Abstract
Benign Paroxysmal Vertigo is one of the most common causes of vertigo. The most common semicircular canal involved in pathogenesis of BPPV is Posterior semicircular canal. However anterior and lateral semicircular canals can also sometimes be responsible for BPPV but their involvement in pathogenesis is still underrated. The incidence of lateral semicircular canal BPPV is in literature is around 10–12% while anterior canal is about 3%. The main objective of this study was to provide the database for incidence of lateral canal BPPV from a tertiary care hospital with the aim that more clinicians incorporate this entity into their differential diagnosis when their cases of posterior canal BPPV are refractory. This was an observational cross-sectional study of 300 patients of BPPV who were coming in ENT OPD as primum or as referral. All the patients underwent both the Dix–Hallpike maneuver as well as the supine roll test. The patients who were having upbeating torsional vertical nystagmus on Dix–Hallpike were treated on lines of posterior canal BPPV whereas those with horizontal nystagmus on supine roll test were treated on lines of lateral canal BPPV. The data was tabulated and analysed for the incidence of lateral canal BPPV. Out of 300 patients; 188 were males and 122 were females. Most commonly affected age group by BPPV was 40–50 years. Out of 300 cases 260 cases (86.6%) had posterior BPPV and 37 cases (12.3%) had lateral canal BPPV. 3 cases (1%) also had anterior canal BPPV. 30/37 cases of lateral BPPV had geotropic nystagmus while 7 cases had apo-geotropic nystagmus. Posterior canal BPPv was treated by Epleys maneuver. Superior canal BPPV was treated by Yacovino maneuver. The cases of lateral canal BPPV were treated by either Vannucchi-asprella; Gufoni; Lempert maneuver or by the combination of two maneuvers. Lateral canal BPPV is an important diagnosis to consider in all cases of BPPV. Its true incidence is still under blanket as many clinicians are not using supine roll test routinely in their practice while diagnosing BPPV. Many refractory cases of BPPV can be cured if the involvement of other canals in its pathogenesis is kept in the mind so that correct diagnostic and repositioning maneuvers can be applied. We also encourage more institutional studies on lateral canal BPPV so that a standard treatment protocol with clear indications can be designed for this entity as is available for BPPV.
Keywords: Horizontal canal BPPV, Lateral canal BPPV, Geotropic nystagmus, Apo-geotropic nystagmus, Supine roll test, Bow and bean test, Vannucchi asprella maneuver, Gufoni maneuver, Lempert maneuver
Introduction
Benign paroxysmal positional vertigo is one of the most common disorder causing dizziness [1]. 90% of vertigo/nystagamus cases are attributable to BPPV, which has been recognised as a clinical entity since the late 1800 and early 1900. In 1921 Barany described the characteristic nystagmus and vertigo caused by position changes and attributed these symptom to disorder of otolith organ [2, 3].
In 1952 Dix and Hallpike further described torsional vertical nystagmus provoked by a specific position with the latency of several seconds which showed fatigability, they then coined the term BPPV [4]. In 1969 Schucknecht proposed the theory of cupulolithiasis, according to which the cupla becomes heavy due to the attached otolithic debris from the utricle and gets deflected by position changes thus evoking nystagmus and vertigo, howsoever this concept couldn’t become popular because it had several limitations in explanation of vertigo. This led to the proposal of the concept of canalolithiasis in 1979 by Hall, which stated that otolithic debris from utricle migrates into semicircular canal via the non ampullary portion and free floats in the endolymph of semicircular canal causing vertigo and nystagmus with changes in head position [5, 6].
This concept forms the theoretical basis of canalith repositioning maneuver to treat benign positional paroxysmal vertigo. Prior to 1980 it was believed that benign positional vertigo is mainly due to posterior semicircular canal, however it was the work of McClure in 1985 which first described the role of lateral semicircular canal in benign positional postural vertigo with which came the existence of supine roll test for diagnosis of horizontal canal. Geotropic and apo-geotropic variants of this condition were later identified, with geotropic variant more common than apo-geotropic variant [7, 8]. Till today the role of horizontal canal in benign positional postural vertigo is still the most debatable and grey area of research niche.
Anterior-canal BPPV (AC-BPPV) is considered the rarest form of semicircular canalolithiasis, with a postulated frequency of 1–2% [9]. Since the appropriate treatment consist of canalolith repositioning maneuvers for appropriate semicircular canal, it is crucial and prudent to determine which canal has been affected. Thus primary aim of present study is to estimate the true incidence of vertigo caused by lateral canal in cases of BPPV presented to our outpatient department.
Materials and Methods
Present study was conducted in out-patient ENT department of Sri Guru Ram Das University of Health Sciences from May 2018 to 2019 and 300 patients were included in the study.
Present study is observational cross-sectional study and STROBE reporting guidelines were used (Strengthening the reporting of Observational studies in epidemiology).
All ethical clearance were taken from ethical committee of institute according to principles of declaration of Helsinki.
