resolution of symptoms, reduction in inflammation, and complete re-epithelialization of the corneal and limbal defect with the visual acuity improving from 20/500 to 20/70 in the right eye. In contrast, the visual acuity improved from 20/300 to 20/150 and remained inflamed with conventional therapy in the left eye. One-month post-AM placement, the right eye remained asymptomatic with the visual acuity improved to 20/30 without any additional therapy, whereas the left eye improved to 20/70 with conventional treatment of BCL, loteprednol, and artificial tears.
Conclusions and Importance
This case suggests application of self-retained AM can be an effective treatment to accelerate the restoration of vision and corneal surface health for acute oGVHD.
Keywords: Amniotic membrane, Dry eye, Ocular inflammation, Ocular graft-versus-host-disease, Ocular surface
1. Introduction
Ocular graft versus host disease (oGVHD) is a devastating immune-mediated complication of allogeneic hematopoietic stem cell transplantation (HSCT) that presents as a Stevens Johnson-like or a Sjogren-like syndrome.1 It affects nearly 40–60% of patients treated with HCST and is associated with extensive fibrosis of the lacrimal glands, severe inflammation, loss of goblet cells, symblepharon, and fornix shortening.1 Progressive disease can also lead to non-healing corneal ulcers or perforation caused by limbal stem cell deficiency.1
Topical immunosuppressants and corticosteroids are commonly used therapies for managing inflammation associated with oGVHD. However, for some cases, these treatments have been associated with neurotoxic effects and have poor tolerance.2 Artificial tears, punctal plugs, and scleral lenses are also often used (after control of inflammation); however, these options are palliative in nature to decrease tear evaporation, provide lubrication, and decrease continuous ocular surface trauma.2 Other recent advances that show promising results are blood preparations (such as autologous serum) and amniotic membrane (AM).2, 3, 4, 5 For the latter, the efficacy has been demonstrated in immune6 or non-immune related dry eye disease,7 severe chemical or thermal injury,8 and Stevens Johnson Syndrome.8 AM's efficacy derives from its anti-inflammatory, anti-scarring, and regenerative properties that pose an attractive multi-modality treatment option for oGVHD.9 While sutured AM has been used to treat severe refractory oGVHD,4,5 there is no reported case of using sutureless AM in treating acute oGVHD.
1.1. Case report
A 69-year-old male presented with a past medical history of acute myeloid leukemia (AML) that was subsequently treated with HSCT in 2013. On March 2017, he developed two episodes of systemic GVHD (lung followed by liver and skin) that were treated with adalimumab, mycophenolate mofetil, tacrolimus, and oral corticosteroids. Six weeks following the systemic GVHD liver and skin involvement, the patient reported rapid progressive onset of eye irritation that was treated with artificial tears, topical corticosteroids, and bandage contact lens (BCL) without improvement. He presented to Upstate Medical Center two weeks later with severe ocular pain, dryness, photophobia, and significant decrease in vision in the right eye greater than the left. During his visit the patient reported no worsening of systemic disease or new changes in systemic therapies. The patient also denied any recent chemical or thermal insults to his eyes prior to onset of his symptoms.
