Dear Editor,
Many hospitals radically changed their organization during the COVID-19 pandemic to face the capacity and resources limitations of intensive care units (ICUs). Scheduled activities were suddenly stopped, allowing for massive reassignments of volunteers. At the University Hospital of Nancy, 15 specific medical teams (75 volunteers) were created to cope with the large number of patients with severe COVID-19-related acute respiratory distress syndrome (ARDS) and requiring prone positioning (PP).
The PP procedure is of crucial importance for severe ARDS patients [1], especially when related to COVID-19 [2]. Although turning a patient into the prone position is not an invasive procedure, it is complex and has many potential adverse effects requiring adequate and well-trained staff. It is also an exhausting and time-consuming task for ICU staff under stressful conditions. Therefore, at the University Hospital of Nancy, dedicated medical teams helped intensivist physicians strictly follow PP guidelines, thereby ensuring the full medical care for critical ARDS patients. Each PP team (PPT) consisted of 1 non-intensivist senior physician, 2 residents, and 2 medical students. Volunteers were trained in a simple ad-hoc training session consisting of 3 to 6 real PP procedures supervised by permanent physicians and nurses of the ICU.
PPTs were deployed from March 23 to April 24, 2020, in an extended ICU (from 22 to 46 beds). During this period, they performed a mean [SD] of 11.5 [3.4] placements per day, with up to 23 placements (PP or its opposite, supine positioning [SP]) at the surge of the outbreak on April 3. Overall, more than 350 placements were performed during this month, corresponding to a total manipulated weight > 30 tons. The PP task is not only physically difficult but also a risk factor for back injuries due to recurrent forward-bending postures.
To deal with this repetitive and depleting task, we investigated whether the use of back-support exoskeletons was helpful and feasible in the context of an ICU facing the CODIV-19 pandemic.
Our pilot study consisted of two steps: first, an exploratory study with whole-body kinematics assessment and evaluation of potential exoskeletons, carried out under simulated conditions, then implementation in a real-life situation with the selected exoskeletons. The exploratory study was carried out at the Hospital Simulation Center of the University of Lorraine.
We recorded the whole-body kinematics of one experienced PPT volunteer (male, 35 years old, 175 cm) by using the Xsens inertial motion capture system. Postural analysis of the PP maneuver without an exoskeleton revealed that the teammate on the side of the patient spends approximately 40% of the time with the torso bent more than 20 degrees forward, whereas the teammate behind the manikin's head maintains a static posture with substantial flexion of the trunk for several minutes to secure the patient's head and avoid extubation. Even when not associated with load manipulation, such postures cause mechanical load on the lower back [3]. These preliminary results confirmed that the use of an exoskeleton for lumbar support is fully justified.
We examined 4 commercial exoskeletons designed to unload the lumbar spine in order to select the one that appropriately met the requirements of the PP maneuver: CORFOR (CORFOR, France), Laevo v1 (Laevo, The Netherlands), BackX (SuitX, USA), and CrayX (German Bionics, Germany). CORFOR is a passive soft exoskeleton (known as an exosuit), Laevo and BackX are passive rigid exoskeletons based on springs, and CrayX is an active exoskeleton involving electrical actuators. Five experienced PPT volunteers performed 11 PP/SP maneuvers with a 100-kg manikin (Fig. 1 ). Two of the participants (male, 30 and 35 years old) tried all 4 exoskeletons.
