Abstract
Firearm injury is a leading cause of injury-related morbidity and mortality in the United States. We sought to systematically identify and summarize existing literature on clinical firearm injury prevention screening and interventions. We conducted a systematic search of PubMed, Web of Science, Cumulative Index of Nursing and Allied Health Literature (CINAHL), PsycInfo, and ClinicalTrials.gov for English-language original research (published 1992–2014) on clinical screening methods, patient-level firearm interventions, or patient/provider attitudes on the same. Unrelated studies were excluded through title, abstract, and full-text review, and the remaining articles underwent data abstraction and quality scoring. Of a total of 3,260 unique titles identified, 72 were included in the final review. Fifty-three articles examined clinician attitudes/practice patterns; prior training, experience, and expectations correlated with clinicians' regularity of firearm screening. Twelve articles assessed patient interventions, of which 6 were randomized controlled trials. Seven articles described patient attitudes; all were of low methodological quality. According to these articles, providers rarely screen or counsel their patients—even high-risk patients—about firearm safety. Health-care–based interventions may increase rates of safe storage of firearms for pediatric patients, suicidal patients, and other high-risk groups. Some studies show that training clinicians can increase rates of effective firearm safety screening and counseling. Patients and families are, for the most part, accepting of such screening and counseling. However, the current literature is, by and large, not high quality. Rigorous, large-scale, adequately funded studies are needed.
Keywords: firearms, injury prevention, suicide, systematic review, violence
INTRODUCTION
US firearm fatality rates remain the highest of all high-income industrialized nations despite comparable rates of both fatal self-inflicted injury and nonfatal assault-related violence (1). In 2012, firearms were responsible for more than 80,000 emergency department visits for nonfatal injuries and 30,000 fatalities (2). Significant health disparities in firearm injury persist, with youth and minority populations disproportionately affected by all types of firearm violence (2). Firearm-related injuries are currently the second leading cause of death overall among US youth aged 14–24 years and have been the leading cause of death among African-American youth for well over a decade (2). Firearms are the means of death in more than half of completed suicides (2). Nonfatal firearm injuries are associated with significant long-term consequences for both injured patients and their community, including high rates of repeat assault injury and subsequent firearm violence (3), long-term physical disabilities, and mental health complications (e.g., post-traumatic stress disorder) (4,5). The emergency department and hospital costs associated with firearm-related assaults alone are substantial, approaching $630 million annually in the United States, before factoring in the costs of lost wages and productivity, long-term medical care, and legal/criminal justice proceedings; if accounting for other forms of firearm injury, the costs would be much higher (6).
The substantial public health burden associated with firearm-related injuries has led multiple national medical organizations—including the Institute of Medicine, the American Medical Association, and many specialty societies—to urge effective programs to decrease firearm-related injuries among high-risk populations (7–14). Physician-led screening and clinically based behavioral interventions have been shown to be feasible, acceptable, and effective in other areas of injury prevention, including child safety seat use (15), intimate partner violence (16), youth violence (17), and substance use (18,19). No consensus exists, however, regarding the feasibility, acceptability, and effectiveness of health-care–based screening for risky firearm possession or regarding the effectiveness of clinically based behavioral interventions to reduce risks of firearm injury (e.g., safe storage). Such data are critical to understanding whether and how best to integrate firearm safety screening and interventions into routine clinical practice. Data on patient attitudes and perceptions around firearm screening and safety interventions are also necessary to understand the receptiveness of patients to such interventions and to address privacy concerns among policy makers.
The primary objective of this paper was to conduct a systematic review of the literature for studies examining the effectiveness—as defined by each study—of health-care–based firearm screening, counseling, or interventions for patients at risk for firearm injury. A secondary objective was to identify and examine the literature regarding clinicians' and patients' attitudes toward preventative measures to increase firearm safety and reduce all types of firearm-related injury. Results should inform future research regarding the best screening and behavioral interventions to both improve firearm safety and decrease the substantial morbidity and mortality resulting from firearm injuries among vulnerable populations.
METHODS
Search strategy
This systematic review was conducted by the study authors under the guidance of a medical research librarian at the Alpert Medical School of Brown University in April 2014. It utilized 4 databases: Cumulative Index of Nursing and Allied Health Literature (CINAHL), PsycInfo, PubMed, and Web of Science. The search was repeated in October 2014 to capture recently published articles. ClinicalTrials.gov was searched in October 2014 for ongoing firearm prevention research studies, and investigators were contacted to obtain any relevant unpublished manuscripts. Finally, the reference sections of included articles and related reviews were hand searched to identify any additional relevant studies for inclusion.
Search terms for the initial database search are detailed inSupplementary Data available athttp://aje.oxfordjournals.org/; they included Medical Subject Headings (MeSH) and non-MeSH terms related to firearms, firearm injuries, homicide, suicide, and prevention or interventions. We included only English-language articles. We included all years of publication and all ages of participants. The search strategy was purposefully inclusive of all medical specialties and was not limited to a specific study design or type of screening or intervention.
Studies were eligible for inclusion in this systematic review if they were English-language original research studies pertaining to clinician firearm screening or behavioral and educational interventions to improve patient safety (e.g., encouraging safe storage, lethal means counseling). In addition, articles examining patient or provider attitudes and beliefs on screening and/or health-care interventions were included to explore potential barriers to health-care–based screening and firearm injury prevention initiatives.
Research articles were excluded if they focused on the epidemiology of firearm injuries or if they described studies of screening and interventions in the criminal justice system, educational system, or the community, such as community-based violence intervention programs. Existing reviews, narratives, opinion articles, and overviews of clinical guidelines were also excluded. Finally, articles were excluded if they did not have a firearm-related outcome (e.g., violence intervention programs that focused on trauma recidivism in general).
Study selection
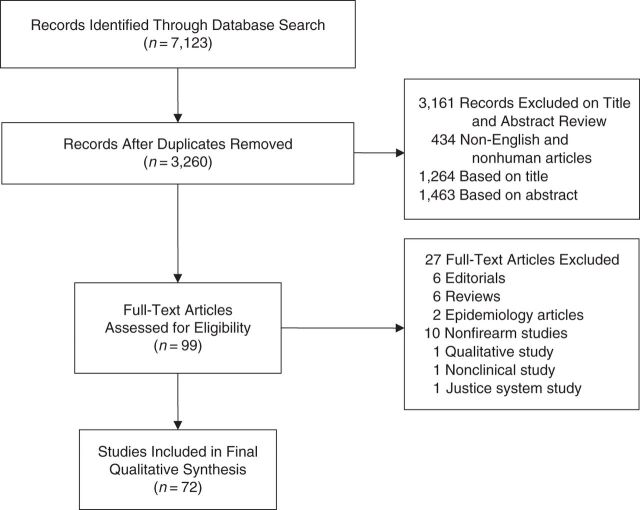
Two investigators conducted the initial title screen, eliminating duplicates across databases. The senior author repeated the title screen with a sample of 200 (7.1%) articles from the full list to assess search quality. After the title screen, abstracts were independently reviewed by 2 of 3 study investigators for inclusion within the review, with the senior author arbitrating discrepancies. In addition, 10% of abstracts underwent a random quality check by the senior author. The study investigators double-reviewed each of the remaining manuscripts for inclusion, resulting in 72 studies included in the final qualitative synthesis. Discrepancies were resolved by group consensus. The study selection and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram describing this process are outlined in Figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the study selection and screening process, 1990–2014.
Data abstraction, synthesis, and analysis
Data were abstracted utilizing a standardized form that was pilot tested and revised by all study investigators prior to the full systematic review. Each study was classified according to the study topic area: 1) clinician practice patterns and attitudes; 2) patient-level firearm safety interventions; or 3) patient attitudes regarding firearm screening and/or interventions. For papers that could potentially fit into more than 1 category, the primary hypothesis of the paper was used to choose the categorization. Additional abstracted data elements included overall study design, study population, description of the screening method or intervention (if applicable), firearm and non-firearm-related outcomes, and any significant limitations.
Methodological quality and bias analysis were also assessed for each study. We evaluated randomized controlled trials by using a modified Jadad score, which assesses the quality and risk of bias by a 5-point scale (20). As recommended by the Cochrane Collaboration (21), nonrandomized trials/studies were assessed by using a modified Newcastle-Ottawa Scale (22), a 3-instrument measure assessing quality on a 9-point scale. Methodological quality was assessed at the time of initial data abstraction. Refer toSupplementary Data for details about the scoring methods.
For both data abstraction and methodological quality for each article, 1 reviewer completed both the primary data extraction and quality assessment, and another reviewer within the study team conducted a secondary review to ensure accuracy of abstracted data and quality assessment. As described above, primary and secondary reviews and quality assessments were equally distributed among 4 reviewers. All reviews were discussed as a group, and discrepancies were resolved by group consensus. A meta-analysis of the data was deemed inappropriate because of the heterogeneity of data and the variety of study designs. Interrater reliability was not calculated as all data were discussed as a group.
RESULTS
Database search and sample characteristics
A total of 7,123 studies were identified during the initial database search in July 2014. After the removal of duplicate titles, 3,260 studies remained, of which 434 studies were excluded as they were not written in English or conducted among human subjects. Title and abstract screening excluded an additional 1,264 and 1,463 articles, respectively, that were not within the content area or scope of this systematic review. A total of 99 articles remained after the title and abstract screen for full-text review. Of these, 27 were excluded: 10 studies without an outcome measure related to firearms, 6 editorial/opinion pieces, 6 review articles, 2 epidemiologic studies, 1 qualitative study, 1 study performed in a nonclinical setting, and 1 manuscript for which the study focused on the criminal justice system.
