Abstract
Objective:
Despite good prognosis for patients with low-risk endometrial cancer, a small subset of women with low-grade/low-stage endometrial cancer experience disease recurrence and death. The aim of this study was to characterize clinical features and mutational profiles of recurrent, low-grade, non-myoinvasive, “ultra-low risk” endometrioid endometrial adenocarcinomas.
Methods:
We retrospectively identified patients with FIGO stage IA endometrioid endometrial cancers who underwent primary surgery at our institution, January 2009 to February 2017, with follow-up of 12 months. “Ultra-low risk” was defined as FIGO tumor grade 1, non-myoinvasive, lacking lymphovascular space invasion. Tumor-normal profiling using massively parallel sequencing targeting 468 genes was performed. Microsatellite instability was assessed using MSIsensor. DNA mismatch repair (MMR) protein proficiency was determined by immunohistochemistry.
Results:
A total of 486 patients with “ultra-low risk” endometrioid endometrial cancers were identified: 14 (2.9%) of 486 patients developed a recurrence. Median follow-up for non-recurrent endometrioid endometrial cancers: 33 months (range, 7–116); for recurrent endometrioid endometrial cancers: 51 months (range, 11–116). Patients with recurrent disease were older, had lower body mass index, were most commonly non-White (p=0.025, p<0.001, and p<0.001, respectively). Other clinical characteristics did not differ. MMR immunohistochemistry was obtained for 211 tumors (43%): 158 (75%) were MMR-proficient, 53 (25%) MMR-deficient. Primary tumors of 9 recurrent and 27 non-recurrent endometrioid endometrial cancers underwent mutational profiling. Most were microsatellite stable (6/9, 67% recurrent; 25/27, 93% non-recurrent). Recurrent PTEN and PIK3CA mutations were present in both groups. Exon 3 CTNNB1 hotspot mutations were found in 4/9 (44%) recurrent and 8/27 (30%) non-recurrent (p=0.44).
Conclusions:
Patients diagnosed with “ultra-low risk” endometrioid endometrial cancers have an overall excellent prognosis. However, in our study, 2.9% of patients with no identifiable clinical or pathologic risk factors developed recurrence. Further work is warranted to elucidate the mechanism for recurrence in this population.
INTRODUCTION
Endometrial cancer is the most common gynecologic malignancy in the United States, diagnosed in over 60,000 women annually 1 The majority of these women are diagnosed with low-grade, uterineconfined disease and have an excellent 5-year survival of over 90%1. However, despite this generally good prognosis, a small subset of women with low-grade/low-stage endometrial cancer experience disease recurrence and death. The recurrence rate for early stage disease across histologic subtypes varies widely, from 2 to 26% in the reported literature 2.
Previous studies have examined risk factors for recurrence among patients with stage I disease and have identified several prognostic factors, including histologic type, tumor grade, depth of myometrial invasion, presence of lymphovascular space invasion, and peritoneal cytology 3–8. The study cohorts were heterogeneous, often grouping different histologies, all stage I and occasional stage II, and patients receiving a variety of adjuvant treatments, including chemotherapy and/or radiation therapy. However, the prognostic factors predictive of disease recurrence in patients with low-grade, non-myoinvasive, lymphovascular space invasion-negative endometrioid endometrial cancers have yet to be defined.
More recently, The Cancer Genome Atlas Network identified four molecular subtypes of endometrial cancer with prognostic implications: POLE-ultramutated, MSI hypermutated, copy-number low, and copy-number high 9. This molecular classification has been proposed as a tool to help stratify risk in low-risk endometrial cancer 10. In particular, CTNNB1 exon 3 hotspot mutations have been suggested as likely drivers of a more aggressive subtype of low-grade, early stage endometrioid endometrial cancers 11. Several retrospective studies have reported that patients with uterineconfined disease whose tumors harbor a somatic CTNNB1 exon 3 mutation have worse clinical outcomes compared with patients whose tumors are CTNNB1 wild-type 12–14.
Here, we sought to evaluate the characteristics of patients with recurrent low-grade, nonmyoinvasive (“ultra-low risk”) endometrioid endometrial cancers. We explored the clinical characteristics of these patients, as well as the molecular profiles of recurrent and non-recurrent ultra-low risk tumors. The ability to accurately identify these patients early in their clinical course may lead to different decisions regarding adjuvant therapy, and an improved clinical outcome.