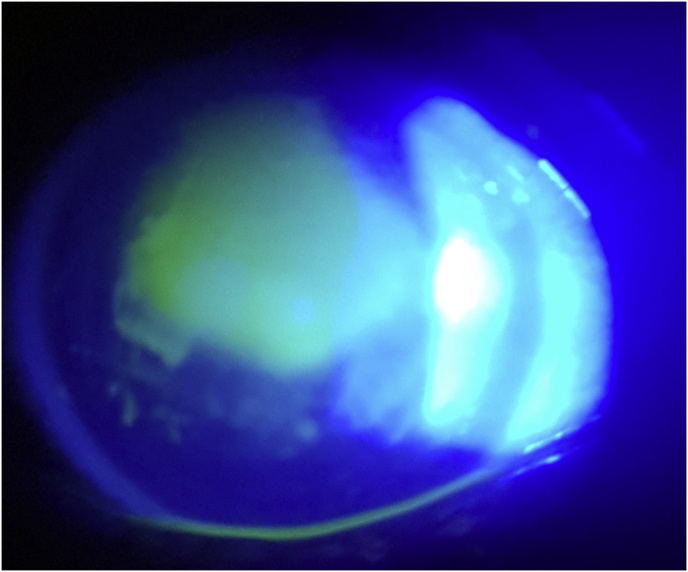
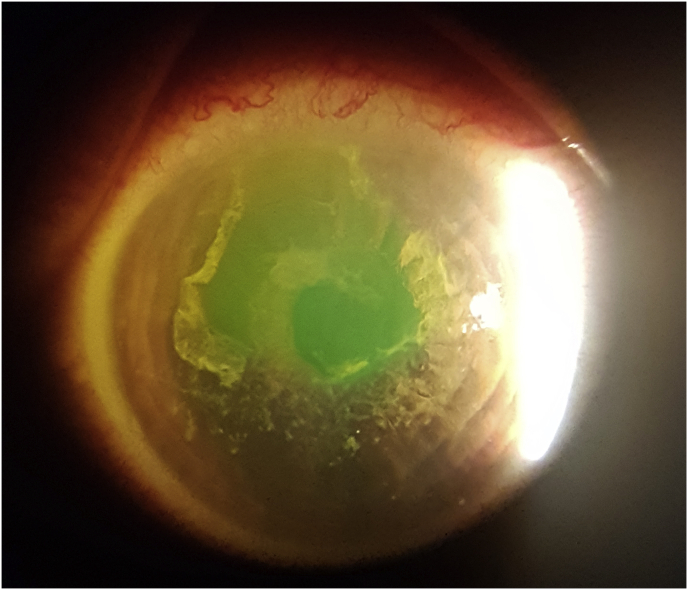
Upon examination, the patient's vision was 20/500 right eye and 20/300 left eye with bilateral erythema of upper and lower eyelids. Both eyes revealed diffuse conjunctival injection, scant tear meniscus, irregular corneal tear film, swelling of puncta as well as mucus and debris deposition in the fornices. The right cornea revealed a large epithelial defect and limbal inflammation (Fig. 1, Fig. 2). The left cornea showed surface irregularity with diffused 3+ superficial punctate keratitis (SPK) which was graded according to oGVHD ocular staining score.1 The anterior chamber of the right eye was difficult to assess due to poor ocular surface, while that of the left was deep and quiet. The dilated funduscopic exam was unremarkable in both eyes. The patient was thus diagnosed with bilateral severe acute findings of oGVHD-related keratopathy. Because the right eye was markedly worse than the left eye, a self-retained cryopreserved AM, PROKERA® Slim (PKS) (Bio-Tissue, Inc., Miami, FL, USA) was placed in the right eye and the left eye was maintained on topical artificial tears, BCL, and topical corticosteroids every 2 h with bilateral inferior punctal plugs.
Fig. 1.
Acute ocular surface inflammation in the right eye before amniotic membrane (AM) insertion showed large corneal epithelial defect.
Fig. 2.
Large corneal and limbal epithelial defect with diffuse conjunctival injection in the right eye before amniotic membrane (AM) insertion.
