Abstract
Covid-19 is a viral disease that has spread throughout the world causing unprecedented impact on millions of people. It's a pandemic disease called officially by the World Health Organization in March 11, 2020. The disease mainly involves the upper respiratory tract system. Extrapulmonary manifestations are still not well understood. In this report, we describe a case of acute pancreatitis in a patient with Covid-19 infection who presented to our hospital.
Keywords: COVID-19, coronavirus disease 2019; RT-PCR, reverse transcription polymerase chain reaction; CT, computed tomography; CECT, contrast enhanced computed tomography; ED, emergency department
Abbreviations: CT, computed tomography; CECT, contrast enhanced computed tomography; COVID-19, coronavirus disease 2019; RT-PCR, Reverse transcription polymerase chain reaction; ED, emergency department; H1N1, Hemagglutinin Type 1 and Neuraminidase Type 1
Case report
A 24-year-old man presented to our emergency department (ED) with a nonradiating sharp, epigastric pain for the last 2 days. It was associated with nausea and vomiting. He denied fever, chills and diarrhea. Review of systems was otherwise unremarkable. There was no history of alcohol consumption. The patient was diagnosed with COVID-19 by nasopharyngeal reverse transcription-polymerase chain reaction 1 day prior to presentation to the ED. He had mild upper respiratory tract symptom. His oxygen saturation was 100% in room air and his chest X-ray was negative. He didn't require any treatment for his COVID-19 infection. He was otherwise healthy without any prior medical or surgical history.
The physical examination of the patient was performed in the ED and showed nondistended, soft abdomen with epigastric discomfort on palpation. No palpable mass. No signs of jaundice or dehydration.
The laboratory tests were ordered which showed elevated lipase (578 IU/L) as well as amylase (391 units/L).
Diagnostic radiology imaging including ultrasound and enhanced CT scan were ordered and reveled no biliary stones and mild pancreatitis (discussed below in details).
The patient was admitted under general surgery and was treated conservatively. He was also monitored by COVID-19 team for any deterioration in symptoms.
The patient remained vitally stable with improving symptoms during hospital stay. He was accordingly discharged after 3 days and advised to return to ED if the symptoms reappear.
Imaging findings
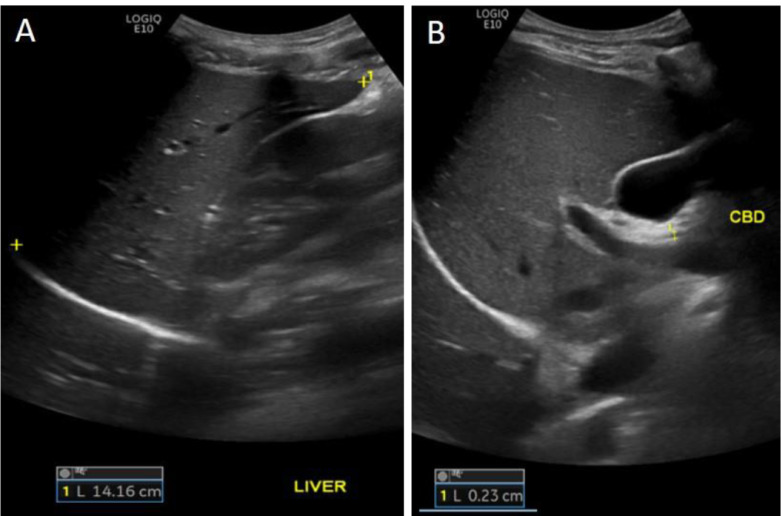
An abdomen ultrasound showed normal liver echogenicity with no focal lesion (Fig. 1).
Fig. 1.
Ultrasound of the abdomen showing normal liver appearance (A), gallbladder and CBD with no stones (B).
Normal gallbladder wall, no stones, normal CBD diameter (Fig. 2).
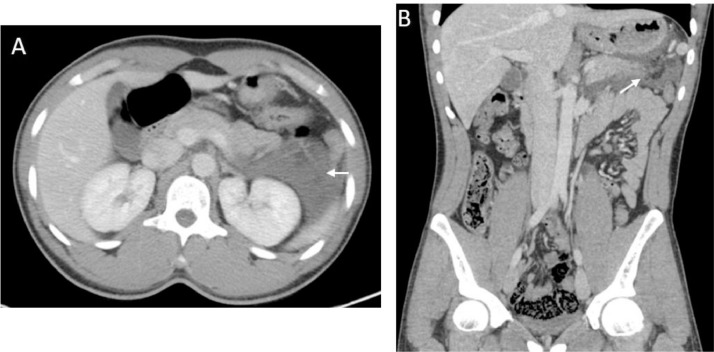
Fig. 2.
