To the Editor,
In December 2019, novel coronavirus 2019 has appeared in China. On 11 February 2020, the World Health Organization officially name the disease as COVID‐19. 1 The new coronavirus is highly contagious. The rapid spread of SARS‐CoV‐2 leads to declaring the pandemic on the 11 March 2020. On 10 May 2020 the number of infected people is 4 132 373 worldwide. 2 The main transmission mode it is through the droplets: by contact or transmission of aerosols. Furthermore, there are doubts regarding the maternal‐infant vertical transmission. 1 , 3 In this overwhelming scenario, new challenges have to be faced, such as COVID‐19 in pregnant women and puerperant. The separation between an infected mother and her baby due to the need for an organizational simplification during a novel emergency does not allow breastfeeding. The use of expressed breast milk for is a valid strategy to continue breastfeeding in security. 3 No clear indications are available on preterm management in the neonatal intensive care unit (NICU) setting during the COVID‐19 pandemic. In this paper, we reported the case of a mother who presented clinical symptoms of respiratory tract infection 10 days after the spontaneous delivery of a preterm newborn. The woman delivered a female neonate at 32 weeks of gestational age, with birth weight appropriate for age. At birth, the newborn received noninvasive ventilatory support (nCPAP) with FiO2 = 0.25. She was admitted to the Neonatology ward, where noninvasive ventilation was stopped at 24 hours of age. Since birth, the newborn was fed with both breastfeeding and expressed maternal milk, and received Kangaroo Mother Care sessions. Eleven days apart from the delivery, the mother developed fever, anosmia, and generalized malaise. Taking into account her provenience from a high‐risk area, reverse transcription polymerase chain reaction (RT‐PCR) assay for SARS‐CoV‐2 acid nucleic on mother nasopharyngeal swab was performed, resulting in positive (Department of Medicine and Surgery, Hygiene and Public Health Laboratory, University of Parma). In contrast, RT‐PCR assay on breast milk, pumped at the symptoms' onset, was negative for SARS‐CoV‐2, allowing the prosecution of nutrition with expressed maternal milk. The neonate showed a good clinical course with normal vital parameters and grew up regularly. She was discharged with a weight gain of 910 g more than the birth weight. Timeline of length stay in hospital is reported in Figure 1.
Figure 1.
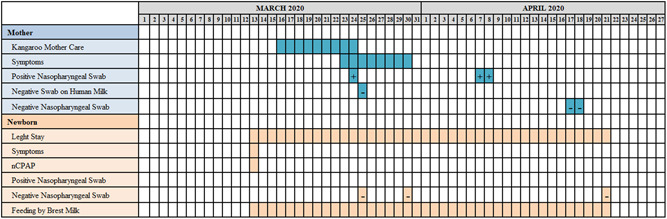
Timeline of clinical length stay of the mother‐baby dyade. + = positive swab; – = negative swab
During a stay in the hospital, mother and healthcare caregivers applied recommended hygiene measures, consisting of wearing surgical‐mask, hand washing, and using alcohol‐based solutions to clean the surfaces. In this setting, no horizontal transmission occurred. Moreover, RT‐PCR assay for SARS‐CoV‐2 performed on breast milk during mother febrile peak was negative. This is in line with recent studies, RT‐PCR assays on breast milk samples collected from affected women result negative for SARS‐CoV‐2. 4 , 5 In our intensive neonatal care unit the facility's ability to accommodate mother‐baby separation or colocation is lacking. Mother passed her quarantine at home. The decision regarding mother‐baby separation was shared between the mother and the clinical team. Breastfeeding is important to the health and wellbeing of newborns and the protective impact of breastfeeding against infectious disease is of particular interest in the context of pandemics. The protective impact of breast milk against infectious lies in its components: immunoglobulins, lactoferrin, lysozyme, functional macrophages lymphocytes and monocytes, probiotic organisms and oligosaccharides. 6 Breast milk would provide IgA antibodies to structural virus protein which could play a role in suppressing the replication of virus. 