METHODS
Case selection
This study was approved by our institution’s Institutional Review Board. Our Institutional Database and the Gynecology Disease Management Team Database were queried for patients with International Federation of Gynecology and Obstetrics (FIGO) tumor grade 1, pathologic stage I endometrioid endometrial cancers who underwent surgery at our institution between January 2009 and February 2017. Staging was assigned using the FIGO 2009 staging system. All patients included in this study had stage IA, grade 1 endometrioid endometrial cancers without myometrial or lymphovascular space invasion. As pelvic fluid cytology is not part of the 2009 staging criteria, patients with both positive and negative cytology were included. Lymph node assessment was not required for inclusion. Patients with synchronous ovarian cancers and/or a follow-up time of less than 12 months were excluded. As surveillance visits are scheduled in 3- to 6-month increments, a minimum follow-up of 12 months captures at least two surveillance visits and improves the likelihood of identifying recurrent disease. All the endometrioid endometrial cancers included in this study were reviewed by an expert gynecologic pathologist.
Electronic medical records were queried for demographics, clinical characteristics, cancer treatment and follow-up. Time to recurrence was calculated from hysterectomy until date of pathologic proven recurrence. Overall survival was calculated from date of primary surgery until death or last follow-up.
Targeted massively parallel sequencing, microsatellite instability (MSI) and mismatch repair (MMR) deficiency analyses
DNA mismatch repair (MMR) protein status was obtained from pathology reports/electronic medical records. Immunohistochemical analysis of the MMR protein—MLH1, MSH2, PMS2, MSH6—was performed, as previously described 15. Endometrioid endometrial cancers with MLH1 and PMS2 deficiency by immunohistochemistry were subjected to MLH1 promoter methylation analysis 16. DNA from formalin-fixed paraffin-embedded (FFPE) tumors and from matched normal tissue or blood from all 9 available cases with recurrent disease and from 27 non-recurrent endometrioid endometrial cancers were subjected to MSK-IMPACT (Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets) sequencing, targeting 341–468 cancer-related genes 17,18. The primary tumor was subjected to sequencing for both recurrent and non-recurrent cases. Sequencing data analyses were performed using validated bioinformatics approaches, as previously described 19,20. All available primary tumors that developed recurrent disease were subjected to sequencing. To minimize bias in comparing genomic alterations in recurrent and non-recurrent low-risk endometrioid endometrial cancers, all non-recurrent tumors that were subjected to genomic profiling were included in analyses. For the quantification of MSI, MSIsensor was used as described by Niu et al 21. Samples with MSIsensor scores ≥10 were deemed MSI-high, MSIsensor scores ≥3 to < 10 indeterminate, and MSIsensor scores <3 microsatellite stable (MSS), as described 19,21.
Statistical analyses
Statistical analyses were performed using SPSS software, version 25.0 (IBM, Armonk, NY). Number of mutations between groups were compared using the Mann-Whitney U test, and mutational frequencies using Fisher’s exact test, two-tailed. Dichotomous outcomes were compared with χ2 test, except when the cell sizes were less than 10, in which case the Fisher’s exact test was used. Survival was calculated using the Kaplan-Meier method. Results were considered statistically significant if P<0.05 or if 95% confidence intervals (CIs) did not contain 1.0.
RESULTS
Clinical features of ultra-low risk endometrioid endometrial cancers
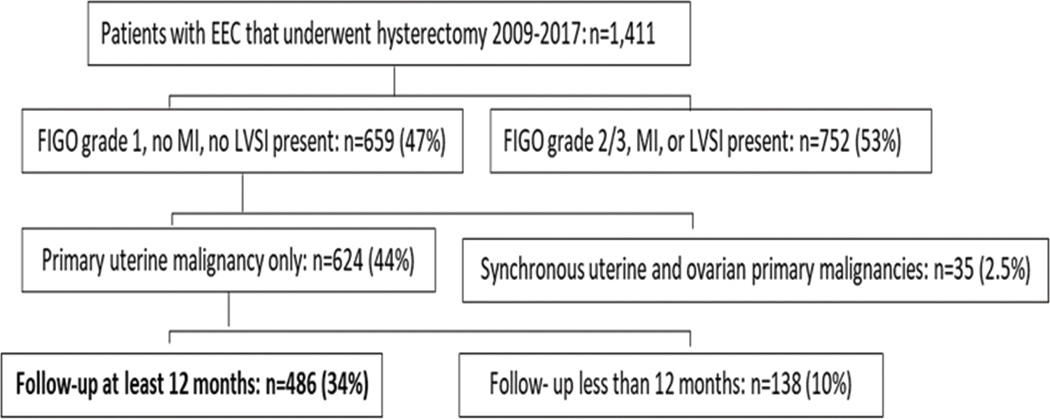
A total of 1,411 women underwent hysterectomy for pathologic stage I endometrioid endometrial cancers at our institution (Figure 1). There were 659 (47%) patients with grade 1 endometrioid endometrial cancers, no myometrial invasion or lymphovascular space invasion. Thirty-five (2.5%) of these patients were excluded because they had synchronous ovarian cancer; an additional 138 (10%) were excluded because they had less than 12 months follow-up post-surgery. In total, 486 (34%) patients were included in this study.