All efforts were taken to maintain Patient Confidentiality all the times.
Inclusion Criteria
All patients who presented to the OPD with following complaints of vertigo from age group 10–80 years were included in the study [10].
Attacks of rotatory vertigo or dizziness are induced by changes in the head position relative to gravity.
The vertigo appears with short latency, lasts for less than a minute and is characterized by an increase followed by a decrease in its intensity.
The intensity of the vertigo decreases or disappears after repeated head positioning.
The vertigo is not associated with any cochlear symptoms such as hearing loss, tinnitus, or ear fullness.
There are no neurologic symptoms other than vertigo.
Exclusion Criteria
Anxious, Phobic patients who do not wish to undergo any intervention were excluded.
-
Patients with
- Obesity.
- Depression.
- Acute neck trauma.
- Middle ear pathology.
- Cervical spondylosis; cervical instability; cervical disc prolapse.
- Vertebro-basilar Insufficiency.
- Carotid sinus syncope.
- Neurodegenerative disorders.
- Disturbances of consciousness.
All patients included in the study underwent otoscopic examination of bilateral ears. Those with normal tympanic membrane and normal hearing tests were taken for positional tests. Both the Dix Hallpike test and Supine Roll test were done in all the patients.
The Diagnostic Criteria for Posterior Canal BPPV [11]
-
A.
Recurrent attacks of positional vertigo or positional dizziness provoked by lying down or turning over in the supine position.
-
B.
Duration of attacks < 1 min.
-
C.
Positional nystagmus elicited after a latency of one or few seconds by the Dix–Hallpike maneuver or side-lying maneuver (Semont diagnostic maneuver). The nystagmus is a combination of torsional nystagmus with the upper pole of the eyes beating toward the lower ear combined with vertical nystagmus beating upward (toward the forehead) typically lasting < 1 min.
-
D.
Not attributable to another disorder.
We used Dix–Hallpike maneuver as a positional test to diagnose Posterior canal BPPV as it is reported as the gold standard for diagnosing benign positional paroxysmal vertigo caused by a posterior canal otolith [11, 12].
The patient begins sitting up, and their head is oriented 45° toward the ear to be tested. The clinician then lies the patient down quickly with their head past the end of the bed and extends their neck 20° below the horizontal, maintaining the initial rotation of the head. The clinician then watches the patient’s eyes for torsional and up-beating nystagmus, which should start after a brief delay and persist for no more than 1 min. This would indicate a positive test. If the test is negative but clinical suspicion remains high, the patient should be given a chance to recover for at least 1 min, and then testing of the other ear can be undertaken [12–14]. Lateral canal pathology is not detected by this method, for which a supine roll test need to be done if suspected [14]. Posterior semicircular canal involvement is proved from the type of the visually observed paroxysmal positioning nystagmus, which is beating towards the undermost and affected ear, with a torsional component clockwise when following leftward movement, or counterclockwise, when following rightward movement [15]. This is illustrated in Fig. 1 and tabulated in Table 1.
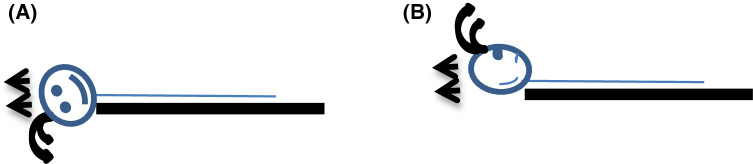
Fig. 1.
Showing the direction of nystagmus in posterior canal BPPV on Dix Hallpike test. a Right sided posterior canal BPPV+ with direction of nystagmus upbeating and counter clockwise towards the right ear; in this scenario left ear is up and right ear is down. b Left sided posterior canal BPPV+ with direction of nystagmus upbeating and clockwise towards the left ear; in this scenario right ear is up and left ear is down
Table 1.
Direction of nystagmus in posterior canal BPPV on Dix Hallpike maneuver
| Isolated right posterior canal BPPV | Upbeating and counter clockwise (towards the affected ear) |
| Isolated left posterior canal BPPV | Upbeating and clockwise (towards the affected ear) |
The Diagnostic Criteria for Lateral Canal BPPV [11]
-
A.
Recurrent attacks of positional vertigo or positional dizziness provoked by lying down or turning over in the supine position.
-
B.
Duration of attacks < 1 min.
-
C.
Positional nystagmus elicited after a brief latency or no latency by the supine roll test beating horizontally toward the undermost ear with the head turned to either side (geotropic direction changing nystagmus).
-
D.
Not attributable to any other disorder.