Of the 72 reviewed articles, 53 focused on clinicians’ attitudes regarding firearm screening and/or intervention and methods of screening within clinical practice (Table 1), 12 focused on patient-level interventions to reduce firearm violence or improve firearm safety (Table 2), and 7 focused on patients' attitudes toward firearm safety counseling (Table 3). Seven articles were randomized controlled trials, 12 utilized a quasi-experimental design, 2 were prospective cohort studies, 1 was a retrospective cohort study, and 50 were cross-sectional. Thirty-two studies were focused in pediatrics, 7 in psychiatry/psychology, 5 in family practice, 4 in internal medicine, 4 in emergency medicine, 3 in pediatric emergency medicine, 2 in trauma surgery, 1 in geriatrics, 1 in preventive medicine, and 13 were multidisciplinary or in nonspecialty-specific groups of clinicians (e.g., medical students, social workers, physicians’ assistants).
Table 1.
A Summary of Studies That Examined Current Clinician Attitudes and Practice Patterns, 1990–2014
| First Author, Year (Reference No.) | Design | No. | Setting | Attitude Results | Screening Rate Results | Limitations | Jadad Scorea | Newcastle- Ottawa Scale Scoreb |
|---|---|---|---|---|---|---|---|---|
| Abraham, 2001 (70) | RCT | 56 | Pediatrics | A standardized workshop and lecture increased intervention group trainees' confidence in providing guidance about weapons access, compared with control group (P < 0.05) | After a standardized workshop and lecture, the intervention group increased screening for weapon access during a standardized patient encounter (from 52.3% to 85.7%). The control group also increased their rate of weapons screening (from 70.8% to 83.3%) | Does not focus on screening for guns. Mixed group of participants (residents + medical students). No longitudinal follow-up. Single center | 1 | |
| Barkin, 1998 (26) | Cross-sectional | 325 | Pediatrics and family practice | 80% of clinicians believed firearm safety counseling is beneficial. Among clinicians reporting ever providing counseling, 51% believed it had been effective | Only 38% of clinicians reported they had ever provided firearm safety counseling | Self-report. Single region | 5 | |
| Barkin, 1999 (27) | Cross-sectional | 325 | Pediatrics and family practice | Firearm safety counseling was ranked as theleast important injury prevention topic by 38% of respondents | 16% of clinicians reported having often or always counseled about firearm safety. Clinicians who placed lower importance on counseling were less likely to provide counseling (OR = 0.58) (P < 0.001) | Self-report. Single region | 5 | |
| Barkin, 2005 (52) | Cross-sectional | 861 | Pediatrics | 52% of pediatricians reported discussing firearms during a well-child visit. There was 85% concordance between pediatricians’ self-report of discussing firearms and families’ recall of the discussion | Self-report/recall bias. Unclear response rate. Secondary outcome | 3 | ||
| Becher, 1999 (40) | Cross-sectional | 66 | Pediatrics | 98% of pediatricians believe families with firearms should receive firearm injury prevention counseling | Although pediatricians reported screening 18% of families for firearm safety, only 11% of families reported such screening. Pediatricians were at best 65% sensitive and 32% specific in predicting which families owned firearms | Self-report/recall bias. Social desirability bias. Limited generalizability. Lack of adjustment for clustering | 3 | |
| Becher, 2000 (65) | Cross-sectional | 915 | Internal medicine and surgery | Physicians who did not own a firearm were more likely to support physician firearm injury prevention (OR = 0.4, 95% CI: 0.3, 0.53) | 19% of internists and surgeons reported screening for firearm safety. Firearm-owning physicians were more likely to report firearm screening and counseling (OR = 1.98, 95% CI: 1.34, 2.93) | Self-report/recall bias. Nonvalidated questionnaire. Low response rate. Social desirability bias | 3 | |
| Betz, 2010 (28) | Cross-sectional | 146 | Emergency medicine | 85% of psychiatrists, 65% of ED physicians, and 59% of ED nurses believe that their own staff should “always” ask suicidal patients about firearm access | Psychiatrists were more likely than ED staff to report always assessing suicidal ED patients’ firearm access (OR = 8.20, 95% CI: 1.87, 35.98). 46% of all types of providers (ED nurse, physician, and psychiatrist) said they always or often ask suicidal patients about access to firearms | Nonvalidated survey. Small sample size. Self-report. Single center | 4 | |
| Betz, 2013 (54) | Cross-sectional | 631 | Emergency medicine | 54% of ED physicians and nurses believed that, if a firearm was not accessible to a suicidal patient, the patient would find a different way to complete suicide. 86% felt it was psychiatrists’ responsibility to screen and counsel on firearm access | 49% of ED physicians and 72% of ED nurses reported “hardly ever” counseling suicidal patients about firearm access and safety | Nonvalidated survey. Self-report | 5 | |
| Borowsky, 1999 (56) | Cross-sectional | 555 | Pediatrics | Pediatricians’ likelihood of screening for guns was related to the following: prior training in violence prevention; having had a patient who was shot; and beliefs about parents’ likelihood of following advice | >50% of respondents reported rarely or never asking families about guns in their home; >70% rarely or never asked adolescents if they carry a weapon (gun, knife, others) | Low response rate. Self-reported data | 5 | |
| Butkus, 2014 (29) | Cross-sectional | 573 | Internal medicine | 74% of surveyed internists reported a need for additional training on firearm counseling. 68% of non-firearm-owning internists agreed “somewhat” or “strongly” that physicians should counsel patients about firearm safety, compared with 57% of firearm-owning internists | 80% of surveyed internists reported never assessing patients’ gun access; 77% reported never discussing firearm injury prevention with their patients | Low response ratec | 4 | |
| Cassel, 1998 (30) | Cross-sectional | 915 | Internal medicine and surgery | 84% of internists and 72% of surgeons believed that physicians should be involved with firearm injury prevention | 15% of surveyed internists and 19% of surveyed surgeons reported currently providing counseling on firearm injury prevention | Low response ratec | 6 | |
| Chaffee, 2000 (31) | Cross-sectional | 220 | Pediatrics | Pediatricians were more likely to screen if they reported the following: positive personal attitudes and beliefs about screening; greater skills and resources for screening; and the presence of positive reinforcement for screening | Pediatricians reported screening 29% of teenagers, on average, for firearm and other weapon carriage; they reported delivering an intervention for ∼50% of patients who screen positive | Nonvalidated survey. Self-reported data. Single state. | 4 | |
| Cheng, 1999 (41) | Cross-sectional | 556 | Pediatrics | 78% of surveyed pediatricians felt firearm safety was important, but only 68% felt confident in screening/counseling, and 38% felt they would be able to prevent firearm injury | 21% reported often or always addressing firearm safety during well-child visits | Self-reported data. Recall bias. Social desirability bias. Nonvalidated survey | 4 | |
| Cohen, 1998 (32) | Cross-sectional | 160 | Pediatrics | Likelihood of counseling on firearm safety by pediatric residents correlated with belief that firearm safety would be tested on the Medical Board exaination (r = 0.25,P = 0.01) | 19% of pediatric residents reported counseling all or most parents of children <1 year about firearm safety | Nonvalidated survey. Self-reported data. Single state | 3 | |
| Delnevo, 2000 (47) | Cross-sectional | 56 | Internal medicine | On review of residents’ charts for 184 new physician-patient encounters, 0% documented discussion of safe firearm storage | Small sample size. Single center. Secondary outcome | 2 | ||
| Dingeldein, 2012 (71) | Quasi-experimental | 92 | Pediatrics | An online, case-based curriculum caused a small, yet statistically significant increase in pediatric residents’ self-efficacy regarding counseling parents about firearm access with parents, compared with a control group; this effect persisted for 6 months | Single center. Social desirability bias. Not adequately powered. Nonvalidated questionnaire | 0 | ||
| Everett, 1997 (25) | Cross-sectional | 271 | Family medicine | Few respondents believed that firearm safety counseling would reduce risk of assault/homicide (14%) or suicide (20%). Although 92% agreed that patients should be counseled to keep guns locked and unloaded, 50% said firearm safety counseling should be a “low or very low priority” for family physicians | 16% of respondents reported sometimes or usually counseling their patients on firearm safety | Low response rate. Small sample size. Self-reported data | 7 | |
| Fallucco, 2012 (60) | Quasi-experimental | 104 | Pediatrics | Pediatricians who completed a skill session intervention (seminar and standardized patient clinical simulation) were more likely than the control group to report that they assessed adolescents for access to weapons (51% vs. 25%) (P = 0.007) | Low enrollment rate. Self-reported data. Single locale. Nonvalidated survey. Secondary outcome | 0 | ||
| Fargason, 1995 (66) | Cross-sectional | 175 | Pediatrics | 32% of pediatricians reported routinely counseling families about firearm safety; this rate did not differ between firearm owners and nonowners | Low response rate. Single state. Nonvalidated survey. Self-report/recall bias | 3 | ||
| Fendrich, 1998 (72) | Quasi-experimental | 321 | Emergency medicine | Clinicians reported improved knowledge but did not change their practice regarding lethal means counseling for suicidal adolescents, after an informational packet was mailed to their emergency department | Self-report. Recall bias. Unable to confirm respondents received the intervention. Social desirability bias | 1 | ||
| Finch, 2008 (58) | Cross-sectional | 486 | Pediatrics | High perceived self-efficacy and confidence in counseling on gun safety correlated with increased frequency of counseling | 24%–25% of pediatricians reported “always/almost always” discussing safe gun storage during well-child visits; 16%–17% reported “always/almost always” discussing gun removal | Low response rate. Self-reported data | 4 | |
| Frank, 2006 (64) | Cross-sectional | 2,316 | Other | The presence of a gun in the student's home inversely correlated with self-reported importance and relevance, of speaking with patients regarding firearm possession and storage | 66% of senior medical students reported that they never or rarely talk to their medical patients about firearm possession and storage | Nonvalidated survey. Self-reported data | 3 | |
| Gielen, 1997 (50) | Cross-sectional | 52 | Pediatrics | During 178 audiotaped well-child visits with 52 pediatric residents, firearm injury prevention wasnever discussed | Small sample size. Single center. Secondary outcome | 5 | ||
| Giggie, 2007 (48) | Cross-sectional | 425 | Pediatrics and psychiatry | On chart review, firearm access was documented in only 3% of pediatric emergency department psychiatric evaluations | Retrospective chart review. Single center | 4 | ||
| Goldberg, 1995 (51) | Cross-sectional | 585 | Family medicine and “primary care” | 3% of patients reported they had ever discussed firearm safety with their physician | Nonvalidated survey. Patient-reported data. Single state | 2 | ||
| Grossman, 1995 (33) | Cross-sectional | 979 | Pediatrics and family medicine | Although 97% of both pediatricians and family practitioners thought firearms should be stored locked and unloaded, the minority reported that they knew how or had time to do so | 20% of pediatricians and 8% of family practitioners reported counseling >5% of their patients’ families on firearm safety | Nonvalidated survey. Self-report. Low response rate | 4 | |
| Halpern-Felsher, 2000 (96) | Cross-sectional | 366 | Pediatrics | Pediatricians reported screening for handgun access with 30% of adolescents and counseling with 25%. Only 12% reported screening all patients, and 7% reported counseling all adolescents | Self-report: recall and social desirability bias. Low response rate. Nonvalidated survey | 3 | ||