Figure 1.
Patient selection for inclusion into study.
Patients included had FIGO grade 1 EEC, no myometrial invasion, and no lymphovascular space invasion. Synchronous ovarian malignancy was an exclusion criterion. Pelvic/peritoneal fluid cytology positive for carcinoma was not an exclusion criterion. EEC, endometrioid endometrial adenocarcinoma; MI, myometrial invasion; LVSI, lymphovascular space invasion.
Median age at hysterectomy was 58 years (range, 28–91) (Table 1). Most patients identified as White (n=403, 83%), 17 (4%) identified as African American, 38 (8%) as Asian, 2 (0.4%) as Hispanic, 11 (2%) as Other, and 15 (3%) did not answer. Median body mass index (BMI) at time of hysterectomy was 31 kg/m2 (range, 16–69).
Table 1.
Clinico-pathologic features of the ultra-low risk endometrioid endometrial cancer patients included in this study.
| All patients (n=486) n (%) |
Non-recurrent (n=472) n (%) |
Recurrent (n=14) n (%) |
P-value | |
|---|---|---|---|---|
| Age (median, range) | 58, (28–91) | 57, 28–91 | 65, 40–84 | 0.025 |
| BMI (median) | 31 (16–69) | 31, 16–67 | 28, 21–31 | 0.001 |
| Race | ||||
| White | 403 (83) | 392 (83) | 11 (79) | 0.001 |
| African American | 17 (4) | 17 (4) | 0 (0) | |
| Hispanic | 2 (0.4) | 1 (0.2) | 1 (7) | |
| Asian | 38 (8) | 38 (8) | 0 (0) | |
| Other | 11 (2) | 11 (2) | 0 (0) | |
| Not answered | 15 (3) | 13 (3) | 2 (14) | 0.001 |
| Type surgical approach | ||||
| Open surgery | 34 (7) | 33 (7.0) | 1 (7.1) | 0.389 |
| Minimally invasive surgery | 452 (93) | 439 (93) | 13 (93) | |
| Lymph nodes | ||||
| Sentinel LN mapping | 345 (71) | 333 (71) | 12 (86) | 0.101 |
| Total LN dissection | 106 (22) | 106 (23) | 0 (0) | |
| None* | 35 (7) | 33 (7) | 2 (14) | |
| Pelvic washing status | ||||
| Positive | 21 (4) | 20 (4) | 1 (7) | 0.852 |
| Negative | 411 (85) | 420 (89) | 13 (93) | |
| Not done | 54 (11) | 32 (7) | 0 (0) | |
| DNA mismatch repair protein | ||||
| IHC | 275 (56) | 266 (56) | 9 (64) | 0.214 |
| Not performed | 158 (33) | 156 (33) | (14) | |
| Proficient | 53 (11) | 50 (11) | (22) | |
| Deficient | 23 | 20 | 3 | |
| MLH1 hypermethylation | ||||
| Lynch syndrome testing | ||||
| Testing not done | 437 (90) | 426 (90) | 11 (79) | |
| Testing done | 49 (10) | 46 (10) | 3 (21) | 0.170 |
| Testing positive for Lynch | 10 | 10 | 0 | |
BMI, Body Mass Index (kg/m2); LN, Lymph Node; IHC, immunohistochemistry
For patients who did not undergo lymph node dissection, the Mayo criteria were used intraoperatively to decide if lymphadenectomy should be performed [21].