For patients with LSCC BPPV, direction-changing positional nystagmus (DCPN) is typically observed in a supine-roll test. When DCPN is directed toward the lower most ear (geotropic), gravity dependent movement of otolith particles within the LSCC has been accepted as a possible mechanism (canalolithiasis). In such cases, the nystagmus lasts transiently and shows fatigability. If geotropic positional nystagmus is paroxysmal and transitory, diagnosis of HC-BPPV due to canalolithiasis is virtually certain and no differential diagnosis is required. Typical horizontal canal BPPV (HC-BPPV) is explained by canalolithiasis, although occasionally the mechanism switches from canalolithiasis to cupulolithiasis. In this rare form of HC-BPPV due to cupulolithiasis (the so called apogeotropic variant) nystagmus beats horizontally to the uppermost ear with weaker nystagmus when the head is turned to the affected side and the nystagmus is persistent without latency or fatigability [10, 12, 15]. In literature it been reported that LSCC BPPV may show transition between canalolithiasis and cupulolithiasis [13, 15, 16].
The positional nystagmus test is performed in a supine position and the head is rotated to the right-ear-down or left ear down position. The positional nystagmus test is called the supine roll test (the Pagnini McClure maneuver), which is useful for the diagnosis of the lateral-canal-type of BPPV. During this maneuver, horizontal nystagmus may beat toward the ground or towards the affected ear (geotropic nystagmus) or toward the ceiling or unaffected ear (apogeotropic nystagmus). The affected side in horizontal canal BPPV has been determined by using the HRT with Ewald’s second law. Ewald’s second law states that the magnitude of the ampullopetal stimulation is stronger than that of ampullofugal stimulation in the HSC canal so the induced nystagmus is stronger when the head is turned toward the affected ear in the geotropic type of HC-BPPV. In contrast, in apogeotropic HC-BPPV head turning to the healthy ear generates a stronger nystagmus. The various situations with diagnostic interpretation on supine roll test are tabulated in Table 2 [11, 15, 17].
Table 2.
Diagnosis of HC-BPPV as on supine roll test
| H-BPPV (R) due to canalolithiasis | Head roll test on right—positive | Head roll test on Left—positive |
| Nystagmus: geotropic | Nystagmus: geotropic | |
| More intense than left | Less intense than right | |
| H-BPPV (R) due to cupulolithiasis | Head roll test on right—positive | Head roll test on Left—positive |
| Nystagmus: apo-geotropic | Nystagmus: apo-geotropic | |
| Less intense than left | More intense than right | |
| H-BPPV (L) due to canalolithiasis | Head roll test on right—positive | Head roll test on Left—positive |
| Nystagmus: geotropic | Nystagmus: geotropic | |
| Less intense than left | More intense than right | |
| H-BPPV (L) due to cupulolithiasis | Head roll test on right—positive | Head roll test on Left—positive |
| Nystagmus: apo-geotropic | Nystagmus: apo-geotropic | |
| More intense than left | Less intense than right |
Though supine roll test is quite indispensable for the diagnosis of HC-BPPV and the affected ear is revealed by the direction toward which the most intense nystagmus beats however, sometimes it may be difficult to appreciate a difference between the intensity of the two sides. Determination of the involved side (lateralization) is very important for the proper treatment of HC-BPPV [11]. In such cases Bow and lean test was used.
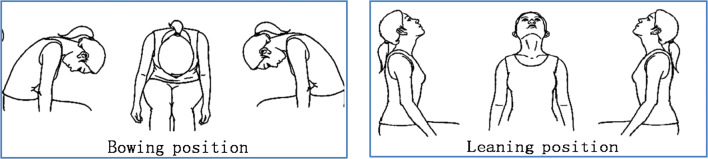
In Bow and Lean the direction of nystagmus was tested when the patient bows the head over 90° (“bowing nystagmus”) and leans the head backward over 45° (“leaning nystagmus”) in the sitting position as shown in Fig. 2. The interpretation of test was done as described in Table 3 [18, 19].
Fig. 2.
Positions for bow and lean test
Table 3.
Interpretation of bow and lean test [19]
| Pathology in H-BPPV | Direction of bowing nystagmus | Direction of leaning nystagmus |
|---|---|---|
| Canalithiasis right ear | Towards right ear | Towards left ear |
| Canalithiasis left ear | Towards left ear | Towards right ear |
| Cupulolitiasis right ear | Towards left ear | Towards right ear |
| Cupulolitiasis left ear | Towards right ear | Towards left ear |
Diagnosis of Anterior Canal BPPV [10, 11, 20, 21]
-
A.
Recurrent attacks of positional vertigo or positional dizziness provoked by lying down or turning over in the supine position.
-
B.
Duration of attacks < 1 min.
-
C.
Presence of a positional vertical down-beating paroxysmal nystagmus evoked through the straight head hanging positioning and sometimes through the Dix Hallpike test. In such positions, possible presence of a clockwise torsional component for the left AC or of a counter-clockwise torsional component for the right anterior canal. Canal conversion in typical posterior canal BPPV during or immediately after (no more than 2 days) the therapeutic manoeuvre, characterised by a vertical up-beating nystagmus, clockwise for the left canal and counter-clockwise.
-
D.
Not attributable to any other disorder especially any central disorder.