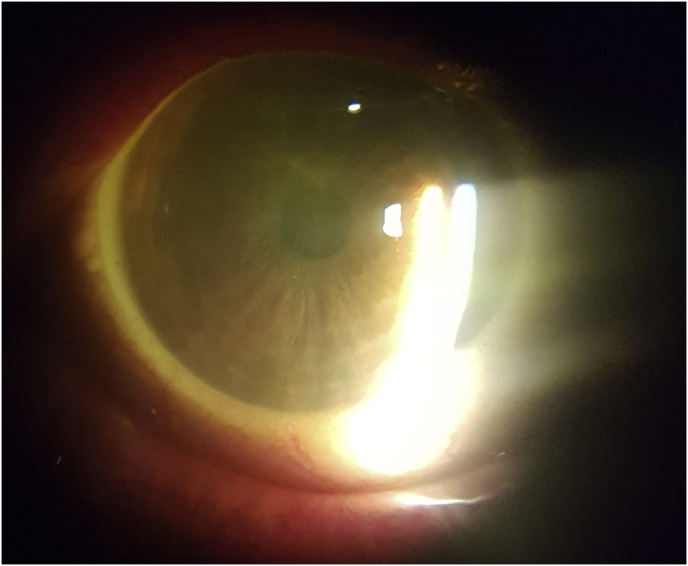
Three days later, after removal of AM in the right eye and BCL in the left eye, his vision improved to 20/70 right eye and 20/150 left eye. The examination revealed complete epithelialization of the corneal and limbal surface and significant decrease in conjunctival inflammation in the right eye (Fig. 3). In addition, the patient reported complete resolution of pain, irritation, photophobia, and dryness in the right eye. In contrast, the left eye still had residual 2+ SPK with persistent symptoms.
Fig. 3.
Complete re-epithelialization and reduced inflammation 3 days after placement of sutureless cryopreserved amniotic membrane (AM).
At one-month follow up, the patient remained asymptomatic with further improvement in visual acuity to 20/30 without any additional therapy in the right eye. However, the visual acuity of the left eye was 20/70 while continuing on BCL, topical loteprednol, and artificial tears 4 times daily. The right eye had a clear cornea, no conjunctival inflammation, good tear lake and moderate tear break up time of 7 seconds. In contrast, the left eye had residual conjunctival inflammation with 1+ SPK on corneal surface, low inferior tear meniscus height, and rapid tear break up time of 2 seconds. The ocular surface disease index (OSDI) score improved from 45 at initial presentation to 21 at one month follow up, with most of the symptoms from the left eye. The patient was transitioned to topical cyclosporine and artificial tears in both eyes as maintenance therapy. At six-month follow up, the patient remained symptom-free while exhibiting a clear cornea with best-corrected visual acuity of 20/20 and no inflammation or scarring in the right eye.
2. Discussion
The current available therapy for oGVHD is limited. Conventional therapies such as artificial tears and BCL cannot reverse the underlying immunologic process of oGVHD and rather are directed towards alleviating symptoms. Anti-inflammatory drops like corticosteroids can reduce inflammation but may result in ocular hypertension, early cataract, delayed corneal epithelialization, and predisposition to ocular surface infection. While autologous serum has shown early effectiveness in restoring ocular surface health of oGVHD,3 it is sometimes difficult to find available compounding pharmacies. Previously, sutured AM transplantation has been reported to successfully manage chronic severe oGVHD.4,5 Compared to the fellow eye that was treated with conventional therapy, this case showed that acute oGVHD can also be successfully treated with self-retained cryopreserved AM by accelerating corneal epithelialization and reduced conjunctival inflammation. As reported in acute chemical burns and acute Stevens Johnson syndrome, early intervention, within the first to second week of onset of symptoms, appears to be crucial to facilitate regenerative healing along with reducing inflammation and scarring.8 In this regard, we believe that the sutureless mode of applying cryopreserved AM is more advantageous than sutured AM because it can be easily placed in the office.