Most patients underwent minimally invasive surgery: 107 (22%) patients had total laparoscopic hysterectomy and 345 (71%) had robotic-assisted total laparoscopic hysterectomy. An additional 34 (7%) patients underwent a total abdominal hysterectomy. Sentinel lymph node mapping and excision was performed in 345 (71%) patients, and 106 (22%) had total pelvic lymph node dissection. Thirty-five (7%) patients did not undergo lymph node analysis. In these cases, the decision to not remove lymph nodes was based on the absence of myo-invasion, as seen on intraoperative frozen section 22. Pelvic fluid cytology was obtained for 432 (89%) patients and was positive for carcinoma in 21 (4%). No patient received adjuvant therapy following surgery.
Clinical features of recurrent ultra-low risk endometrioid endometrial cancers
Of the 486 endometrioid endometrial cancers patients included in this study, 14 (2.9%) developed recurrences (Table 2). All recurrences were confirmed by an expert gynecologic pathologist. Median follow-up for ultra-low risk endometrioid endometrial cancers patients who developed recurrences (n=14) was 50.5 months (range, 20–116), compared to 34.0 months (range, 12–116) for non-recurrent cases (n=472; p=0.01). For recurring patients, median time until cancer recurrence was 13 months (95% CI, 0–31.3). Recurrent patients were older than non-recurrent patients (median 65 years, range 40–84, p=0.025; versus median 57.5 years, range 28–91) and had a lower median BMI (median 27.6 kg/m2, range 20.9–30.8; versus median 31.2 kg/m2, range 16.4–68.6, p≤0.001) (Table 1). Of note, no other clinical and pathologic characteristics assessed, including type of hysterectomy, type of lymph node dissection, the presence of positive pelvic/peritoneal cytology, or tumor DNA MMR proficiency, differed between ultra-low risk endometrioid endometrial cancers with or without recurrences.
Table 2.
Clinico-pathologic characteristics of the 14 endometrioid endometrial cancer patients with tumor recurrence.
| Recurrence characteristics | n (%) |
|---|---|
| FIGO grade at recurrence | |
| Grade 1 | 11 (79) |
| Grade 2 | 2 (14) |
| Grade 3 | 1 (7) |
| Number sites of recurrence | |
| 1 site | 11 (79) |
| >1 site | 3 (21) |
| Site of recurrence | |
| Vagina | 8 (57) |
| Lung metastases | 1 (7) |
| Pelvic mass | 2 (14) |
| Multiple sites | 3 (21) |
| Treatment of recurrence | |
| Surgery alone | 0 |
| Chemotherapy alone | 1 (7) |
| Radiation therapy alone | 6 (43) |
| Combination (surgery +/−radiation +/− chemotherapy +/− hormone therapy) | 6 (50) |
| Status at last follow up | |
| Alive with no disease | 8 (57) |
| Alive with disease | 4 (29) |
| Dead | 2 (14) |
All recurrences were of endometrioid histology, akin to the primary tumors, and the majority of recurrences were of low tumor grade: 11 (79%) grade 1, 2 (14%) grade 2, and 1 (7%) grade 3. Eleven (79%) patients had single site recurrence and 3 (21%) had multi-site recurrence. For those with single site recurrence, 8 had a vaginal cuff recurrence, 2 pelvic mass (other than lymph node), and 1 had lung nodule recurrence (Table 2). The 3 patients with endometrioid endometrial cancers with multi-site recurrence had a combination of local and distant disease (1 patient had pelvic lymph node involvement). Recurrences were treated with radiation therapy alone (n=6), chemotherapy alone (n=1), multimodal therapy (combination of chemotherapy and/or radiation therapy and/or surgery and/or hormonal therapy; n=7). Three patients had progressive or recurrent disease following completion of treatment for their first recurrence. At last follow-up, 12 (87%) patients were alive, of whom 4 (33%) had active disease. Median overall survival was not reached for the group.
DNA MMR protein analysis
Immunohistochemisty of the DNA MMR proteins MLH1, MSH2, MSH6 and PMS2 was available for 211 of 486 endometrioid endometrial cancers (43%). The majority of ultra-low risk endometrioid endometrial cancers (158/211, 75%) were found to be DNA MMR proficient, and 53 (25%) of 211 tumors displayed loss of DNA MMR protein expression. Of the 53 DNA MMR-deficient endometrioid endometrial cancers, 24 (45%) were MLH1 hypermethylated. Forty-nine of the 53 patients (92%) with MMR-deficient tumors underwent germline mutation testing, and 10 (19%) were found to have Lynch syndrome. Of the 14 patients who experienced a recurrence, MMR protein immunohistochemistry was available for 5 (36%); of these, 3 displayed loss of MMR protein expression and MLH1 hypermethylation.