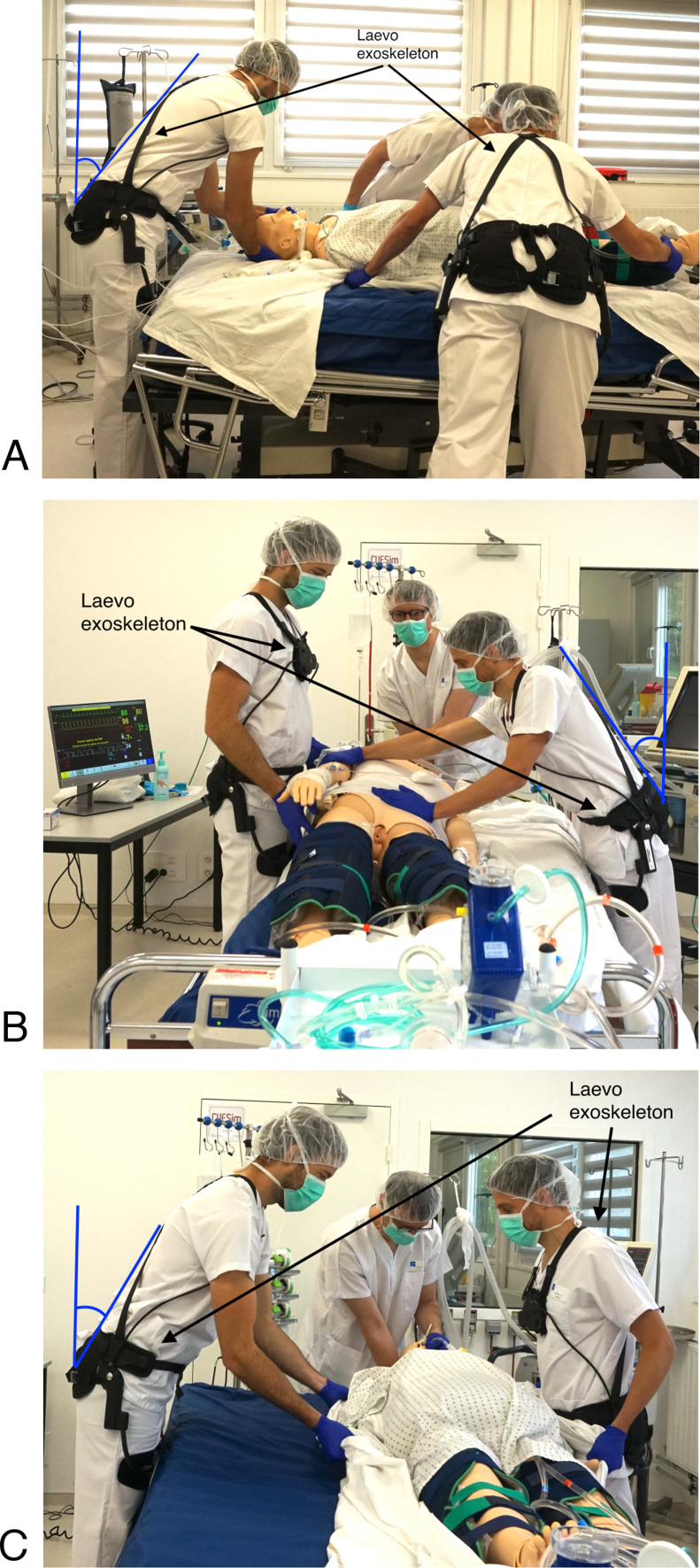
Fig. 1.
Typical postures assumed by medical staff during the prone positioning/supine positioning (PP/SP) maneuver. A. Static forward bending to secure the patient's head. B. Forward trunk flexion during SP. C. Forward trunk flexion during repositioning of the patient on the bed. The photos were taken at the Hospital Simulation Center of the University of Lorraine. Two volunteers are equipped with the Laevo exoskeleton.
After testing each exoskeleton, these 2 participants completed a technology acceptance questionnaire adapted from [4] to evaluate the perceived effort, safety, comfort, efficacy, installation, and intention to use. Each construct of the questionnaire regroups several items on a 5-point Likert scale, with 1 indicating “strongly negative” and 5 “strongly positive”; 3 is the neutral answer. The reported scores are described according to the mean [SD] of all questions related to each construct (safety, comfort, usability, etc.). The participants also reported on their experience in a semi-directed interview.
Both participants perceived a reduction in physical effort when using all exoskeletons except CORFOR (3.0 [0.0] vs Laevo, BackX and CrayX: 4.0 [0.0]). All exoskeletons were scored positively in terms of perceived safety and comfort (CORFOR: 4.37 [0.7]; Laevo: 4.5 [0.5]; BackX: 4.0 [1.1]; CrayX: 3.8 [1.0]), and the participants did not notice a change in their efficacy, positive or negative, while using the exoskeletons. Laevo was the easiest to install (CORFOR: 3.5 [2.1]; Laevo: 4.5 [0.7]; BackX: 1.5 [0.7]; CrayX: 1.5 [0.7]) and had the highest and only positive score in the intention-to-use construct (CORFOR: 3.0 [0.0]; Laevo: 4.5 [0.7]; BackX: 2.5 [0.7); CrayX: 3.0 [0.0]).