The supine straight-head hanging position, by bringing the patient to the supine position with the head 30° (or even more) below the earth-horizontal [11]. Patients with suspicion of Bilateral posterior canal BPPV head-down test was done. In this test the head of the patient was extended directly backward from the sitting to the supine straight head hanging position. During this test, both posterior canals get irritated, resulting in the appearance of nystagmus. This nystagmus has only a vertical upbeating component, because the torsional components, having opposite directions, are cancelled. For patients in which both Dix hallpike and Supine Roll Test were positive they were diagnosed as having both posterior as well as horizontal canal BPPV [15].
Epleys maneuver was done for posterior semicircular canal vertigo. The rehabilitation manoeuvres used in horizontal BPPV.
If were the Vannucchi-asprella manoeuvre; Lempert manoeuvre and Gufoni manoeuvre. Yacovino repositioning manoeuvre for anterior canal BPPV was employed [21–25].
All patients were followed for at least 2 weeks. Cure was defined as complete resolution symptoms and disappearance of nystagmus of nystagmus in the provoking position.
Patients who still exhibited symptoms after treatment but demonstrated no elicitable nystagmus were considered improved.
Persistence of nystagmus indicated treatment failure. Irrespective of the involved canal the brandt daroff exercises were prescribed in all patients of posterior BPPV. The data was analysed and results were tabulated.
Results
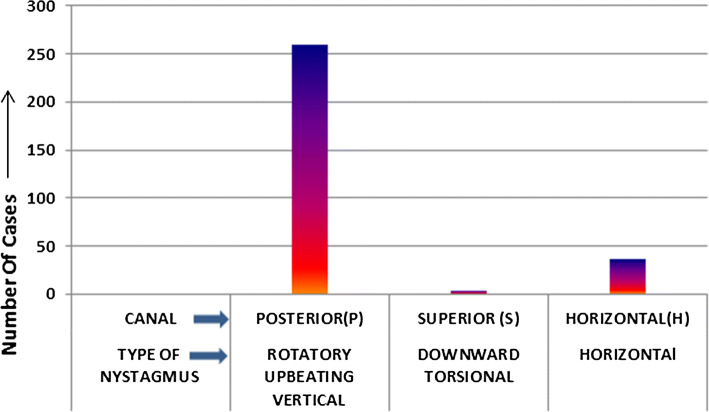
The demographics of present study included 300 patients. There were 188 males and 122 females (Table 4). There were 23 patients in age group less than 40 and 47 patients in age group more than 60 years. 119 patients in age group 40–50 years and 111 patients in 50–60 years age group (Table 4). In present study 260 patients had posterior canal BPPV; 37 had horizontal canal BPPV and 3 cases had anterior canal BPPV (Fig. 3). Out of 37 cases of Horizontal nystagamus 30 were geotropic and 7 were apogeotropic (Table 5). Out of 260 cases diagnosed of BPPV due to posterior canal 258 were successfully treated with Epleys. Though two cases were symptomatically improved with reduced nystagmus still were considered refractory as the patient still had some nystagmus on doing Dix hallpike. The 26/30 cases of geotropic horizontal nystagmus were treated by Vannucchi; Lempert and Gufoni. 2 cases of Apo-geotropic were teated by Vannucchi asprella and 1 case by combination of Vannucchi-asprella with Lempert. 2 cases of Apo-geotropic were treated by Gufoni and 1 case by combination of Gufoni and Lempert (Table 6).
Table 4.
Demographic characteristics of the study
| Demographic variable | Number |
|---|---|
| Gender | |
| Male | 188 |
| Female | 122 |
| Age group | |
| < 40 | 23 |
| 40–50 | 119 |
| 50–60 | 111 |
| > 60 | 47 |
Fig. 3.
This bar diagram shows that in our study (n = 300); 260 (86.6%) cases of BPPV were attributed to posterior semicircular canal; 37 (12.3%) cases of BPPV were attributed to lateral semicircular canal whereas only 3 (1%) cases were associated with anterior semicircular canal
Table 5.
Showing the classification of horizontal nystagmus into its geotropic and apogeotropic types in our study
| Type of horizontal nystagmus | Number of cases (N = 37) |
|---|---|
| Geotropic | 30 |
| Ageotropic | 07 |
Table 6.
Rehabilitation in BPPV due to various canals in our study
| Canal involved in BPPV | Rehabilitation maneuver used | Cases cured/total cases |
|---|---|---|
| Posterior canal | Epleys maneuver | 258/260 |
| Superior canal | Yacovino maneuver | 1/3 |
| Horizontal canal (apo-geotropic) | Vannucchi asprella | 2/7 |
| Vanucchi asprella + lempert | 1/7 | |
| Gufoni | 2/7 | |
| Gufoni + lempert | 1/7 | |
| Horizontal canal (geotropic) | Vannucchi asprella | 17/30 |
| Lempert | 6/30 | |
| Gufoni | 3/30 |
Discussion
Majority of literature commonly suggested that posterior canal is the most common canal in BPPV as it is the most gravity dependent and this led to the assumption that BPPV was a disorder associated with the posterior canal. Since diagnosis and treatment of horizontal canal BPPV is different than posterior canal BPPV it is prudent to diagnose true canal involved for accurate treatment [7]. However present study was conducted to gravitate true incidence of horizontal canal in 300 patients of BPPV and it was found that even though most common cause of BPPV is due to posterior canal but there is definite incidence of horizontal canal involvement, leading to complete resolution of signs and symptoms in cases which would otherwise be labeled as refractory if diagnosis of lateral canal would not have been made. The present study tried to address the very important issue of role of accurate canal involvement for actual diagnosis and treatment of BPPV with large cohort; homogenous population and diagnostic protocol being the major strengths of this study. The major limitation was that it was an observational non randomized study, and hence there are concerns related to internal and external validity and generalibility of results.