Mutational profiles and MSI status of ultra-low risk endometrioid endometrial cancers
A series of 9 (n=14; 64%) recurrent and 27 (n=472; 6%) non-recurrent endometrioid endometrial cancer tumors underwent molecular profiling. There were no differences in clinicopathologic factors between patients who underwent tumor profiling and those who did not (median age, median BMI, race, type of surgical approach, type of lymph node assessment, and pelvic washing status; p>0.05, respectively). Except for patient race, clinico-pathologic characteristics did not differ between those with and without a recurrence (Table 3). First, we assessed whether there was a difference in the mutational profiles between ultra-low risk endometrioid endometrial cancers that did recur compared to those that did not. Mutational profiling of primary tumors from 9 recurrent and 27 non-recurrent endometrioid endometrial cancers patients revealed a similar mutation burden, with recurrent endometrioid endometrial cancers harboring a median of 5.9 (range, 3.7–180.6) and non-recurrent endometrioid endometrial cancers a median of 5.1 (range, 0–178.3) non-synonymous somatic mutations (p=0.52). The majority of ultra-low risk endometrioid endometrial cancers were MSS as defined by MSIsensor, and no differences between the recurrent versus non-recurrent groups were found (recurrent endometrioid endometrial cancers: 6/9 MSS, 2/9 MSI-indeterminate, 1/9 not assessable; non-recurrent endometrioid endometrial cancers: 25/27 MSI-stable, 1/27 MSI-indeterminate, 1/27 not assessable).
Table 3.
Clinico-pathologic features of the ultra-low risk endometrioid endometrial cancer patients that underwent molecular profiling (n=36).
| Non-recurrent (n=27) n (%) |
Recurrent (n=9) n (%) |
P-value | |
|---|---|---|---|
| Age (median, range) | 57 (36–75) | 62 (40–78) | 0.245 |
| BMI (median) | 32 (19–67) | 30 (26–31) | 1.000 |
| Race | 0.028 | ||
| White | 22 (81) | 6 (67) | |
| African American | 0 (0) | 0 (0) | |
| Hispanic | 0 (0) | 1 (11) | |
| Asian | 4 (15) | 0 (0) | |
| Other | 1 (4) | 0 (0) | |
| Not answered | 0 (0) | 2 (22) | |
| Type surgical approach | 1.000 | ||
| Open surgery | 1 (4) | 0 (0) | |
| Minimally invasive surgery | 26 (96) | 9 (100) | |
| Lymph nodes | 0.180 | ||
| Sentinel LN mapping | 19 (70) | 9 (100) | |
| Total LN dissection | 7 (26) | 0 (0) | |
| None* | 1 (4) | 0 (0) | |
| Pelvic washing status | 0.513 | ||
| Positive | 1 (4) | 1 (11) | |
| Negative | 24 (89) | 8 (89) | |
| Not done | 2 (7) | 0 (0) | |
BMI, Body Mass Index (kg/m2); LN, lymph node
For patients who did not undergo lymph node dissection, the Mayo Criteria were used intraoperatively to decide if lymphadenectomy should be performed. (For description of the Mayo Criteria see Mariani et al, Low-risk corpus cancer: is lymphadenectomy or radiotherapy necessary? Am J Obstet Gynecol 2000;182:1506–19.22)
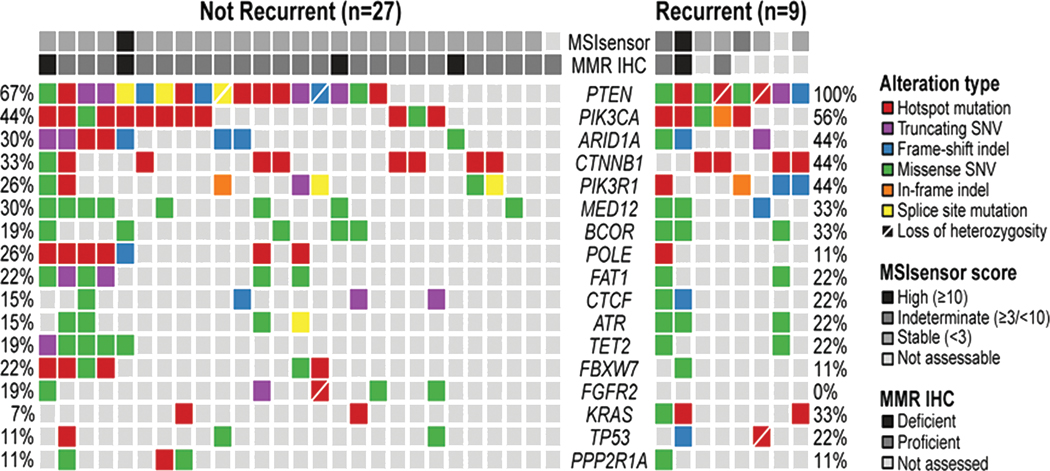
Mutational analysis revealed that PTEN and PIK3CA were the most frequently mutated genes in both groups, with PTEN mutations being present in 100% (9/9) of recurrent and 63% (17/27) of non-recurrent endometrioid endometrial cancers (p=0.04), and PIK3CA mutations in 56% (5/9) of recurrent and 44% (12/27) of non-recurrent endometrioid endometrial cancers (p=0.71) (Figure 2). Of interest, there were 6 tumors with POLE exonuclease domain mutations (EDM), including 1/9 recurrent (11%) and 5/27 non-recurrent (19%) endometrioid endometrial cancers (p=1.00). Mutations included p.A456P, p.V411L, p.P286R, p.F367V, and p.P436R, which have been previously described as hotspot or pathogenic mutations and are associated with an ultramutator phenotype 18,23–25.