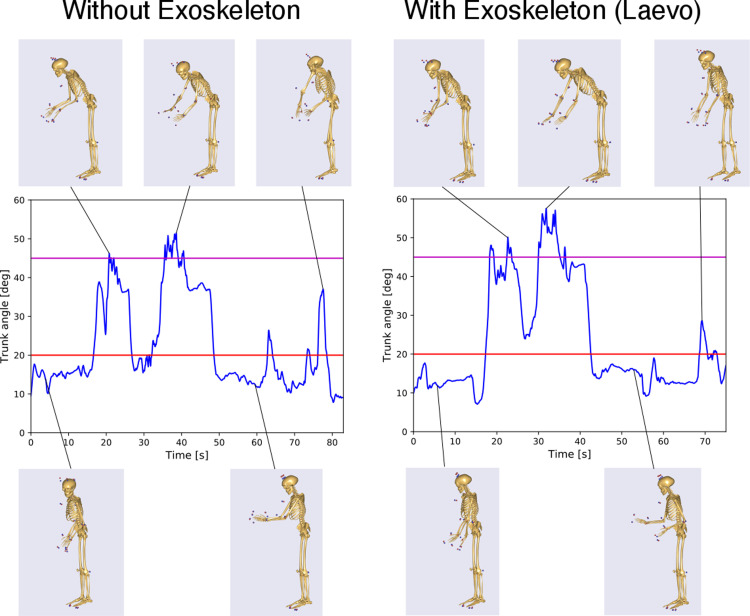
Both participants reported that CrayX was too cumbersome to wear in an ICU, whereas the mechanical design of BackX unpleasantly hindered several arm movements of the PP maneuver. CORFOR was not helpful. Conversely, participants were satisfied with Laevo in terms of perceived assistance during bent postures, ease of use, and freedom of movement. Importantly, they mentioned that Laevo did not modify their movements during the PP maneuver, which was confirmed by the analysis of the kinematic data (Fig. 2 ).
Fig. 2.
Trunk flexion angle during a typical PP maneuver without (left) and with (right) the assistance of the Laevo exoskeleton, recorded at the Hospital Simulation Center. Angles above 20 degrees (red line on the graph) are considered risky for ergonomics when maintained or repeated; values greater than 45 degrees (magenta line) indicate postures with severe risk. The overall similarity of the 2 graphs suggests that the PP maneuver is not substantially affected by the use of the exoskeleton. This observation agrees with the subjective report of the participants. The angles were computed with the AnyBody biomechanical modelling software, using the Xsens MVN recordings of the movement realized by one participant (male, 35 years old, 175 cm).
Building upon these promising pilot results and given the urgency associated with the COVID-19 crisis, we proceeded to test under real-life conditions to demonstrate the feasibility of using Laevo in a COVID-19 ICU situation. The same 2 volunteers were each equipped with a Laevo in a way that complies with the drastic hygiene rules of the ICU during the outbreak. During a typical 3-hr shift, they performed 10 PP maneuvers on ICU patients, each volunteer positioned 3 times at the head and 7 times at the patient's side. After each maneuver, the participants reported their perceived effort on a Borg-CR10 (0–10) scale. At the end of the shift, they completed an extended version of the same questionnaire used in the simulated environment and reported on their experience in an interview. Concomitantly, the PPT colleagues completed a questionnaire to report on their experience working alongside the people wearing exoskeletons.
Overall, the evaluation of Laevo was positive in terms of physical relief (questionnaire score: 4.2 [0.4]): both participants reported that the perceived general fatigue at the end of the shift was reduced when using Laevo. Importantly, they both said they would use Laevo again without hesitation for future shifts when they would be positioned at the patient's head (effort score on Borg-CR10 scale: head: 1.8 [0.4]; side: 3.2 [0.7]).
Cardiac activity of the 2 participants was monitored with a Holter-ECG during the whole shift in the ICU. Unfortunately, the analysis of the ECG data was inconclusive because of the multiple biases in this real-life condition, such as the elevated stress of the participants due to the COVID-19 context and the frequency of multiple gestures performed during the PP maneuver preventing the precise characterization of the help of exoskeleton in terms of heart rate data. Although we could not reliably measure the physiological and biomechanical effects of Laevo in the ICU, we expect beneficial effects such as those reported by previous laboratory studies with similar postures [5], [6].
The participants found Laevo comfortable (questionnaire score: 4.5 [0.5]), except when walking, which is a well-known issue of Laevo v1 [7] that was improved in recent versions. Laevo did not prevent or constrain the usual gestures and activity in the ICU. Accordingly, their teammates did not notice any particular changes in the practice, and no physical or psychological side effects were observed. These results are important for a potential adoption of Laevo by the PPT in current practice because the positive attitude of co-workers is fundamental for the acceptance of a new technology at work [8].
The use of exoskeletons to cope with an exhausting task such as prone positioning in the ICU to safely maintain a large number of patients on mechanical ventilation during the surge of the COVID-19 outbreak is a consistent topic of research. Our pilot study showed that using an exoskeleton to assist medical staff could be helpful and be readily feasible, even in the dreadful context of the COVID-19 pandemic.