In present study out of 300 patients enrolled 188 (62.6%) were males 122 (40.6%) were females and most common age group affected 40–50 years (119 patients) 39.6% followed by age group of 50–60 years (111 patients) 37% (Table 4). According to present study posterior canal 260/300 (86.6)% was most commonly affected followed by horizontal 37/300 (12.3%) and superior 03/300 (1%) (Fig. 3). In studies conducted by Casani et al. [26] Fife et al. [27] Steenerson et al. [28] Honrubia et al. [29] Marcais et al. [30] Korres et al. [31] de la Meilleure following results were concluded for various canals involved in BPPV and are presented in tabulated form Table 7.
Table 7.
Results of the differential involvement of three semicircular canals in BPPV by various studies in literature
| Study | Total BPPV cases | P-SCC % | L-SCC % | Superior SCC % | Mixed |
|---|---|---|---|---|---|
| Casani et al. | 674 | 85.2% | 9.8% | Nil | Nil |
| Fife et al. | 424 | 91% | 6% | 3% | 3% |
| Steenerson et al. | 923 | 91% | 8.7% | Nil | Nil |
| Honrubia et al. | 292 | 93.5% | 5.1% | 1.4% | Nil |
| Marcais et al. | 258 | 93% | 2% | Nil | Nil |
| Korres et al. | 122 | 90.2% | 8.2% | 2.8% | 1.6% |
| de la Meilleure | 287 | 78% | 16.4% | 2.8% | Nil |
Results of all these studies correlated with our present study (Fig. 3) emphasising the fact that there is definitive role of horizontal canal for correct treatment of BPPV. BPPV originating from stimulation of the lateral semicircular canal is the second most common type of BPPV, accounting for approximately 5–15% of the patients but its frequency has been occasionally reported up to 30% [20, 32] Lateral canal BPPV is due to detached otoconia that enter the lateral canal instead of the posterior canal. Vertigo may be more intense than in posterior canal involvement and is usually associated with severe autonomic symptoms [15].
It is characterized by paroxysmal positional nystagmus which is lateral instead of vertical-torsional. The supine roll test is the most commonly utilized method for determining the affected ear in therapeutic trials of horizontal semicircular canal BPPV. The pathological side, which must be identified for successful physical treatment, is usually indicated by nystagmus intensity: the more intense positional nystagmus beats towards the affected ear. In lateral canal nystagmus a geotropic form and a less common apogeotropic form are recognised with former being more amenable to treatment [33] According to Studies conducted by Bertholon et al. [34] and Waespe et al. [35] geotropic nystagmus is more common than apo-geotropic nystagmus and are presented below in tabulated form Table 8. The incidence of geotropic and apo-geotropic nystagmus was found to be similar in our study as presented in Table 5.
Table 8.
Results of studies in literature regarding the incidence of geotropic and apo-geotropic nystagamus
| Study | Geotropic nystagmus (%) | Apogeotropic nystagmus (%) |
|---|---|---|
| Bertholon et al. | 60 | 40 |
| Waespe et al. | 70 | 30 |
During supine roll test; in geotropic nystagmus the rightward horizontal nystagmus is induced by the right-ear-down head position and leftward horizontal nystagmus is induced by the left-ear-down head position with the patient supine. The nystagmus consists of major horizontal and minor torsional components. The nystagmus appears with short latency, lasts for less than a minute and is characterized by an increase followed by a decrease in its intensity. In the apo-geotropic form, there is a right nystagmus when the patient lies on the left side and a left nystagmus when the patient lies on the right side. When the nystagmus is geotropic, the debris is located in the posterior aspect of the canal, and the pathophysiological mechanism is a canalolithiasis. When the nystagmus is apo-geotropic, the mechanism is cupulolitiasis; with the debris attached to the cupula [33, 36]. With respect to the right ear, the cupulolithiasis variant causes ampullofugal movement of fluid in the canal and causes the cupula to signal inhibition when laying on the affected side. This will result in nystagmus beating away from the affected ear (left-beating, in this case). Laying on the unaffected left side, in this example, will cause ampullopetal movement of the fluid and the cupula to be deflected to an excitatory position, causing right-beating nystagmus. The canalithiasis variant, with respect to right ear involvement, will cause the inverse of nystagmus patterns to occur. Laying on the affected right side will cause ampullopetal fluid movement and deflect the cupula to an excitatory position, causing right-beating nystagmus. Whereas laying on the unaffected side will cause ampullofugal movement and the cupula to be put in the inhibitory position, causing left beating nystagmus [37].