| C. Johnson, 1999 (73) | Quasi-experimental | 308 | Pediatrics | After an interactive educational program for pediatric residents, the percentage of parents reporting firearm guidance during their well child visits increased (from 9.7% preintervention to 19.1% postintervention (OR = 2.2) (P = 0.04) | Small sample size. Recall bias by patients. Nonvalidated survey. No control group | 1 | ||
| R. Johnson, 2011 (62) | Prospective cohort | 168 | Psychiatry | Immediately posttraining, mental health providers reported high confidence and self-efficacy in discussing firearms and lethal means reductions with their clients. Slight decrease in providers’ beliefs and attitudes at 2–3 months posttraining | No pretest. No control group to compare counseling. Self-reported data. Loss to follow-up | 2 | ||
| Jones, 1992 (97) | Cross-sectional | 64 | Pediatrics | Pediatric nurse practitioners reported discussing home firearm safety with 4%–7% of families | Self-report. Social desirability bias and recall bias. Single state | 3 | ||
| Kaplan, 1998 (59) | Cross-sectional | 159 | Internal medicine and family medicine | Physicians were more likely to report asking about firearms if they had prior CME training on suicide risk assessment, geriatric health training, high confidence in diagnosing depression, a suicidal patient in the last year, or perceived patient barriers to mental health treatment | 58% of physicians reported asking depressed and suicidal elderly patients (or their families) about firearm access | Self-report. Single state | 3 | |
| Khubchandani, 2009 (43) | Cross-sectional | 28 | Other | 25% of preventive medicine residency programs provided formal training on firearm injury prevention; 89% of program directors felt firearm control was a serious public health issue. Those who provided formal training perceived significantly higher benefits | 89.3% of program directors do not routinely screen patients for firearm access, and 68% report their residents do not routinely screen patients | Self-report. Social desirability bias. Not generalizable. Small sample size | 3 | |
| Khubchandani, 2011 (57) | Cross-sectional | 64 | Psychiatry | 9.4% of psychiatric nursing student program directors provided firearm injury prevention training in the past year. Barriers to implementing training included the following: lack of faculty expertise (64.1%) and lack of existing guidelines (51.6%); number of barriers identified correlated with lower likelihood of having training programs | 48% of psychiatric nursing student program directors reported that they did not routinely screen patients for firearm ownership | Self-report. Recall bias. Social desirability bias | 3 | |
| Klein, 2001 (74) | Quasi-experimental | 161 | Pediatrics | After training in GAPS plus systemic changes to the structure of adolescent preventive care visits, more adolescents reported receiving firearm screening and counseling (from 5% to 22%) (P < 0.001); and more charts contained physician documentation of the same (from 8% to 74%) (P < 0.0001) | Generalizability of setting—clinics were preselected for likelihood of success. Self-report, social desirability bias | 1 | ||
| LoConte, 2008 (75) | Quasi-experimental | 44 | Geriatrics | Among a case-control sample of geriatric male veterans: having “access to firearms” in a standardized electronic health record note template was associated with a documented rate of firearm screening of 100%, compared with 4% in a clinic that did not use the standardized note. Among patients with firearm access, only 57% were reported to receive counseling | Small sample size. Single site, all male population. Surrogate measure of outcome. Comparison group was a separate clinic, with multiple confounders | 0 | ||
| McManus, 1997 (49) | Retrospective cohort | 54 | Pediatric emergency medicine | 0 parents of adolescent patients evaluated in the ED after an intentional drug ingestion (0 of 54) reported being informed about the risks associated with access to firearms | Recall bias. Nonvalidated questionnaire. Self-report. Small sample size. Sampling bias | 5 | ||
| Morriss, 1999 (63)d | Quasi-experimental | 33 | Multidisciplinary | 8 hours of structured, interactive training did not improve front-line, non-psychiatrically trained workers’ observed skills in removing lethal weapons from potentially suicidal patients (P = 1.00) | Small sample size. Diverse group of participants. Skills measured in role play | 0 | ||
| Olson, 1997 (34) | Cross-sectional | 982 | Pediatrics | In the 1994 version of the survey, 82% of pediatricians agreed that firearm safety counseling would reduce injury/death, 82% believed that pediatricians should screen, and 95% believed that pediatricians should counsel on safe storage | 12% of pediatricians report “always” identifying families who have firearms in their home; 33% reported “always” counseling on safe storage; 18% “always” counseled that guns should be removed from the home. Female sex, having recently treated a patient with a gun injury, and living in an urban area correlated with rates of counseling | Self-report | 4 | |
| Olson, 2007 (35) | Cross-sectional | 922 | Pediatrics | In the 2000 version of the survey, 83% of pediatricians agreed that firearm safety counseling would reduce injury/death, 87% believed that pediatricians should screen, and 96% believed that pediatricians should counsel on safe storage | 15% now report “always” screening for firearms in the home; 49% report “always” counseling on safe storage; 22% report “always” counseling that guns should be removed from the home. Older age, female sex, having treated a patient with a gun injury,not owning a gun, andnot living in a rural area now correlated with rates of counseling | Self-report | 4 | |
| Price, 1997 (67) | Cross-sectional | 300 | Family medicine | 14% of family practice residency directors perceived firearm safety counseling as effective at reducing the number of accidental firearm injuries or deaths. 16% of family practice residencies offer formal training in firearm safety counseling | Nonvalidated survey. Self report. Moderate response rate | 3 | ||
| Price, 1997 (68) | Cross-sectional | 161 | Pediatrics | 19% of pediatric residency directors perceived firearm safety counseling as effective at reducing the number of accidental firearm injuries or deaths. 34.8% of pediatric residencies offer formal training in firearm safety counseling; of these, 70% taught specific counseling skills | Nonvalidated survey. Self report. Moderate response rate | 4 | ||
| Price, 2007 (36) | Cross-sectional | 205 | Psychiatry | Psychiatrists were twice as likely to provide firearm anticipatory guidance if they held high-efficacy expectations. Psychiatrists who had some form of training on firearm counseling were >13 times more likely to counsel their patients regarding firearms | 45% of psychiatrists almost never discuss firearm issues with their patients | Nonvalidated survey. Self-report. Low response rate | 3 | |
| Price, 2010 (61) | Cross-sectional | 115 | Psychiatry | 55% of psychiatric residency program directors believed resident training could reduce firearm suicide mortality | 11% of program directors currently provide formal firearm injury prevention training for their resident; 55% of program directors routinely screen their own patients for firearm ownership/access | Self-report | 2 | |
| Price, 2013 (55) | Cross-sectional | 278 | Emergency medicine | 63% of emergency physicians thought patients wouldnot regard them as a good source of information on firearm safety. 70%–75% said their firearm counseling wouldnot impact rates of firearm homicide or suicide | 32% of emergency physicians said they did not discuss firearm issues with their patients; 48% reported discussing firearms with severely mentally ill patients | Self-report. Low response rate | 4 | |
| Shafii, 2009 (37) | Cross-sectional | 447 | Trauma surgery | 14% of trauma surgeons thought it was their personal responsibility to screen for risky behaviors including firearm access; 82% felt that trainees, nurses, or social workers should be screening; 4% thought that no one should screen | 8% of trauma surgeons reported that someone on their service currently screened for gun ownership among injured adolescent patients | Self-report. Nonvalidated survey. Low response rate. Secondary outcome | 3 | |
| Slovak, 2008 (45) | Cross-sectional | 697 | Social work | 34% of social workers reported routinely assessing patients for firearm ownership/access; 15.3% reported routinely counseling on firearm safety. Likelihood of counseling was associated with self-efficacy, knowledge, and attitudes | Low response rate. Self-report. Social desirability bias. Recall bias | 4 | ||
| Slovak, 2010 (44) | Cross-sectional | 697 | Social work | Prior training and working in an urban area increased likelihood of positive attitudes toward firearm safety assessment and counseling (P < 0.05) | Low response rate. Social desirability bias | 4 | ||
| Solomon, 2002 (46) | Cross-sectional | 322 | Pediatrics | Senior residents were more likely to report counseling teens on firearm safety (OR = 1.8, 95% CI: 1.04, 3.2) but less likely to do so if they grew up in a home with a firearm (OR = 0.67, 95% CI: 0.5, 0.91). Residents were more likely to report counseling parents if they felt it would be effective (OR = 4.8, 95% CI: 2.1, 10.9) but less likely if they were uncomfortable with doing so (OR = 0.77, 95% CI: 0.65, 0.91) | 51% and 46% reported routinely counseling teens and parents, respectively, about firearm safety | Self-report. Social desirability bias. Recall bias | 4 | |
| Thompson, 2012 (42) | Cross-sectional | 112 | Physician assistant | Although 77.7% of physician assistant program directors believed firearm violence is a problem, 15.2% reported providing firearm injury prevention training in their program (average time, 30 minutes). Lack of time, lack of expertise, and lack of standardized materials were the biggest barriers to providing training | Self-report. Social desirability bias | 4 | ||
| Traylor, 2010 (38) | Cross-sectional | 339 | Psychiatry | 58% of clinical psychologists believed that firearm safety counseling would reduce suicide attempt and completion; 79% believed firearm safety was more important among patients with mental health disorders than in the general population | 78% of clinical psychologists did not have a routine system in place to screen for firearm access among mentally ill patients; 52% provided counseling about firearm safety to high-risk patients | Self-report. Low response rate | 4 | |
| Webster, 1992 (39) | Cross-sectional | 630 | Pediatrics | 74% of pediatricians agreed/strongly agreed that pediatricians have a responsibility to counsel families about firearms | 30% of pediatricians reported ever counseling patients on firearm injury prevention | Nonvalidated survey. Self-report. Single state | 4 | |
| Wright, 1997 (53) | Cross-sectional | 135 | Pediatrics | Residents were more likely to report firearm screening/counseling if they had training on firearm injury prevention (OR = 10, 95% CI: 4.15, 24.58) and if they were familiar with AAP's TIPP or STOP program (OR = 3.03, 95% CI: 1.17, 7.99). Barriers to counseling included the following: lack of information (59.1%), not enough time (27.3%), and belief that parents were not receptive to counseling (13.6%) | 50.7% of pediatric chief residents reported routinely providing age-appropriate firearm injury prevention counseling | Self-report. Social desirability bias. Fidelity of counseling not determined. Not generalizable—chief residents may not be surrogate for all pediatric residents | 2 | |
| Zavoski, 1996 (69) | Cross-sectional | 140 | Pediatrics | 56% of pediatric residency program directors reported teaching residents about firearm safety | Nonvalidated survey. Low response rate. Self-report | 4 |
Abbreviations: AAP, American Academy of Pediatrics; CI, confidence interval; CME, continuing medical education; ED, emergency department; GAPS, Guidelines for Adolescent Preventive Services; OR, odds ratio; RCT, randomized controlled trial; STOP, Steps to Prevent Firearm Injury; TIPP, The Injury Prevention Program.