Figure 2.
Mutational profiles of low grade, non-invasive endometrioid endometrial cancers with and without recurrences.
Targeted massively parallel sequencing was performed for 27 non-recurrent and 9 recurrent endometrioid endometrial cancers. All samples were from the primary tumor, regardless of recurrence status. The most recurrent genes affecting 341–468 cancer-related genes are shown. Mutation types are color coded by the legend. Note that none of the mutations were statistically significantly different between non-recurrent and recurrent ultra-low risk endometrioid endometrial cancers.
None of the other genes analyzed were mutated at statistically significant frequencies between the two groups. This included TP53, seen in 22% (2/9) recurrent and 11% (3/27) of non-recurrent tumors (p=0.58) and CTNNB1 exon 3 hotspot mutations, which were found in 44% (4/9) of recurrent endometrioid endometrial cancers and 30% (8/27) of non-recurrent endometrioid endometrial cancers (p=0.44).
DISCUSSION
While patients diagnosed with low-grade, early stage endometrioid endometrial cancer have an overall excellent prognosis, there is a subset of patients who will experience a recurrence. In our study, the rate of cancer recurrence in this selected low-risk cohort of grade 1 stage I endometrioid endometrial cancers without lymphovascular space invasion or myoinvasion was 2.9%. We did not identify any distinctive clinical characteristics that were unique to the patients who had a cancer recurrence.
Previous work has focused on the identification of molecular markers associated with recurrence in endometrioid endometrial cancers. For example, Liu and colleagues initially identified a subset of patients whose tumors harbored a CTNNB1 hotspot mutation in exon 3 and had a worse clinical outcome than those whose tumors lacked the mutation 11. This initial clinical cohort comprised patients with all grades and all stages of disease. The molecularly selected more aggressive subtype of endometrioid endometrial cancer was seen in younger patients, with low-grade (90% grade 1/2), and early stage (88% stage I/II) disease. This early finding was then validated by Kurnit and colleagues in patients with low-grade (grade 1/2) and early stage (stage I/II) endometrioid endometrial cancers, 12 in whom a CTNNB1 exon 3 mutation was associated with worse outcome. Of interest, the authors noted that patients with endometrioid endometrial cancers harboring the mutation were more likely to have tumors with pathologic characteristics associated with a lower risk of recurrence, including lower FIGO grade, less deep myometrial invasion, and less lymphovascular space invasion. The association between shorter survival and endometrioid endometrial cancer with a CTNNB1 mutation was also noted in a 2019 report by Costigan and colleagues 13.
Despite published literature demonstrating that low-grade, early stage endometrioid endometrial cancers with CTNNB1 mutation are more likely to have worse cancer-related outcomes, we identified a similar frequency of CTNNB1 exon 3 hotspot mutations between endometrioid endometrial cancers in patients with a cancer recurrence and endometrioid endometrial cancers in patients without recurrence. Importantly, we focused on evaluating an ultra-low risk cohort of patients with no myometrial invasion or lymphovascular space invasion.