The benefit of performing the supine roll test is that it allows clinicians to confirm a diagnosis of lateral semicircular canal BPPV quickly and efficiently. It also allows clinicians to more accurately and comprehensively diagnose positional vertigo that is not due to the posterior canal, whereas without supine roll testing, patients with lateral semicircular canal BPPV might be diagnostically missed if only traditional Dix–Hallpike testing were done [38]. Despite the wide range Effective treatments for lateral semicircular canal BPPV are somewhat predicated on knowing which side is affected, although it is recognized that determining the affected side can be complex. Despite use of supine roll tests and some of its modifications, clear lateralization remains unclear in about 20% of lateral canal BPPV cases. In such situations, one may simply treat one side and then the other. Alternatively, other testing methods, such as the bow and lean procedure maybe applied to add to the diagnosis certainty of side of involvement [18, 19, 38]. In the present study out of 260 patients who were diagnosed with posterior canal BPPV were given Epley manoeuver and Brandt Daroff exercises 258 (99.2%) reported complete resolution of signs and symptoms at 2 weeks follow up. Epleys maneuver is the only recommended method of treating PC-BPPV with confirmed level A evidence according to the American Academy of Neurology with reported success of more than 80 percent after first round of repositioning and success rate further increases with repetition of maneuver which was also correlated with present study [39]. 37 patients of horizontal nystagmus were diagnosed 30 of geotropic and 07 of apo-geotropic.
Though Many physical treatments have been proposed for lateral canal BPPV beginning with barbecue rotation by Lempert but according to a recent evidence-based review of the American Academy of Neurology, all the studies belong to the Class IV level of evidence studies, corresponding to uncontrolled trials, or derived from case reports or from expert opinion [24, 26, 27, 39, 40]. The therapeutic strategy comprises several liberatory manoeuvresmost common being barbecue rotation techniques (Vannucchi-asprella, Lempert), and Gufoni manoeuvre. In a study by Libonati its described that Vannucchi-asprella manoeuvre is preferred as it can immediately solve both geotropic and apogeotropic forms as well as the transformation of some apogeotropic forms into geotropic forms. In their study 85% were treated with Vannucchi asprella maneuver; out of which only 8% geotropic cases required Lempert barbeque rotation and almost 65% of apogeotropic cases were changed to geotropic. In rest 35% cases they employed gufoni maneuver. 98% were solved by first treatment session in Lateral canal BPPV [24], Tirelli and russolo et al. suggested a 360° rotation along longitudinal axis and 51 out of 62 patients getting cured in single sitting. The 360° procedure described by them and used to treat the lateral semicircular canal involved is a variant of the repositioning procedure that is usually performed to treat a posterior canal with debris. For the lateral semicircular canal, they recommended tilting the patient’s head forward 30° while carrying out this 360° CRP. They emphasized that It is important to devise a single, standard treatment procedure that is effective for all the variants of BPPV whether of the lateral semicircular canal or of the posterior semicircular canal, given the practical reality of clinical practice, especially in outpatient clinics staffed by young trainee doctors or nonspecialists [41]. Chiou e al. reported hundred percent resolution of symptoms in their patients by forced prolonged position by having patients lie on side of weaker nystagmus. They reported both the efficacy of maneuver as well as good compliance [42].
In Present study we mainly employed the Vannucchi asprella; Gufoni and Lempert maneuver. The maneuvers were either used alone or in some cases in combination. We could completely cure only 32/37 patients. Most of the apo geotropic cases required more than 5 repetitions except in cases where only Gufoni was used. Gufoni maneuver was very effective in providing immediate relief but it couldn’t be used in anxious patients. In 1 case of Apo-geotropic nystagmus a combination of Vannucchi asprella and lempert was used; Vannucchi asprella in this case converted the Apo-geotropic nystagmus to geotropic and lempert then treated the geotropic component A review of the literature, also, highlights a considerable variety of rehabilitation manoeuvres, each theoretically valid, aimed at achieving the ampullofugal endocanalar progression of the otoconial debris, either by angular accelerations (barbecue rotation techniques), or by sudden linear accelerations (Gufoni liberatory manoeuvre), or through slow gravitational sedimentation (Vannucchi FPP). As none of the manoeuvres proposed, so far, have been successful in almost the totality of the cases, at the first treatment, particularly, as far as concerns the apogeotropic forms we further recommend multi institutional studies with large sample size and control groups for standardising the treatment protocol for Horizontal canal BPPV as is for posterior canal BPPV [24, 42].