Both sutureless and graft cryopreserved AM contain HC-HA/PTX3 (heavy chain-hyaluronic-pentraxin3) complex, which is uniquely present in AM and exerts anti-inflammatory and anti-scarring mechanisms.8,9 Specifically for GVHD, subconjunctival injection of HC-HA/PTX3 purified from human AM has been shown to prevent the development of oGVHD when given at the time of allogeneic HSCT in mice by preserving tear secretion, maintaining conjunctival goblet cell density, and suppressing scarring and infiltration of CD4+ Th 17 effector cells as well as CD45+ and MHC class II + cells in lacrimal glands.9
3. Conclusion
The sutureless approach of AM is important because it can be placed in-office for early treatment of acute oGVHD. This is an early effective anti-inflammatory treatment to restore corneal surface integrity (see Fig. 3), restore visual acuity and potentially avoid serious ocular complications in acute oGVHD. In addition, it also eliminates suture-induced inflammation and the risk of surgical complications. Future studies are needed to examine whether early utilization of AM is opportune in managing both acute and chronic oGVHD to prevent progressive and irreversible damage.
Patient consent
Consent to publish this case report was obtained by the patient. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding was received as part of this work.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: H. Y, S. D., R. W., R. S., S. A., A.C.
Acknowledgements
This work was presented in part at the American Society of Cataract and Refractive Surgery (ASCRS), San Diego, CA, May 2019.
Contributor Information
Han Y. Yin, Email: hhyin003@gmail.com.
Swetha Dhanireddy, Email: swetha.dhanireddy87@gmail.com.
Robert Weisenthal, Email: weisenr@gmail.com.
Robert Swan, Email: swanro@upstate.edu.
Samuel Alpert, Email: alperts@upstate.edu.
Anny M.S. Cheng, Email: acheng@fiu.edu.
References
- 1.Ogawa Y., Kim S.K., Dana R. International chronic ocular graft-vs-host-disease (GVHD) consensus group: proposed diagnostic criteria for chronic GVHD (Part I) Sci Rep. 2013;3 doi: 10.1038/srep03419. 3419-3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tung C.I. Current approaches to treatment of ocular graft-versus-host disease. Int Ophthalmol Clin. 2017;57:65–88. doi: 10.1097/IIO.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa Y., Okamoto S., Mori T. Autologous serum eye drops for the treatment of severe dry eye in patients with chronic graft-versus-host disease. Bone Marrow Transplant. 2003;31:579–583. doi: 10.1038/sj.bmt.1703862. [DOI] [PubMed] [Google Scholar]
- 4.Peric Z., Skegro I., Durakovic N. Amniotic membrane transplantation-a new approach to crossing the HLA barriers in the treatment of refractory ocular graft-versus-host disease. Bone Marrow Transplant. 2018;53:1466–1469. doi: 10.1038/s41409-018-0140-6. [DOI] [PubMed] [Google Scholar]
- 5.Peris-Martinez C., Menezo J.L., Diaz-Llopis M. Multilayer amniotic membrane transplantation in severe ocular graft versus host disease. Eur J Ophthalmol. 2001;11:183–186. doi: 10.1177/112067210101100215. [DOI] [PubMed] [Google Scholar]
- 6.Cheng A.M., Tighe S., Sheha H. Adjunctive role of self-retained cryopreserved amniotic membrane in treating immune-related dry eye disease. Int Ophthalmol. 2018;38:2219. doi: 10.1007/s10792-017-0708-y. [DOI] [PubMed] [Google Scholar]
- 7.Cheng A.M., Zhao D., Chen R. Accelerated restoration of ocular surface health in dry eye disease by self-retained cryopreserved amniotic membrane. Ocul Surf. 2016;14:56–63. doi: 10.1016/j.jtos.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J., Sheha H., Fu Y., al etl. Update on amniotic membrane transplantation. Expet Rev Ophthalmol. 2010;5(5):645–661. doi: 10.1586/eop.10.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ogawa Y., He H., Mukai S. Heavy chain-hyaluronan/pentraxin 3 from amniotic membrane suppresses inflammation and scarring in murine lacrimal gland and conjunctiva of chronic graft-versus-host disease. Sci Rep. 2017;7:42195. doi: 10.1038/srep42195. [DOI] [PMC free article] [PubMed] [Google Scholar]