7 Probiotic organisms and oligosaccharides support “good” colonization of the intestinal tract and suppress the growth of pathogenic bacteria. Growth factors in breastmilk also assist in the maturation of the infant's own immune system. Favre et al 8 suggest that SARS‐CoV‐2 positive mothers must be isolated from newborns until viral shedding clears. However, any physical distance between mothers and infants impair the establishment of breastfeeding and bonding. The resourcing and other requirements associated with separating and isolating mothers' and infants needs also to be considered. Salvatori et al 4 reported a case series in which both the two mothers and two full‐term babies were SARS‐CoV‐2 positive and stay in a rooming‐in setting. Postnatal horizontal COVID‐19 infection occurred in newborns but expressed breast milk analysis did not reveal traces of the virus, so breastfeeding continued and the dyad was not separate. Lack of mother‐to‐baby transmission, when the mother was infected before delivery of baby were also reported. 9 , 10
Here we describe a case of preterm baby breastfeeding mother at 11 days postpartum COVID‐19 affected, in a NICU setting. The adherence to hygiene measures by health workers and newborn parents, in addition to the paths implemented for the management of positive COVID‐19 patients, contributes to infection control and its spreading prevention.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
PS made substantial contributions to the study concept and design. GM was in charge of the manuscript draft. MA, DM, FM, and GM, took responsibility for obtaining written consent from patients, collecting samples, and confirming data accuracy. PL and SM made substantial contributions to data acquisition, analysis, and interpretation. ES critically revised the manuscript for important intellectual content.
REFERENCES
- 1. Hong H, Wang Y, Chung HT, Chen CJ. Clinical characteristics of novel coronavirus disease 2019 (COVID‐19) in newborns, infants and children. Pediatr Neonatol. 2020;61(2):131‐132. 10.1016/j.pedneo.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Worldometer . Covid‐19 Coronavirus Pandemic . https://www.worldometers.info/coronavirus/. Accessed May 10, 2020.
- 3. Davanzo R. Breast feeding at the time of COVID‐19: do not forget expressed mother's milk, please. Arch Dis Child Fetal Neonatal Ed. 2020:319149. 10.1136/archdischild-2020-319149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salvatori G, De Rose DU, Concato C, et al. Managing COVID‐19‐positive maternal‐infant dyads: an Italian experience. Breastfeed Med. 2020;15:347‐348. 10.1089/bfm.2020.0095 [DOI] [PubMed] [Google Scholar]
- 5. Dashraath P, Wong JLJ, Lim MXK, et al. Coronavirus disease 2019 (COVID‐19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;S0002‐9378(20):30343‐30344. 10.1016/j.ajog.2020.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Andreas NJ, Kampmann B, Mehring Le‐Doare K. Human breast milk: a review on its composition and bioactivity. Early Hum Dev. 2015;91:629‐635. 10.1016/j.earlhumdev.2015.08.013 [DOI] [PubMed] [Google Scholar]
- 7. Tsutsumi H, Honjo T, Nagai K, Chiba Y, Chiba S, Tsugawa S. Immunoglobulin A antibody response to respiratory syncytial virus structural proteins in colostrum and milk. J Clin Microbiol. 1989;27(9):1949‐1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Favre G, Pomar L, Qi X, Nielsen‐Saines K, Musso D, Baud D. Guidelines for pregnant women with suspected SARS‐CoV‐2 infection. Lancet Infect Dis. 2020. 10.1016/S1473-3099(20)30157-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhu H, Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mother with 2019‐nCoV pneumonia. Transl Pediatr. 2020;9:51‐60. 10.21037/tp.2020.02.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yan J, Guo J, Fan C, et al. Coronavirus disease 2019 (COVID‐19) in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020;S0002‐9378(20):30462‐2. 10.1016/j.ajog.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]