Thus, evaluation of the nystagmus on specific canal repositioning tests helps to determine the type of semicircular canal involved in BPPV, with the intensity and direction of nystagmus aiding in determining the involved ear leading to a correct diagnosis. The proper repositioning manoeuvres allow a rapid and simple cure for the BPPV. Therefore to our experience we suggest that it is of outmost importance to diagnose lateral canal involvement if effective treatment of BPPV has to be done.
Conclusion
Lateral canal BPPV is an underdiagnosed entity. Its diagnosis by simple tests is of significance if we really want to improve the results of BPPV management in our clinics where we see how distressing vertigo can be for our patients. There is also a dire need for standardising the management protocols of Lateral canal BPPV as are for posterior canal BPPV so that results can be more valid and reproducible.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Before starting the study Ethical Clearance was taken from the institutional ETHICAL Committee as per DECLARATION OF HELSINKI.
Informed consent
Informed consent was duly taken from all the patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jaskaran Singh, Email: jassigill001@gmail.com.
Bhanu Bhardwaj, Email: entwithdrbhanu@gmail.com.
References
- 1.Hotson JR, Baloh RW. Acute vestibular syndrome. N Engl J Med. 1998;339:680–685. doi: 10.1056/NEJM199809033391007. [DOI] [PubMed] [Google Scholar]
- 2.Bertholon P, Tringali S, Faye MB, Antoine JC, Martin C. Prospective study of positional nystagmus in 100 consecutive patients. Ann Otol Rhinol Laryngol. 2006;115:587–594. doi: 10.1177/000348940611500804. [DOI] [PubMed] [Google Scholar]
- 3.Barany R. Diagnose von krankheitserscheinungen im. Bereiche des otolithenapparates. Acta Otolaryngol. 1921;2:434–437. doi: 10.3109/00016482009123103. [DOI] [Google Scholar]
- 4.Dix MR, Hallpike CS. The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45:341–354. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuknecht HF. Cupulolithiasis. Arch Otolaryngol. 1969;90:765–778. doi: 10.1001/archotol.1969.00770030767020. [DOI] [PubMed] [Google Scholar]
- 6.Parnes LS, McClure JA. Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. 1992;102:988–992. doi: 10.1288/00005537-199209000-00006. [DOI] [PubMed] [Google Scholar]
- 7.McClure JA. Horizontal canal BPV. J Otolaryngol. 1985;14:305. [PubMed] [Google Scholar]
- 8.Casani AP, Vannucci G, Fattori B, Berrettini S. The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112:172–178. doi: 10.1097/00005537-200201000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. J Clin Neurol. 2015;11(3):262–267. doi: 10.3988/jcn.2015.11.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imai T, Takeda N, Ikezono T, Shigeno K, Asai M, Watanabe Y, et al. Classification, diagnostic criteria and management of benign paroxysmal positional vertigo. Auris Nasus Larynx. 2017;44:1–6. doi: 10.1016/j.anl.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Mandala M (2017) How to diagnose and treat BPPV. In: 3rd Congress of the European Academy of Neurology. Amsterdam
- 12.Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol. 1952;61(4):987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K, Hollingsworth DB, Roberts R, Seidman MD, Prasaad Steiner RW, Tsai Do B, Voelker CC, Waguespack RW, Corrigan MD. Clinical practice guideline: benign paroxysmal positional vertigo (update) executive summary. Otolaryngol Head Neck Surg. 2017;156(3):403–416. doi: 10.1177/0194599816689660. [DOI] [PubMed] [Google Scholar]
- 14.Ranalli P. An overview of central vertigo disorders. Adv Otorhinolaryngol. 2019;82:127–133. doi: 10.1159/000490281. [DOI] [PubMed] [Google Scholar]
- 15.Balatsouras DG, Koukoutsis G, Ganelis P, Korres GS, Kaberos A. Diagnosis of single- or multiple-canal benign paroxysmal positional vertigo according to the type of nystagmus. Int J Otolaryngol. 2011;2011:483965. doi: 10.1155/2011/483965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steddin S, Ing D, Brandt T. Horizontal canal benign paroxysmal positioning vertigo (h-BPPV): transition of canalolithiasis to cupulolithiasis. Ann Neurol. 1996;40:918–922. doi: 10.1002/ana.410400615. [DOI] [PubMed] [Google Scholar]
- 17.Shin JE, Jeong KH, Ahn SH, et al. Change of nystagmus direction during a head-roll test in lateral semicircular canal cupulolithiasis. Auris Nasus Larynx. 2017;44:227–231. doi: 10.1016/j.anl.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Choung Y, Shin YR, Kahng H, Park K, Choi SJ. ‘Bow and lean test’ to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116:1776–1781. doi: 10.1097/01.mlg.0000231291.44818.be. [DOI] [PubMed] [Google Scholar]