Previous studies generally agree on the efficiency of passive back-support exoskeletons to reduce lumbar muscular activity and perceived exertion/discomfort, particularly during operations involving trunk flexion/extension in the sagittal plane [9], [10]. However, although occupational exoskeletons are deployed in the industrial sector [11], their use in the healthcare system is rarely reported, with no reported use in ICUs.
The medical staff using the passive exoskeleton Laevo during the PP maneuvers in the ICU perceived physical relief in the low back during bent postures, particularly when working at the patient's head. Subjective evaluation, which is used in field studies to evaluate the adoption of exoskeletons in industry [12], indicates an intention to adopt such a technology after this pilot study, although limited by the small number of participants.
Before a potential standardization, further studies are needed to clarify the indications and beneficial effects of this artificial help for PP maneuvers, particularly with validated physiological measures that can be used in the ICU.
Funding
The work was partly funded by the European Commission through the project H2020 AnDy (GA no. 731540), Nancy University Hospital, and Hôpital Virtuel de Lorraine.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgments
The authors thank all the members of the project “ExoTurn” that allowed for realizing this pilot study and their respective institutions for their support: Antoine Didelot, Silvère Barde, Sergueï Malikov, Jean Marc Sellal, Agnes Aublet-Cuvelier and Lien Wiolande.
References
- 1.Guérin C., Reignier J., Richard J.C., Beuret P., Gacouin A., Boulain T. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 2.Wilson K.C., Chotirmall S.H., Bai C., Rello J., On behalf of the International Task Force on COVID-19 . 2020. COVID-19: Interim Guidance on Management Pending Empirical Evidence. From an American Thoracic Society-led International Task Force. [Google Scholar]
- 3.Hoogendoorn W.E., Bongers P.M., de Vet H.C., Douwes M., Koes B.W., Miedema M.C. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: results of a prospective cohort study. Spine. 2000;25:3087–3092. doi: 10.1097/00007632-200012010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Wioland L., Debay L., Atain-Kouadio J.-J. 2019. Processus d’acceptabilité et d’acceptation des exosquelettes: évaluation par questionnaires. Références en santé au travail, TF 274, no 160; pp. 49–76. http://www.inrs.fr/dms/inrs/CataloguePapier/DMT/TI-TF-274/tf274.pdf. [Google Scholar]
- 5.Bosch T., van Eck J., Knitel K., de Looze M. The effects of a passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Appl Ergon. 2016;54:212–217. doi: 10.1016/j.apergo.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Koopman A.S., Kingma I., Faber G.S., de Looze M.P., van Dieën J.H. Effects of a passive exoskeleton on the mechanical loading of the low back in static holding tasks. J Biomech. 2019;83:97–103. doi: 10.1016/j.jbiomech.2018.11.033. [DOI] [PubMed] [Google Scholar]
- 7.Baltrusch S.J., van Dieën J.H., Bruijn S.M., Koopman A.S., van Bennekom C.A.M., Houdijk H. The effect of a passive trunk exoskeleton on metabolic costs during lifting and walking. Ergonomics. 2019;62:903–916. doi: 10.1080/00140139.2019.1602288. [DOI] [PubMed] [Google Scholar]
- 8.Maurice P., Allienne L., Malaise A., Ivaldi S. 2018. Ethical and Social Considerations for the introduction of Human-Centered Technologies at Work. IEEE Workshop on Advanced Robotics and its Social Impacts (ARSO) [Google Scholar]
- 9.Nussbaum M.A., Lowe B.D., de Looze M., Harris-Adamson C., Smets M. An Introduction to the Special Issue on Occupational Exoskeletons. IISE Trans Occup Ergon Hum Factors. 2019;7:153–162. doi: 10.1080/24725838.2019.1709695. [DOI] [Google Scholar]
- 10.Theurel J., Desbrosses K. Occupational Exoskeletons: Overview of Their Benefits and Limitations in Preventing Work-Related Musculoskeletal Disorders. IISE Trans Occup Ergon Hum Factors. 2019;7:264–280. doi: 10.1080/24725838.2019.1638331. [DOI] [Google Scholar]
- 11.De Looze M.P., Bosch T., Krause F., Stadler K.S., O'Sullivan L.W. Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics. 2016;59:671–681. doi: 10.1080/00140139.2015.1081988. [DOI] [PubMed] [Google Scholar]
- 12.Hensel R., Keil M. Subjective Evaluation of a Passive Industrial Exoskeleton for Lower-back Support: A Field Study in the Automotive Sector. IISE Trans Occup Ergon Hum Factors. 2019;7:213–221. doi: 10.1080/24725838.2019.1573770. [DOI] [Google Scholar]