a Jadad Score (for randomized controlled trials) out of a total of 5 points.
b Modified Newcastle-Ottawa Score (for other study designs) out of a total of 9 points.
c Used essentially the same survey tool.
d Study performed in the United Kingdom.
Table 2.
Studies That Evaluated Patient-Level Interventions to Alter Risky Behaviors Such as Weapon Carrying or Methods of Firearm Storage, 1990–2014
| First Author, Year (Reference No.) | Design | Target | No. | Setting | Results | Limitations | Jadad Scorea | Newcastle- Ottawa Scale Scoreb |
|---|---|---|---|---|---|---|---|---|
| Albright, 2003 (84) | Quasi-experimental | Adults | 156 | Family medicine | Patients who received brief verbal/written counseling were 3 times more likely to make safe changes in gun storage habits (OR = 3.04, 95% CI: 1.28, 7.24) | Not randomized. Small sample size. Self-reported outcomes using nonvalidated questionnaire | 1 | |
| Barkin, 2008 (23) | RCT | Parents | 124 practices, 4,890 parents | Pediatrics | A motivational interviewing-based pediatric intervention increased parents’ prevalence of firearm storage with cable locks at 6 months postvisit (P = 0.001) | Self-reported outcomes | 4 | |
| Brent, 2000 (81) | Quasi-experimental | Parents | 106 | Psychiatry | A physician recommendation to remove firearms from the home to families of depressed teens resulted in 27% of families removing firearms from the home at the close of the clinical trial and 36% at 2 years | Secondary, post hoc analysis. Small sample size. Not generalizable. Intervention not standardized. Self-report of firearm ownership. Social desirability bias | 0 | |
| Carbone, 2005 (85) | Quasi-experimental | Parents | 180 | Pediatrics | Families who were given brief counseling, a brochure, and a firearm lock had improved firearm-safety practices compared with control group (61.6% vs. 26.9%) (RR = 2.29, 95% CI: 1.52, 3.44) (P < 0.001) | Time-series design. Small sample size. Self-report. Social desirability bias | 1 | |
| Grossman, 2000 (79) | RCT | Parents | 56 practitioners, 1,295 families | Pediatrics | After practitioner-delivered firearm safety (“STOP”) counseling, no difference between intervention and control groups in rates of firearm acquisition (1.3% vs. 0.9%)(P = 0.44), rates of firearm removal (6.7% vs. 5.7%) (P = 0.98), or rates of purchase of firearm safety equipment among firearm owners (27.3% vs. 21.0%) (P = 0.24) | Difficulty assessing whether intervention was delivered. Self-reported outcomes using nonvalidated questionnaire | 1 | |
| Johnston, 2002 (78) | RCT | Adolescents | 631 | Pediatric emergency medicine | At 3 and 6 months post-ED visits, teens who received a brief intervention from a trained therapist were no more likely to report decreased weapon carriage than the control group; this held true even among those reporting weapon carriage at baseline (RR = 0.67, 95% CI: 0.16, 2.71) | Intervention targeted multiple injury prevention behaviors. Low rate of risky behavior at baseline. Secondary outcome. Self-reported data | 3 | |
| Kruesi, 1999 (80) | Quasi-experimental | Parents | 103 | Pediatric emergency medicine | Receiving means restriction counseling from ED staff increased parents’ likelihood of locking up or disposing of firearms after a child's mental health assessment in the ED (5 of 8 receiving counseling vs. 0 of 7 not receiving counseling) | No randomization. Potential for confounders in group not receiving intervention. Self-reported data. Small sample size | 1 | |
| Morriss, 1999 (63) | Quasi-experimental | Clinicians | 33 | Other | No improvement in ability to remove lethal weapons from potentially suicidal patients (P = 1) | Program evaluated in nonphysician staff | 1 | 1 |
| Oatis, 1999 (83) | Quasi-experimental | Parents | 1,617 | Pediatrics | After practice-wide implementation of clinician (“STOP”) counseling about firearm safety, parents reported no change in prevalence of guns in the home (P = 0.1), guns being stored unlocked (P = 1.0), or guns being stored loaded (P = 0.3) | Self-reported data. Low follow-up rate. Underpowered | 1 | |
| Sangvai, 2007 (76) | RCT | Parents | 319 | Pediatrics | After a multicomponent intervention, no difference in observed firearm safe storage was observed between intervention and control groups | Intervention targeted multiple injury prevention behaviors. Extremely low enrollment and follow-up rates | 2 | |
| Sherman, 2001 (82) | Prospective cohort | Adults | 46 | Psychiatry | Of patients threatening to harm themselves or others with a firearm, none had access to a firearm at discharge. Of the 30% with access to a firearm at admission, all relinquished their firearm prior to discharge; 11% of the total sample was readmitted with access to a firearm within 24 months | No comparison group. Small sample size | 4 | |
| Stevens, 2002 (77) | RCT | Adolescents | 3,145 | Pediatrics | Among recipients of a multicomponent office-based injury prevention counseling intervention, safe firearm storage did not increase at any time point | Intervention targeted multiple injury prevention behaviors. Self-reported outcomes. Low baseline rate of gun ownership | 1 | |
| Zatzick, 2014 (24) | RCT | Adolescents | 120 | Trauma surgery | Reduction in risk of continuing to carry a weapon at 1 year of follow-up after a stepped collaborative care intervention for hospitalized, assault-injured adolescents (RR = 0.31, 95% CI: 0.11, 0.90) | Weapon carriage not a primary outcome. Outcome not specific to firearms, but inclusive of them | 5 |
Abbreviations: CI, confidence interval; ED, emergency department; OR, odds ratio; RCT, randomized controlled trial; RR, relative risk; STOP, Steps to Prevent Firearm Injury.
a Jadad Score (for randomized controlled trials) out of a total of 5 points.
b Modified Newcastle-Ottawa Score (for other study designs) out of a total of 9 points.
Table 3.
Studies That Examined Patient Attitudes Toward Firearm Safety Counseling, 1990–2014
| First Author, Year (Reference No.) | Design | Target | Number | Setting | Results | Limitations | Newcastle- Ottawa Scale Scorea |
|---|---|---|---|---|---|---|---|
| Bonds, 2007 (87) | Cross-sectional | Adult patients | 3,175 | Internal medicine | 53% of patients felt providers should never ask about the presence of guns in the home; 7% reported being screened in the previous year. Patients who had been asked about firearms by their PCP within the past year were more likely to endorse future screening (OR = 4.4, 95% CI: 3.4, 5.8) | Low response rate. Self-report. Nonvalidated survey. Female-only study. Single state | 4 |
| Forbis, 2007 (86) | Cross-sectional | Parents | 951 | Pediatrics | 8% of parents reported receiving firearm counseling during an office visit. Non-firearm owners, compared with firearm owners, were more likely to say physicians should screen for firearm possession (72% vs. 59%) (P < 0.001) or should advise families to remove firearms from the home (42% vs. 12%) (P < 0.001) | Self-report. Recall bias. Nonvalidated survey. Social desirability bias | 5 |
| Haught, 1995 (89) | Cross-sectional | Parents | 510 | Pediatrics | 11% of caregivers reported prior firearm safety screening/counseling; 74% thought pamphlets or posters in the clinic on firearm safety would be helpful. Although only 17% thought speaking with a physician or nurse would be useful, 84% said they would either follow a physician's advice or “think it over” | Self-report. Single region. Nonvalidated survey | 4 |
| May, 1993 (91) | Cross-sectional | Adult patients | 53 | Internal medicine | 81% of young African-American men, interviewed after a clinic visit with a single provider in which they discussed firearm safety, reported that discussing firearms with their physician was important | Nonvalidated survey. A single clinic with a single physician. Small sample size. Unclear response rate | 1 |
| Radant, 2003 (92) | Cross-sectional | Adult patients | 964 | Family medicine | 76% of firearm owners did not want to learn about firearm safety information from their physician | Self-report. Single state. Nonvalidated survey | 3 |
| Shaughnessy, 1999 (88) | Cross-sectional | Adult patients | 1,214 | Family medicine | 8% reported having previously been asked about gun safety by their physician; 20% would be offended if their physician asked; 57% of patients felt gun safety should not be discussed as it was a lower priority compared with other medical issues, and only 14% thought their physician was knowledgeable on the topic | Single state. Nonvalidated (but previously used) adaptation of others’ surveys | 3 |
| Webster, 1992 (90) | Cross-sectional | Parents | 215 | Pediatrics | 90% of all parents were willing to discuss firearms with their pediatrician. Willingness to follow a pediatrician's advice on firearm safety was lower for gun-owning families and for fathers | A single state. Nonvalidated survey | 3 |
Abbreviations: CI, confidence interval; OR, odds ratio; PCP, primary care provider.
a Modified Newcastle-Ottawa Score (for other study designs) out of a total of 9 points.