Postcontrast CT scan axial (A) and coronal images (B), showing edema of the distal pancreas with surrounding fluid (arrow).
An abdominopelvic computed tomography (CT) with IV contrast (potovenous phase) was performed, axial (Fig. 1) and coronal reformation (Fig. 2), which revealed a mild edema of the distal pancreas with a non-encapsulated peripancreatic low density fluid around pancreatic tail extending to the splenorenal recess (arrow). The pancreas showed normal enhancement with no necrosis or abscess formation. No portal or splenic vein thrombosis.
Discussion
There are many causes of acute pancreatitis in adults. Passage or impaction of gallstones remain the main cause. Other causes may include alcohol abuse, metabolic disorders, autoimmune diseases, drugs and toxins. Viruses such as mumps, Coxsackie B, measles, Epstein–Barr and hepatitis A, B, and E can also cause acute pancreatitis. Few cases that suggest association between H1N1 influenza and acute pancreatitis have been reported [1,4]. One study has also suggested a direct impact of COVID19 infection on the pancreas [7].
Pancreatic injury in COVID-19 might be caused directly by viral involvement or secondary from enzyme abnormalities in the context of severe illness without substantial pancreatic injury [5].
The diagnosis depends usually on the clinical parameters; however, imaging plays an important role in aiding the diagnosis whenever the clinical picture is unclear. It also helps in detecting possible causes, complications, and to assess disease severity based on imaging scoring systems.
Contrast enhances computed tomography provides over 90% sensitivity and specificity for the diagnosis of acute pancreatitis [2].
Based on Atlanta classification of acute pancreatitis, which is an international multidisciplinary classification of the severity of acute pancreatitis, the severity of acute pancreatitis can be divided into interstitial edematous pancreatitis or necrotizing pancreatitis [6].
Early aggressive intravenous fluid resuscitation provides micro- and microcirculatory support to prevent serious complications such as pancreatic necrosis [3].
Conclusion
Although acute pancreatitis is not an uncommon condition, this case report suggest possibility of a rare and direct causal relation between COVID-19 infection and acute pancreatitis. This can aid physicians in decision making, predicting COVID-19 as a possible cause.
References
- 1.Agzarian, A. and Agzarian, A. (n.d.). Influenza A as a cause of acute pancreatitis: a case report. [online] Available at: https://proceedings.med.ucla.edu/wp-content/uploads/2016/11/A160816AA-WH-edited.pdf[Accessed 18 May 2020].
- 2.Banks P.A., Freeman M.L. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101(10):2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 3.Gardner T.B., Vege S.S., Pearson R.K., Chari S.T. Fluid resuscitation in acute pancreatitis. Clin Gastroenterol Hepatol. 2008;6(10):1070–1076. doi: 10.1016/j.cgh.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Habib A., Jain A., Singh B., Jamshed N. H1N1 influenza presenting as severe acute pancreatitis and multiorgan dysfunction. Am J Emerg Med. 2016;34(9):1911. doi: 10.1016/j.ajem.2016.01.019. https://www.ajemjournal.com/article/S0735-6757(16)00029-2/pdf [online]e1–1911.e2. Available at. [Accessed 18 May 2020] [DOI] [PubMed] [Google Scholar]
- 5.Liu, F., Long, X., Zou, W., Fang, M., Wu, W., Li, W., et al (2020). Highly ACE2 expression in pancreas may cause pancreas damage after SARS-CoV-2 infection. [DOI] [PMC free article] [PubMed]
- 6.Thoeni R.F. The revised atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012;262(3):751–764. doi: 10.1148/radiol.11110947. [DOI] [PubMed] [Google Scholar]
- 7.Wang F., Wang H., Fan J., Zhang Y., Wang H., Zhao Q. Pancreatic injury patterns in patients with COVID-19 pneumonia. Gastroenterology. 2020;5:434–435. doi: 10.1053/j.gastro.2020.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]