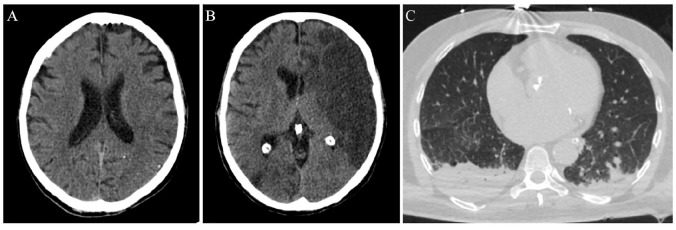
Figure 1.
Imaging evaluation of an ischemic stroke patient with concomitant COVID-19.
This 53-year-old man presented in the emergency department of a comprehensive stroke centre on March 18, 2020. The patient was aphasic with right hemiplegia. The National Institute of Health Stroke Scale (NIHSS) score was 16. He was afebrile and his family members denied any symptoms attributable to COVID-19. Neurological symptoms’ onset-to-presentation time was 1 h. A non-contrast brain computed tomography (CT)-scan was performed, intracranial haemorrhage was excluded and early hyperacute signs of left middle cerebral artery ischemia were disclosed (loss of grey-white matter differentiation (A). No other contraindications existed and intravenous thrombolysis with alteplase was administered. Door-to-needle time was relatively prolonged (70 min), since the CT-scan was occupied at that time with chest examinations of patients with possible SARS-CoV-2 infection. There was no availability for mechanical thrombectomy in this institution (after-hours presentation of the patient and limited personnel in the catheter laboratory). Diagnostic work-up revealed two possible stroke mechanisms: atrial fibrillation of unknown duration with subsequent cardio-embolism, and concomitant atherothrombotic disease, causing haemodynamically significant (>70%) stenosis of the internal carotid arteries bilaterally. During the next 48 h, the patient presented neurological deterioration (NIHSS-score of 22) and follow-up brain CT showed an extensive infarction in the distribution of the left middle cerebral artery (B). At that time, the patient developed a low-grade fever, most probably due to aspiration. Chest CT-scan was indicative of bilateral aspiration pneumonia (C). Oropharyngeal swabs were also examined for SARS-CoV-2 on RT-PCR assay, but the virus was not detected. Three days later, the patient was intubated and transferred to the general intensive care unit. The second oropharyngeal swab test was positive for SARS-CoV-2 RNA. The patient expired on March 24, 2020 due to further neurological deterioration from cerebral oedema.