While it is notable that, in our cohort, the median follow-up time for patients without a recurrence was 17 months less than for patients with a recurrence (34 versus 50.5 months), for those patients who did recur, the median time until cancer recurrence was 13 months (95% CI 0–31). Given that the majority (68–100%) of all recurrences in endometrioid endometrial cancers are diagnosed by 3 years, the median follow-up time of 33 months for the non-recurrent cohort is informative 26.
Our study is limited by its retrospective nature and the small number of tumors that were subjected to sequencing, given the rarity of ultra-low risk endometrioid endometrial cancers that recur. As a historic cohort, MMR protein proficiency data were unavailable for over half of the samples, limiting possible MMR-proficiency analysis. Further, our results are subject to a degree of ascertainment bias—all patients with non-recurrent malignancies were consented to tumor genomic sequencing at time of their diagnosis (offering testing to newly diagnosed patients has been the standard at our institution since 2016), while patients who experienced a recurrence had tumor testing either because they had a recurrence or for the purposes of this report. However, the samples included in the current study were homogeneous from a clinical and pathologic perspective: all grade 1, noninvasive tumors with no lymphovascular space invasion. Therefore, the nonrecurrent samples that had undergone genomic profiling and were included in this report were considered an appropriate representation for the non-recurrent tumors in the cohort. Finally, because of the small number of recurrent tumors that were sequenced, we could not perform any intragroup comparisons (for example, comparing the tumor genomic profile in patients that had a single site recurrence with those that had multi-site recurrences).
Although the evidence available to date supporting CTNNB1 mutation as a poor prognostic indicator is compelling, all data reported thus far are retrospective in nature. We did not identify a greater frequency of the CTNNB1 mutation in our ultra-low risk cohort. Based on our findings, tumor mutational sequencing analysis for patients with noninvasive, low-grade endometrial cancer, currently does not seem to substantially contribute to the clinical management of these patients. However, larger studies are warranted, and we anticipate the results of PORTEC-4a (CT03469674), which will help evaluate the utility of treating patients based on molecular subtyping rather than clinicopathologic staging 27. At this time, further research is warranted to identify molecular markers that distinguish the group of patients with extremely low-risk disease who experience cancer recurrence.
Supplementary Material
Highlights.
Ultra-low risk endometrioid endometrial cancer recurrence rate is 2.9%.
No identifiable clinical or pathologic risk factors were noted.
Tumor genomic profile did not reveal differences between recurrent and non-recurrent tumors.
Acknowledgments
DISCLOSURES:
Dr. Abu-Rustum reports grants from Stryker/Novadaq, grants from Olympus, grants from GRAIL, outside the submitted work.
Dr. Cadoo reports other* from Astra Zeneca, other** from Syndax Pharmaceuticals, outside the submitted work. (*Travel, accommodation, meal; institutional support for therapeutic trial; **institutional support for therapeutic trial)
Dr. Leitao is an ad hoc consultant for Intuitive Surgical Inc., outside the submitted work.
Dr. Soslow reports personal fees from Ebix/Oakstone*; personal fees from Cambridge University Press**; personal fees from Springer Publishers**; personal fees from Roche***, outside the submitted work. (*Preparation of recorded lectures; **royalties; ***one lecture)
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 2.Bendifallah S, Canlorbe G, Collinet P, et al. Just how accurate are the major risk stratification systems for early-stage endometrial cancer? Br J Cancer. 2015;112(5):793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fujimoto T, Nanjyo H, Fukuda J, et al. Endometrioid uterine cancer: histopathological risk factors of local and distant recurrence. Gynecol Oncol. 2009;112(2):342–347. [DOI] [PubMed] [Google Scholar]
- 4.Guntupalli SR, Zighelboim I, Kizer NT, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol. 2012;124(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirai M, Hirono M, Oosaki T, Hayashi Y, Yoshihara T, Matsuzaki O. Prognostic factors relating to survival in uterine endometrioid carcinoma. Int J Gynaecol Obstet. 1999;66(2):155–162. [DOI] [PubMed] [Google Scholar]