Generally, study quality was graded as low across all study designs. Only 2 randomized controlled trials scored at a 4 or 5 on the 5-point Jadad scale (23,24), and only 1 nonrandomized controlled trial scored as a 7 or higher on the modified Newport-Ottawa Scale (25). Most of the studies used nonvalidated outcomes that were subject to both recall and social desirability bias (e.g., providers reporting their own screening rates; patients reporting their own rates of safe firearm storage). The vast majority of studies utilized proxy measures for firearm injury risk, that is, safe storage, firearm carriage, and access to firearms by high-risk groups. No studies utilized firearm injury as an outcome measure.
Clinician practice patterns and attitudes regarding screening and firearm safety interventions
Of the 53 studies (Table 1) that focused on clinician practice patterns and attitudes, the majority (43 of 53) were cross-sectional in nature with 37 of the studies reporting on clinicians' practice patterns regarding firearm screening and counseling. Current self-reported screening and counseling rates by clinicians were low in all studies and across all surveyed disciplines (nurses, clinical psychologists, social workers, medical students, residents, attending physicians, family medicine, pediatrics, psychiatry, surgery, emergency medicine, and preventive medicine). Multiple studies reported a large disparity between the percentage of clinicians believing that firearm screening and interventions were important and the percentage of clinicians who reported actually using evidence-based screening or intervention practices (25–46).
Everett et al. (25), authors of the only manuscript in this group to receive a modified Newport-Ottawa Scale of 7 or greater, described family practitioners' experience in firearm safety counseling; this study found that only 16% of family practitioners sometimes or usually counsel patients regarding firearm safety, with over three fourths reporting they lacked formal training, only one fifth believing counseling would reduce the risk of firearm-related suicide, and even fewer believing counseling would reduce the risk of firearm-related assault or homicide.
Six studies examined a measure other than simply clinician-reported behaviors. Direct observational studies found that firearm access or injury prevention was discussed or documented in 0% of new patient visits in internal medicine (47), 0%–3% of pediatric emergency department psychiatric evaluations (48,49), and 0% of well-child visits in an urban pediatric clinic (50). In a survey of adult primary care patients, only 3% reported having ever discussed firearm safety with their primary care provider (51). Barkin et al. (52) found high concordance between physician- and patient-reported rates of discussing “guns around children.” Becher and Christakis (40) found poor sensitivity and specificity of pediatricians' estimation of whether a family owned a firearm, compared with families' own self-report of firearm ownership.
Clinicians who lacked formal training (25,36,45,46,53), who felt that suicide was not preventable (25,54,55), or who felt that patients were unlikely to follow their advice (43,56,57) were unlikely to screen and counsel on firearm safety among any population. Clinicians who felt suicide was preventable, who believed that screening and counseling made a difference in injury prevention, who had prior training, and who had high self-efficacy reported higher screening and counseling rates (26,27,31,32,36,44,46,53,56,58,59). Most studies in this group assessed the frequency of queryingparents regarding the presence of a firearm in the home and recommending safe storage (i.e., locked and unloaded) or firearm removal (25–27,32–35,39,46,50,52,55,56,58). The second most common group of studies examined screening and lethal means counseling in depressed or suicidal patients (28,36,38,48,54,59–63).
Three studies (34,35,64) reported an inverse correlation between the clinician's reporting being a firearm owner and rates of providing anticipatory guidance on firearm safety. In 1 study, however, being a firearm owner increased the rate of screening and counseling (65); in another study, there was no difference in the reported rate of firearm safety counseling between firearm owners and nonowners (66).
Emergency physicians believed that firearms were a larger problem among those with mental illness than among the general population, and both emergency physicians and trauma surgeons felt that it was the responsibility of a psychiatrist or other specialist to conduct firearm screening and subsequent anticipatory guidance to improve firearm safety practices (28,37). Several studies, however, reported that psychiatrists and psychologists screen the minority of their at-risk patients (28,36,38,48). Most clinicians reported selective screening for those patients whom they felt to be most at risk of firearm injury, rather than universal screening of patients within their practice (31,37,38).
The minority of pediatric, psychiatric, and family medicine residencies reported providing firearm injury prevention training to their residents (61,67–69). Program directors for preventive medicine, psychiatric nursing, and physician assistant training programs also reported infrequently offering firearm safety training to their students (42,43,57).
Nine studies examined the efficacy of clinician-level interventions to change rates of firearm safety screening and counseling. Eight tested whether an interactive seminar or educational session changed firearm screening and intervention practices for at-risk adolescents (60,70–72), pediatric well-child visits (73,74), or depressed or suicidal patients (62,63). One study tested whether standardizing the assessment of access to weapons in patients with dementia changed screening and counseling rates (75). The sole randomized controlled trial by Abraham et al. (70) compared a multihour lecture and workshop with standard violence prevention education for pediatric residents and medical students. In this study, both intervention and control group participants significantly increased their rate of screening for weapon access (among other items) during standardized patient encounters from pre- to posttest; however, the intervention group reported higher self-efficacy and confidence in weapon screening compared with the control group. In 2 quasi-experimental studies of interactive educational programs for pediatricians (skill sessions, role playing, lectures), physicians’ attitudes and self-reported firearm screening rates improved (60,73). A similar lecture and multihour workshop for community mental health providers and for volunteer front-line non-mental health workers resulted in high posttraining confidence and self-efficacy regarding firearms and lethal means discussions (62). In another study of a similar intervention among front-line non-mental-health workers (e.g., in primary care offices, emergency departments), there was no observed change in the workers' ability to remove lethal means from suicidal patients postintervention (63). A quasi-experimental study showed that a case-based, online firearm injury prevention curriculum for pediatric residents resulted in an increase in beliefs that pediatric residents should discuss firearm safety with parents; this change persisted 6 months after the intervention (71). A pre- and poststudy that examined the effect of the American Medical Association's “Guidelines for Adolescent Preventive Services” in several community and migrant health centers found that, after implementation, screening for firearms significantly increased according to both adolescents' report and chart review (74). A quasi-experimental study of emergency medicine physicians showed that, compared with no information, mailed information packets may increase the rate at which emergency physicians self-report recommending firearm removal from suicidal adolescents (72). In a single case-control study of the geriatric population, patients in a clinic that had “access to firearms” as a field in the electronic health record note template had 100% documented screening versus 4% at a similar clinic without an electronic health record prompt (75).
Studies in this group were limited by recall bias, use of nonvalidated self-report measures, lack of objective data, small sample sizes, and an inability to compare respondents with nonrespondents. Many were also limited by nonresponse bias. Studies that aimed to effect change in providers' beliefs in or rates of screening/counseling were limited by quasi-experimental designs that were unable to control for confounders.
Patient-level interventions to improve firearm safety
Twelve studies (Table 2) focused on patient-level interventions to reduce firearm-related injury risk or increase firearm safety measures. The 2 studies with the highest quality scores (i.e., randomized controlled trials with a Jadad scale ≥4) were found to be effective at improving firearm safety. Barkin et al. (23) conducted a cluster-randomized trial in which pediatric practices were randomly assigned to training in a 5-part motivational interviewing-based violence prevention screening and brief intervention versus usual practice; the intervention strategy included information about safe firearm storage. At 6-month follow-up, parents in the intervention practices reported increased usage of firearm cable locks (odds ratio =2.0, 95% confidence interval: not reported) (P = 0.001). Zatzick et al. (24) found that, among a sample of adolescents admitted to a hospital trauma unit, a collaborative care intervention (combining elements of motivational interviewing, case management, and stepped pharmacological treatment for post-traumatic stress disorder) was more effective than standard care at reducing risky behaviors, including weapon carriage (relative risk = 0.31, 95% confidence interval: 0.11, 0.90).
Two moderate quality randomized controlled trials and 2 low quality randomized controlled trials found that less theoretically based or firearm-focused counseling strategies were ineffective at increasing safe firearm storage (76,77) or decreasing weapon carriage rates (78,79) in high-risk populations. Two of these trials (76,77) studied pediatric office-based multicomponent interventions (including nonspecific counseling methods, provision of safety equipment, and booster calls) on multiple injury prevention topics. In Sangvai et al. (76), research staff delivered the intervention to parents; in Stevens et al. (77), office staff delivered it to parents. Neither study observed an increase in parental reports of safe firearm storage among intervention recipients compared with the control group. Both studies had significant limitations. Sangvai et al. reported a low enrollment rate of 35%, enrollment bias with nonparticipants more likely to be firearm owners (P < 0.001), and low follow-up rates of 8%. In Stevens et al., a minority of eligible participants received the intervention (47%). In the study by Grossman et al. (79), pediatric practitioners delivered a structured American Association of Pediatrics-endorsed brief on firearm safety to parents, complemented by coupons for safety equipment. This intervention, too, found no increase in parental safety behaviors. Limitations included high rates of loss to follow-up (77% retention) and difficulty assessing intervention delivery (73% documented as receiving the intervention). Furthermore, the study was underpowered to detect the desired change in firearm safety behaviors given the low rate of firearm ownership. In Johnston et al. (78), injured teens being treated in the emergency department were randomly assigned to standard care or to trained therapists delivering a motivational interviewing-informed counseling session. Although this intervention was theoretically based, it covered multiple injury prevention topics, including helmet use, seatbelt use, and firearm safety. This study found no change in weapon carriage at 6 months (relative risk = 1.0, 95% confidence interval: 0.54, 1.88). It was limited by a small number of adolescents (n = 30) who carried a weapon at baseline and by the lack of clarity regarding which intervention topics were covered.