- 19.Lee JB, Han DH, Choi SJ, Park K, Park HY, Sohn IK, Choung Y. Efficacy of the “bow and lean test” for the management of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2010;120:2339–2346. doi: 10.1002/lary.21117. [DOI] [PubMed] [Google Scholar]
- 20.Korres SG, Balatsouras DG, Papouliakos S, Ferekidis E. Benign paroxysmal positional vertigo and its management. Med Sci Monit. 2007;13(6):275–282. [PubMed] [Google Scholar]
- 21.Califano L, Salafia F, Mazzone S, Melillo MG, Califano M. Anterior canal BPPV and apogeotropic posterior canal BPPV: two rare forms of vertical canalolithiasis. Acta Otorhinolaryngol Ital. 2014;34(3):189–197. [PMC free article] [PubMed] [Google Scholar]
- 22.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 23.Lempert T, Tiel-Wilck K, Positional A. Maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope. 1996;106(4):476–478. doi: 10.1097/00005537-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Asprella Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. 2005;25(5):277–283. [PMC free article] [PubMed] [Google Scholar]
- 25.Gufoni M, Mastrosimone L, Di Nasso F. Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal. Acta Otorhinolaryngol Ital. 1998;18(6):363–367. [PubMed] [Google Scholar]
- 26.Casani AP, Vannucci G, Fattori B, et al. The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112:172–178. doi: 10.1097/00005537-200201000-00030. [DOI] [PubMed] [Google Scholar]
- 27.Fife TD. Recognition and management of horizontal canal benign paroxysmal positional vertigo. Am J Otol. 1998;19:345–351. doi: 10.1016/S0196-0709(98)90012-6. [DOI] [PubMed] [Google Scholar]
- 28.Steenerson RL, Cronin GW, Marbach PM. Effectiveness of treatment techniques in 923 cases of benign paroxysmal positional vertigo. Laryngoscope. 2005;115:226–231. doi: 10.1097/01.mlg.0000154723.55044.b5. [DOI] [PubMed] [Google Scholar]
- 29.Honrubia V, Baloh RW, Harris MR, et al. Paroxysmal positional vertigo syndrome. Am J Otol. 1999;20:465–470. [PubMed] [Google Scholar]
- 30.Macias JD, Lambert KM, Massingale S, et al. Variables affecting treatment in benign paroxysmal positional vertigo. Laryngoscope. 2000;110:1921–1924. doi: 10.1097/00005537-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 31.Korres SG, Balatsouras DG. Diagnostic, pathophysiologic, and therapeutic aspects of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2004;131:438–444. doi: 10.1016/j.otohns.2004.02.046. [DOI] [PubMed] [Google Scholar]
- 32.Korres S, Balatsouras DG, Kaberos A, Economou C, Kandiloros D, Ferekidis E. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23(6):926–932. doi: 10.1097/00129492-200211000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Nuti D, Vannucchi P, Pagnini P. Lateral canal BPPV: which is the affected side? Audiol Med. 2005;3(1):16–20. doi: 10.1080/16513860510028275. [DOI] [Google Scholar]
- 34.Bertholon P, Faye MB, Tringali S, et al. Benign paroxysmal positional vertigo of the horizontal canal. Clinical features in 25 patients. Ann Otolaryngol Chir Cervicofac. 2002;119:73–80. [PubMed] [Google Scholar]
- 35.Waespe W. Benign positional vertigo and nystagmus of the horizontal semicircular canal. Schweiz Med Wochenschr. 1997;127:287–295. [PubMed] [Google Scholar]
- 36.Vannucchi P, Pecci R. About nystagmus transformation in a case of apogeotropic lateral semicircular canal benign paroxysmal positional vertigo. Int J Otolaryngol. 2011;2011:4. doi: 10.1155/2011/687921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kurtzer DA, Gans RE, McLeod H. New horizontal canal benign paroxysmal positional vertigo treatment: kurtzer hybrid maneuver. Glob J Otol. 2017;6(3):555686. doi: 10.19080/GJO.2017.06.555686. [DOI] [Google Scholar]
- 38.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Corrigan MD. Clinical practice guideline: benign paroxysmal positional vertigo (update) Otolaryngol Head Neck Surg. 2017;156(3):S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 39.Fife TD, Iverson DJ, Lempert T, Furman JM, Baloh RW, Tusa RJ, et al. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70:2067–2074. doi: 10.1212/01.wnl.0000313378.77444.ac. [DOI] [PubMed] [Google Scholar]
- 40.Nuti D, Mandalà M, Salerni L. Lateral canal paroxysmal positional vertigo revisited. Ann NY Acad Sci. 2009;1164:316–323. doi: 10.1111/j.1749-6632.2008.03720.x. [DOI] [PubMed] [Google Scholar]
- 41.Tirelli G, Russolo M. 360-Degree canalith repositioning procedure for the horizontal canal. Otolaryngol Head Neck Surg. 2004;131:740–746. doi: 10.1016/j.otohns.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 42.Chiou WY, Lee HL, Tsai SC, Yu TH, Lee XX. A single therapy for all subtypes of horizontal canal positional vertigo. Laryngoscope. 2005;115:1432–1435. doi: 10.1097/01.mlg.0000168092.91251.d3. [DOI] [PubMed] [Google Scholar]