- 6.Malkasian GD Jr. Carcinoma of the endometrium: effect of stage and grade on survival. Cancer. 1978;41(3):996–1001. [DOI] [PubMed] [Google Scholar]
- 7.Tornos C, Silva EG, El-Naggar A, Burke TW. Aggressive stage I grade 1 endometrial carcinoma Cancer. 1991;70(4):790–798. [DOI] [PubMed] [Google Scholar]
- 8.Singh N, Hirschowitz L, Zaino R, et al. Pathologic Prognostic Factors in Endometrial Carcinoma (Other Than Tumor Type and Grade). Int J Gynecol Pathol. 2019;38 Suppl 1:S93–S113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cancer Genome Atlas Research N, Kandoth C, Schultz N, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talhouk A, McConechy MK, Leung S, et al. Confirmation of ProMisE: A simple, genomicsbased clinical classifier for endometrial cancer. Cancer. 2017;123(5):802–813. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Patel L, Mills GB, et al. Clinical significance of CTNNB1 mutation and Wnt pathway activation in endometrioid endometrial carcinoma. J Natl Cancer Inst. 2014;106(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurnit KC, Kim GN, Fellman BM, et al. CTNNB1 (beta-catenin) mutation identifies low grade, early stage endometrial cancer patients at increased risk of recurrence. Mod Pathol. 2017;30(7):1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Costigan DC, Dong F, Nucci MR, Howitt BE. Clinicopathologic and Immunohistochemical Correlates of CTNNB1 Mutated Endometrial Endometrioid Carcinoma. Int J Gynecol Pathol. 2019. [DOI] [PubMed] [Google Scholar]
- 14.Moroney MR, Davies KD, Wilberger AC, et al. Molecular markers in recurrent stage I, grade 1 endometrioid endometrial cancers. Gynecol Oncol. 2019;153(3):517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garg K, Leitao MM Jr., Kauff ND, et al. Selection of endometrial carcinomas for DNA mismatch repair protein immunohistochemistry using patient age and tumor morphology enhances detection of mismatch repair abnormalities. Am J Surg Pathol. 2009;33(6):925933. [DOI] [PubMed] [Google Scholar]
- 16.Walsh MD, Cummings MC, Buchanan DD, et al. Molecular, pathologic, and clinical features of early-onset endometrial cancer: identifying presumptive Lynch syndrome patients. Clin Cancer Res. 2008;14(6):1692–1700. [DOI] [PubMed] [Google Scholar]
- 17.Cheng DT, Mitchell TN, Zehir A, et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): A Hybridization Capture-Based Next-Generation Sequencing Clinical Assay for Solid Tumor Molecular Oncology. J Mol Diagn. 2015;17(3):251–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zehir A, Benayed R, Shah RH, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23(6):703–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith ES, Paula ADC, Cadoo KA, et al. Endometrial Cancers in BRCA1 or BRCA2 Germline Mutation Carriers: Assessment of Homologous Recombination DNA Repair Defects. 2019(3):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weigelt B, Bi R, Kumar R, et al. The Landscape of Somatic Genetic Alterations in Breast Cancers From ATM Germline Mutation Carriers. J Natl Cancer Inst. 2018;110(9):1030–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Middha S, Zhang L, Nafa K, et al. Reliable Pan-Cancer Microsatellite Instability Assessment by Using Targeted Next-Generation Sequencing Data. JCO Precis Oncol. 2017;2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mariani A, Webb MJ, Keeney GL, Haddock MG, Calori G, Podratz KC. Low-risk corpus cancer: is lymphadenectomy or radiotherapy necessary? Am J Obstet Gynecol. 2000;182(6):1506–1519. [DOI] [PubMed] [Google Scholar]
- 23.Church DN, Briggs SE, Palles C, et al. DNA polymerase epsilon and delta exonuclease domain mutations in endometrial cancer. Hum Mol Genet. 2013;22(14):2820–2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang MT, Bhattarai TS, Schram AM, et al. Accelerating Discovery of Functional Mutant Alleles in Cancer. Cancer Discov. 2018;8(2):174–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stasenko M, Tunnage I, Ashley CW, et al. Clinical outcomes of patients with POLE mutated endometrioid endometrial cancer. Gynecol Oncol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fung-Kee-Fung M, Dodge J, Elit L, et al. Follow-up after primary therapy for endometrial cancer: a systematic review. Gynecol Oncol. 2006;101(3):520–529. [DOI] [PubMed] [Google Scholar]
- 27.ClinicalTrials.gov. Identifier: NCT03469674, PORTEC-4a: Molecular Profile-based Versus Standard Adjuvant Radiotherapy in Endometrial Cancer (PORTEC-4a). 2019; https://clinicaltrials.gov/ct2/show/NCT03469674#moreinfo.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.