The remaining intervention studies used a mix of quasi-experimental and retrospective or prospective cohort designs. These studies examined a variety of techniques, including means restriction counseling (80,81), multidisciplinary treatment teams (82), and multicomponent interventions similar to those of the study by Grossman et al. (79,83–85). Positive effects were observed on firearm access among suicidal teens in the emergency department (80), firearm access among admitted suicidal adults (82), and safe firearm storage among family medicine patients (84). There were also improvements noted in safe storage practices in families at a pediatric clinic (85). Firearm-owning parents of adolescents with major depression infrequently complied with physician recommendations to remove firearms from the home (27%) (81). No change in safe storage rates of firearms was observed among parents of pediatric patients who presented to a primary care practice that had implemented the American Academy of Pediatrics' Steps to Prevent Firearm Injury program (83).
Patient attitudes regarding firearm screening and safety interventions
Seven studies described patient attitudes toward clinicians' firearm screening and behavioral counseling (Table 3). All studies were cross-sectional in nature, and all were of low methodological quality. A minority of adult primary care patients had previously discussed firearm injury prevention with their physician (86), and those who had not been screened were unlikely to want to do so in the future (87,88). Parents of pediatric patients (including those queried in an article which primarily addressed clinician screening practices) (40,89,90) and high-risk urban African-American young men (91) expressed interest in discussing firearm safety. Most patient groups reported, however, that discussing firearm safety with their physician was a lower priority when compared with other preventive health topics, and few saw their physician as an authoritative source of information about firearm safety (88–90). Firearm owners reported they would be less likely to follow the advice of physicians regarding safe storage practices (89,90,92), were less likely to agree that physicians should screen for firearm possession (86), and were less agreeable to remove firearms from the home (40). Study results were limited by small sample sizes, low response rates, and recall bias.
DISCUSSION
Our systematic review is most notable for a lack of rigorous evidence regarding clinically based firearm safety screening practices or interventions for high-risk populations. Although existing studies suggest improvement in screening rates and firearm safety from clinically based screening and interventions without showing evidence of harm, further investigation is clearly needed. The studies in this review were generally of lower quality, as assessed by standardized scoring instruments, and had significant limitations restricting our ability to define best practice. This finding is likely reflective of the lack of research funding for such studies over the past decade (14,93–95), as rigorous studies require a substantial financial investment of resources. The results of this review therefore emphasize the need for design of, and funding for, high-quality research on clinically based firearm safety screening and on interventions to reduce firearm injury rates among high-risk populations.
Current practice
The studies examining screening practices and physician attitudes demonstrate that, despite clinician acceptance of the need for firearm injury prevention among high-risk populations (30), screening and counseling to increase safety are performed by a minority of clinicians in primary care, psychiatry, psychology, pediatrics, emergency medicine, and trauma surgery (25–27,29–35,37,39–41,43,45,47,48,50,51,54,56,58,64,66,96,97). Although many of these studies had methodological limitations, one would expect social desirability bias and low response rates to increase, not decrease, the reported rates of screening. On the basis of the literature from other areas of preventive medicine (98–102), we hypothesize that the lack of screening and intervention guidelines, as well as the absence of clinician education about why and how to reduce high-risk patients' firearm injury rates, explains the disparity between attitudes and practice.
Our systematic review shows that clinician beliefs and self-efficacy influenced how frequently they screened for firearm access or provide injury prevention counseling, highlighting the need for additional training to improve such practices (25,34–36,43,54,56,64). Clinicians who lacked formal training, who felt that suicide was not preventable, and who believed that patients were unlikely to follow their advice were unlikely to screen and counsel on firearm safety; clinicians who had high confidence and self-efficacy toward counseling were more likely to screen (25,26,31,36,54–56,58,59). Although many of the studies on physician screening practices were published in the 1990s, it is unlikely that clinician awareness, training, and practice regarding firearm injury prevention have changed significantly in the interim.
Nine studies included in our systematic review specifically addressed how best to increase clinician screening (60,62,63,70–75). All of these studies, although advancing the dearth of knowledge in the field, were limited methodologically and had varying degrees of reported efficacy. They all emphasize the need for a heightened focus on improving clinician training, particularly in the primary care, psychiatric, and emergency department settings, on firearm safety counseling, recognition of persons at risk, and understanding how to implement effective injury prevention practices.
Others' work confirms that increased exposure to suicide prevention interventions in general might enhance clinician awareness and acceptance of screening (103). Clinician educational interventions regarding clinical approaches to high-risk alcohol and other drug use, youth violence, and other similar injury risk factors have been shown to be effective (101,104,105). Similar programs may be successful for increasing firearm safety screening and counseling, as well.
Who should be screened?
The available literature is notably silent regarding who should be screened for firearms and in what health-care setting such screening should occur. Many of the pediatric studies in this review posit that firearm screening should be a standard part of universal injury prevention screening, alongside screening for seat belts, smoke detectors, and bicycle helmets (27,32,76–78). Such studies, however, generally found low existing rates of such universal, primary care-based screening (27,32) and often reported low increases in screening rates with multitopic screening and interventions (63,73,74,76).
Epidemiologic studies, not eligible for this systematic review, highlight the need for indicated screening among high-risk clinical populations. Approximately 40% of suicidal youth have access to a firearm (106). Adolescent firearm unintentional or suicidal deaths are strongly associated with unsafe firearm storage at home (107). Almost one fourth of assault-injured youth seeking emergency department care in an urban setting have a firearm (108), with ∼60% of these youth going on to experience a subsequent firearm violence event within the next 2 years (3). These papers, in combination with other studies in our review (24,80), suggest that indicated screening among high-risk populations or during a high-risk clinical event may be a useful method for identifying patients at risk of firearm injury.
Surprisingly, none of the studies in this systematic review examined the yield or accuracy of indicated firearm safetyscreening among known high-risk populations (although, as discussed below, multiple studies examined counseling in these groups). None of the studies compared the rate of identification of high-risk patients using indicated versus universal screening, and none of the studies examined whether screening should be limited to health-care settings where patients are either most comfortable discussing potential high-risk behaviors (e.g., primary care offices, psychiatrist office) or most at risk for negative outcomes related to high-risk firearm behaviors (e.g., during an emergency department visit for suicidal ideation). The lack of high-quality studies examining such best practices for firearm safety screening limits the ability to derive consensus guidelines for clinicians and again highlights the need for additional well-funded research (109).
Possible interventions
The literature reviewed is also far from conclusive regarding best practices for intervening with patients who screen positive for high-risk firearm behaviors (e.g., suicidality in a patient with an unlocked firearm or an underage youth with a history of recent violence). This review did identify evidence that clinically based interventions could affect high-risk firearm behaviors, including improving rates of safe storage and reducing firearm access among assault-injured youth, parents of young children, and depressed or suicidal patients (23,24,80–82,84,85). Three studies in our review suggest that counseling of suicidal patients or their parents about lethal means restriction may increase rates of firearm removal from the home (80–82). Studies that used structured, theoretically based interventions (e.g., motivational interviewing or stepped collaborative care) were identified in our review as most effective at achieving improved firearm safety (23,24). Dissemination studies and those that intervened on multiple injury prevention topics in low-risk patients were markedly less effective, perhaps highlighting the difficulty of addressing multiple risk behaviors, especially among patients with low rates of risky firearm ownership (76–78,83). These results suggest that how counseling is delivered, to whom, and in what setting, are all critically important aspects of firearm safety initiatives. Presumably, different types of interventions should be targeted to different populations. For instance, the content of counseling would differ for suicidal patients, older depressed adults, parents of toddlers, and youth carrying a firearm for protection. More study is needed, however, to determine the best theoretically based interventions for improving firearm safety for each high-risk group. Research is also needed to test which type of clinician can most effectively provide an intervention (e.g., physician, psychiatrist, social worker).
Previous clinical intervention studies regarding substance abuse, violence, and other risky behaviors may help inform development of clinical firearm safety interventions. Motivational interviewing has been shown to be an effective strategy for reducing peer and dating violence in alcohol-using youth presenting to the emergency department (110,111). Structured violence intervention programs may decrease future violence among assault-injured patients (8). Restricting access to readily available lethal means (e.g., firearms, bridges, domestic gas, and so on) through legislation or engineering has been associated with reductions in suicide completion by those means (112–122); however, the efficacy of lethal means counseling by clinicians needs to be further studied (123). The use of technology to deliver such interventions may also help to improve reach and efficacy (124–126).
Regarding patient receptiveness toward discussing firearms and firearm safety with physicians, our review suggests that patients would accept physician counseling (87,89–91), but more research is needed to understand which patients, if any, perceive firearm safety to be a low priority (88). Better injury prevention skills by providers can improve patient education on the importance of discussing firearm safety at the individual level. Public health campaigns such as the Asking Saves Kids campaign (127) and the Children's Safety Network (128) may educate patients and clinicians about the importance of this topic at the community level. Continued and intensified public outreach may assist in raising the profile on the issue of firearm injury and might make it more likely that parents and patients will be more receptive to receiving information and counseling from providers in the office or hospital setting.
