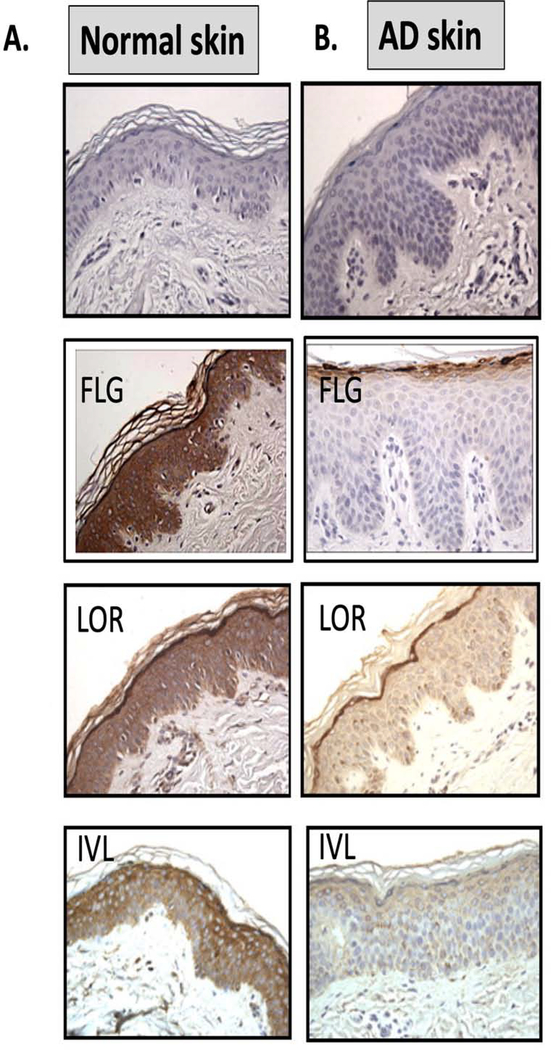
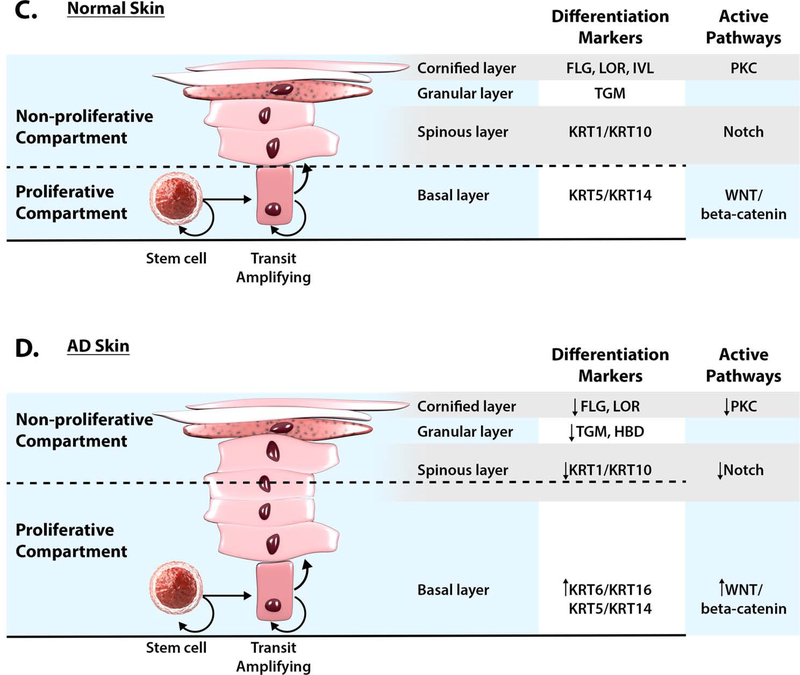
Figure 2. Lack of Keratinocyte Terminal Differentiation in Atopic Dermatitis.
Abnormalities in keratinocyte differentiation in AD skin result in hyperplasia of the basal layer, reduction of spinous layer and inhibition of markers of terminal differentiation (FLG, IVL, LOR) in AD (B) as compared to NA skin (A) (reproduction with permission from reference 4 and reference 134). Schematic of epidermal differentiation pattern in normal (C) and AD skin (D) is shown. The keratinocyte differentiation process is an integrated multi-step program of sequential changes in gene expression and cell structure, as the cells migrate from the proliferative basal layer, through spinous and granular layers, into the cornified layer, which functions as a skin barrier. Cells proliferate in the basal layer of epidermis. In the spinous (suprabasal) layer, cells irreversibly exit the cell cycle and switch from KRT5/KRT14 to KRT1/KRT10 production. Wnt/beta-catenin pathway is active in the proliferating epidermis, while keratinocyte differentiation in the spinous layer is under control of the Notch pathway. Deficient Notch activity alters epidermal differentiation in AD skin, expanding the proliferative compartment and influencing subsequent changes in epidermal differentiation program. Changes in extracellular Ca2+ and lipid metabolism trigger the protein kinase C (PKC) pathway activation and regulates transcription of late differentiation markers in granular layer, FLG, LOR, IVL, HBD and TGM1. Inhibition of terminal differention marker expression is observed in AD skin.
Permissions obtained from reference 28 and reference 134 to publish edited portions of images.