Limitations
There are a number of limitations to our systematic review. Most significantly, only 72 relevant studies met our inclusion criteria, and most were of low quality as determined by the scoring systems outlined in our methods and our supplemental tables (Supplementary Data). Further, many studies have small sample sizes, and there is significant heterogeneity between the included studies. For these reasons, it is difficult to draw concrete conclusions regarding best screening and intervention practices from our results. Although search methodology conformed to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for identifying studies in a systematic review (129), some relevant publications may have been inadvertently missed. We attempted to address this through a repeat review of our search results as well as by reviewing the references of included studies for potentially missed articles. Finally, although standardized, validated scoring criteria were used to assess study quality, and although multiple reviewers were used to minimize error or bias, data extraction and scoring methods are inherently subjective, possibly resulting in incorrect study categorization.
Conclusion
In conclusion, our systematic review of the current medical literature identified 72 publications that reported on patient-level interventions to improve firearm injury prevention screening and intervention, that described current clinician attitudes and practice patterns regarding firearm safety screening, or that described patient attitudes toward firearm safety counseling. This review shows that screening rates, even among high-risk populations, are currently low, which appears to be largely due to low provider self-efficacy and lack of training across all disciplines. Some higher quality studies demonstrated that interventions might be effective at improving rates of safe firearm storage in homes with children and at reducing firearm carriage among traumatically injured youth. No studies showed harm, and some suggest there may be a benefit in interventions for suicidal patients. Further research is needed to identify how high-risk patient behaviors should be identified and what types of interventions most effectively reduce injury risk. Our success in other injury prevention topics, such as reducing motor vehicle crashes (94), suggests that we can succeed in reducing injury with adequate research and resources. We are clearly at the beginning of delineating best practices for clinically based firearm injury prevention.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts (Paul J. D. Roszko); Department of Emergency Medicine, Rhode Island Hospital/Alpert Medical School of Brown University, Providence, Rhode Island (Megan L. Ranney, Jonathan Ameli); School of Public Health, University of Michigan, Ann Arbor, Michigan (Patrick M. Carter, Rebecca M. Cunningham); Department of Emergency Medicine, University of Michigan, Ann Arbor, Michigan (Patrick M. Carter, Rebecca M. Cunningham); and Injury Prevention Center of Rhode Island Hospital, Alpert Medical School of Brown University, Providence, Rhode Island (Megan L. Ranney).
The authors would like to thank Curtis Hayne for his assistance with the early stage of the literature review.
The views in the manuscript reflect those of the authors, not of the authors' institutions.
Conflict of interest: none declared.
REFERENCES
- 1. Richardson EG,Hemenway D. Homicide, suicide, and unintentional firearm fatality: comparing the United States with other high-income countries, 2003.J Trauma.2011;70(1):238–243. [DOI] [PubMed] [Google Scholar]
- 2. US Centers for Disease Control and Prevention.WISQARS (Web-based Injury Statistics Query and Reporting System).Washington, DC:Centers for Disease Control and Prevention;2010http://www.cdc.gov/injury/wisqars. Accessed February 25, 2015. [Google Scholar]
- 3. Cunningham RM,Carter PM,Ranney M et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study.JAMA Pediatr.2015;169(1):63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Greenspan AI,Kellermann AL. Physical and psychological outcomes 8 months after serious gunshot injury.J Trauma.2002;53(4):709–716. [DOI] [PubMed] [Google Scholar]
- 5. DiScala C,Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries.Pediatrics.2004;113(5):1306–1312. [DOI] [PubMed] [Google Scholar]
- 6. Howell EM,Abraham P. The Hospital Costs of Firearm Assaults.Washington, DC:The Urban Institute;2013:1–10. [Google Scholar]
- 7. Institute of Medicine and the National Research Council.Priorities for Research to Reduce the Threat of Firearm-Related Violence.Washington, DC:The National Academies Press;2013. [Google Scholar]
- 8. Cunningham R,Knox L,Fein J et al. Before and after the trauma bay: the prevention of violent injury among youth.Ann Emerg Med.2009;53(4):490–500. [DOI] [PubMed] [Google Scholar]
- 9. Muelleman RL,Reuwer J,Sanson TG et al. An emergency medicine approach to violence throughout the life cycle. SAEM Public Health and Education Committee.Acad Emerg Med.1996;3(7):708–715. [DOI] [PubMed] [Google Scholar]
- 10. Dowd MD,Sege RD;Council on Injury, Violence, and Poison Prevention Executive Committee et al. Firearm-related injuries affecting the pediatric population.Pediatrics.2012;130(5):e1416–e1423. [DOI] [PubMed] [Google Scholar]
- 11. American College of Emergency Physicians.Firearm safety and injury prevention.Irving, TX:American College of Emergency Physicians; http://www.acep.org/Clinical—Practice-Management/Firearm-Safety-and-Injury-PreventionPublished February 2001Updated April 2013. Accessed February 23, 2015. [Google Scholar]
- 12. Butkus R,Doherty R,Daniel H et al. Reducing firearm-related injuries and deaths in the United States: executive summary of a policy position paper from the American College of Physicians.Ann Intern Med.2014;160(12):858–860. [DOI] [PubMed] [Google Scholar]
- 13. American Medical Association.H-145.975 Firearm Safety and Research, Reduction in Firearm Violence, and Enhancing Access to Mental Health Care.Chicago, IL:American Medical Association; https://www.ama-assn.org/ssl3/ecomm/PolicyFinderForm.pl?site=www.ama-assn.org&uri=/resources/html/PolicyFinder/policyfiles/HnE/H-145.975.HTMPublished June 2013Updated June 2014. Accessed February 23, 2015. [Google Scholar]
- 14. Weinberger SE,Hoyt DB,Lawrence HC 3rd et al. Firearm-related injury and death in the United States: a call to action from 8 health professional organizations and the American Bar Association.Ann Intern Med.2015;162(7):513–516. [DOI] [PubMed] [Google Scholar]
- 15. Zaza S,Sleet DA,Thompson RS et al. Reviews of evidence regarding interventions to increase use of child safety seats.Am J Prev Med.2001;21(4 suppl):31–47. [DOI] [PubMed] [Google Scholar]
- 16. Nelson HD,Bougatsos C,Blazina I. Screening Women for Intimate Partner Violence and Elderly and Vulnerable Adults for Abuse: Systematic Review to Update the 2004 U.S. Preventive Services Task Force Recommendation.Rockville, MD:Agency for Healthcare Research and Quality;2012(Evidence synthesis no. 92. AHRQ publication no. 12-05167-EF-1). [PubMed] [Google Scholar]
- 17. Walton MA,Chermack ST,Shope JT et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial.JAMA.2010;304(5):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Walton MA,Resko S,Barry KL et al. A randomized controlled trial testing the efficacy of a brief cannabis universal prevention program among adolescents in primary care.Addiction.2014;109(5):786–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walton MA,Bohnert K,Resko S et al. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: one year outcomes.Drug Alcohol Depend.2013;132(3):646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jadad AR,Moore RA,Carroll D et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials.1996;17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 21. Higgins JPT,Green S, eds.Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]The Cochrane Collaboration;2011www.cochrane-handbook.org. [Google Scholar]
- 22. Wells GA,Shea B,O'Connell D et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.htmPublished January 2000. Accessed February 23, 2015.
- 23. Barkin SL,Finch SA,Ip EH et al. Is office-based counseling about media use, timeouts, and firearm storage effective? Results from a cluster-randomized, controlled trial.Pediatrics.2008;122(1):e15–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zatzick D,Russo J,Lord SP et al. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial.JAMA Pediatr.2014;168(6):532–539. [DOI] [PubMed] [Google Scholar]
- 25. Everett SA,Price JH,Bedell AW et al. Family practice physicians’ firearm safety counseling beliefs and behaviors.J Community Health.1997;22(5):313–324. [DOI] [PubMed] [Google Scholar]
- 26. Barkin S,Duan N,Fink A et al. The smoking gun: do clinicians follow guidelines on firearm safety counseling? Arch Pediatr Adolesc Med.1998;152(8):749–756. [DOI] [PubMed] [Google Scholar]
- 27. Barkin S,Fink A,Gelberg L. Predicting clinician injury prevention counseling for young children.Arch Pediatr Adolesc Med.1999;153(12):1226–1231. [DOI] [PubMed] [Google Scholar]
- 28. Betz ME,Barber CW,Miller M. Firearm restriction as suicide prevention: variation in belief and practice among providers in an urban emergency department.Inj Prev.2010;16(4):278–281. [DOI] [PubMed] [Google Scholar]
- 29. Butkus R,Weissman A. Internists’ attitudes toward prevention of firearm injury.Ann Intern Med.2014;160(12):821–827. [DOI] [PubMed] [Google Scholar]
- 30. Cassel CK,Nelson EA,Smith TW et al. Internists’ and surgeons’ attitudes toward guns and firearm injury prevention.Ann Intern Med.1998;128(3):224–230. [DOI] [PubMed] [Google Scholar]
- 31. Chaffee TA,Bridges M,Boyer CB. Adolescent violence prevention practices among California pediatricians.Arch Pediatr Adolesc Med.2000;154(10):1034–1041. [DOI] [PubMed] [Google Scholar]
- 32. Cohen LR,Runyan CW,Bowling JM. Social determinants of pediatric residents’ injury prevention counseling.Arch Pediatr Adolesc Med.1998;152(2):169–175. [DOI] [PubMed] [Google Scholar]
- 33. Grossman DC,Mang K,Rivara FP. Firearm injury prevention counseling by pediatricians and family physicians. Practices and beliefs.Arch Pediatr Adolesc Med.1995;149(9):973–977. [DOI] [PubMed] [Google Scholar]
- 34. Olson LM,Christoffel KK,O'Connor KG. Pediatricians’ experience with and attitudes toward firearms. Results of a national survey.Arch Pediatr Adolesc Med.1997;151(4):352–359. [DOI] [PubMed] [Google Scholar]
- 35. Olson LM,Christoffel KK,O'Connor KG. Pediatricians’ involvement in gun injury prevention.Inj Prev.2007;13(2):99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Price JH,Kinnison A,Dake JA et al. Psychiatrists’ practices and perceptions regarding anticipatory guidance on firearms.Am J Prev Med.2007;33(5):370–373. [DOI] [PubMed] [Google Scholar]
- 37. Shafii T,Rivara FP,Wang J et al. Screening adolescent patients admitted to the trauma service for high-risk behaviors: Who is responsible? J Trauma.2009;67(6):1288–1292. [DOI] [PubMed] [Google Scholar]
- 38. Traylor A,Price JH,Telljohann SK et al. Clinical psychologists’ firearm risk management perceptions and practices.J Community Health.2010;35(1):60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Webster DW,Wilson MEH,Duggan AK et al. Firearm injury prevention counseling: a study of pediatricians’ beliefs and practices.Pediatrics.1992;89(5 pt 1):902–907. [PubMed] [Google Scholar]
- 40. Becher EC,Christakis NA. Firearm injury prevention counseling: Are we missing the mark? Pediatrics.1999;104(3 pt 1):530–535. [DOI] [PubMed] [Google Scholar]
- 41. Cheng TL,DeWitt TG,Savageau JA et al. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues.Arch Pediatr Adolesc Med.1999;153(6):629–635. [DOI] [PubMed] [Google Scholar]
- 42. Thompson A,Price JH,Khubchandani J et al. Physician assistants training on firearm injury prevention.Patient Educ Couns.2012;86(3):348–353. [DOI] [PubMed] [Google Scholar]
- 43. Khubchandani J,Price JH,Dake JA. Firearm injury prevention training in Preventive Medicine Residency programs.J Community Health.2009;34(4):295–300. [DOI] [PubMed] [Google Scholar]
- 44. Slovak K,Brewer TW. Suicide and firearm means restriction: Can training make a difference? Suicide Life Threat Behav.2010;40(1):63–73. [DOI] [PubMed] [Google Scholar]
- 45. Slovak K,Brewer TW,Carlson K. Client firearm assessment and safety counseling: the role of social workers.Soc Work.2008;53(4):358–366. [DOI] [PubMed] [Google Scholar]
- 46. Solomon BS,Duggan AK,Webster D et al. Pediatric residents’ attitudes and behaviors related to counseling adolescents and their parents about firearm safety.Arch Pediatr Adolesc Med.2002;156(8):769–775. [DOI] [PubMed] [Google Scholar]
- 47. Delnevo CD,Hausman AJ. Injury-prevention counseling among residents of internal medicine.Am J Prev Med.2000;19(1):63–65. [DOI] [PubMed] [Google Scholar]
- 48. Giggie MA,Olvera RL,Joshi MN. Screening for risk factors associated with violence in pediatric patients presenting to a psychiatric emergency department.J Psychiatr Pract.2007;13(4):246–252. [DOI] [PubMed] [Google Scholar]
- 49. McManus BL,Kruesi MJP,Dontes AE et al. Child and adolescent suicide attempts: an opportunity for emergency departments to provide injury prevention education.Am J Emerg Med.1997;15(4):357–360. [DOI] [PubMed] [Google Scholar]
- 50. Gielen AC,McDonald EM,Forrest CB et al. Injury prevention counseling in an urban pediatric clinic. Analysis of audiotaped visits.Arch Pediatr Adolesc Med.1997;151(2):146–151. [DOI] [PubMed] [Google Scholar]
- 51. Goldberg BW,von Borstel ER,Dennis LK et al. Firearm injury risk among primary care patients.J Fam Pract.1995;41(2):158–162. [PubMed] [Google Scholar]
- 52. Barkin SL,Scheindlin B,Brown C et al. Anticipatory guidance topics: Are more better? Ambul Pediatr.2005;5(6):372–376. [DOI] [PubMed] [Google Scholar]
- 53. Wright MS.Pediatric injury prevention. Preparing residents for patient counseling.Arch Pediatr Adolesc Med.1997;151(10):1039–1043. [DOI] [PubMed] [Google Scholar]
- 54. Betz ME,Miller M,Barber C et al. Lethal means restriction for suicide prevention: beliefs and behaviors of emergency department providers.Depress Anxiety.2013;30(10):1013–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Price JH,Thompson A,Khubchandani J et al. Perceived roles of emergency department physicians regarding anticipatory guidance on firearm safety.J Emerg Med.2013;44(5):1007–1016. [DOI] [PubMed] [Google Scholar]
- 56. Borowsky IW,Ireland M. National survey of pediatricians’ violence prevention counseling.Arch Pediatr Adolesc Med.1999;153(11):1170–1176. [DOI] [PubMed] [Google Scholar]
- 57. Khubchandani J,Wiblishauser M,Price JH et al. Graduate psychiatric nurse's training on firearm injury prevention.Arch Psychiatr Nurs.2011;25(4):245–252. [DOI] [PubMed] [Google Scholar]
- 58. Finch SA,Weiley V,Ip EH et al. Impact of pediatricians’ perceived self-efficacy and confidence on violence prevention counseling: a national study.Matern Child Health J.2008;12(1):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kaplan MS,Adamek ME,Rhoades JA. Prevention of elderly suicide. Physicians’ assessment of firearm availability.Am J Prev Med.1998;15(1):60–64. [DOI] [PubMed] [Google Scholar]
- 60. Fallucco EM,Conlon MK,Gale G et al. Use of a standardized patient paradigm to enhance proficiency in risk assessment for adolescent depression and suicide.J Adolesc Health.2012;51(1):66–72. [DOI] [PubMed] [Google Scholar]
- 61. Price JH,Thompson AJ,Khubchandani J et al. Firearm anticipatory guidance training in psychiatric residency programs.Acad Psychiatry.2010;34(6):417–423. [DOI] [PubMed] [Google Scholar]
- 62. Johnson RM,Frank EM,Ciocca M et al. Training mental healthcare providers to reduce at-risk patients’ access to lethal means of suicide: evaluation of the CALM Project.Arch Suicide Res.2011;15(3):259–264. [DOI] [PubMed] [Google Scholar]
- 63. Morriss R,Gask L,Battersby L et al. Teaching front-line health and voluntary workers to assess and manage suicidal patients.J Affect Disord.1999;52(1-3):77–83. [DOI] [PubMed] [Google Scholar]
- 64. Frank E,Carrera JS,Prystowsky J et al. Firearm-related personal and clinical characteristics of US medical students.South Med J.2006;99(3):216–225. [DOI] [PubMed] [Google Scholar]
- 65. Becher EC,Cassel CK,Nelson EA. Physician firearm ownership as a predictor of firearm injury prevention practice.Am J Public Health.2000;90(10):1626–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Fargason CA Jr,Johnston C. Gun ownership and counseling of Alabama pediatricians.Arch Pediatr Adolesc Med.1995;149(4):442–446. [DOI] [PubMed] [Google Scholar]
- 67. Price JH,Bedell AW,Everett SA et al. Training in firearm safety counseling in family practice residency programs.J Community Health.1997;22(2):91–99. [DOI] [PubMed] [Google Scholar]
- 68. Price JH,Conley PM,Oden L. Training in firearm safety counseling in pediatric residency programs.Arch Pediatr Adolesc Med.1997;151(3):306–310. [DOI] [PubMed] [Google Scholar]
- 69. Zavoski RW,Burke GS,Lapidus GD et al. Injury prevention training in pediatric residency programs.Arch Pediatr Adolesc Med.1996;150(10):1093–1096. [DOI] [PubMed] [Google Scholar]
- 70. Abraham A,Cheng TL,Wright JL et al. Assessing an educational intervention to improve physician violence screening skills.Pediatrics.2001;107(5):e68. [DOI] [PubMed] [Google Scholar]
- 71. Dingeldein L,Sheehan K,Krcmarik M et al. Evaluation of a firearm injury prevention Web-based curriculum.Teach Learn Med.2012;24(4):327–333. [DOI] [PubMed] [Google Scholar]
- 72. Fendrich M,Kruesi MJP,Wislar JS et al. Implementing means restriction education in urban EDs.Am J Emerg Med.1998;16(3):257–261. [DOI] [PubMed] [Google Scholar]
- 73. Johnson CD,Fein JA,Campbell C et al. Violence prevention in the primary care setting: a program for pediatric residents.Arch Pediatr Adolesc Med.1999;153(5):531–535. [DOI] [PubMed] [Google Scholar]
- 74. Klein JD,Allan MJ,Elster AB et al. Improving adolescent preventive care in community health centers.Pediatrics.2001;107(2):318–327. [DOI] [PubMed] [Google Scholar]
- 75. LoConte NK,Gleason CE,Gunter-Hunt G et al. Standardized note template improves screening of firearm access and driving among veterans with dementia.Am J Alzheimers Dis Other Demen.2008;23(4):313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sangvai S,Cipriani L,Colborn DK et al. Studying injury prevention: practices, problems, and pitfalls in implementation.Clin Pediatr (Phila).2007;46(3):228–235. [DOI] [PubMed] [Google Scholar]
- 77. Stevens MM,Olson AL,Gaffney CA et al. A pediatric, practice-based, randomized trial of drinking and smoking prevention and bicycle helmet, gun, and seatbelt safety promotion.Pediatrics.2002;109(3):490–497. [DOI] [PubMed] [Google Scholar]
- 78. Johnston BD,Rivara FP,Droesch RM et al. Behavior change counseling in the emergency department to reduce injury risk: a randomized, controlled trial.Pediatrics.2002;110(2 pt 1):267–274. [DOI] [PubMed] [Google Scholar]
- 79. Grossman DC,Cummings P,Koepsell TD et al. Firearm safety counseling in primary care pediatrics: a randomized, controlled trial.Pediatrics.2000;106(1 pt 1):22–26. [DOI] [PubMed] [Google Scholar]
- 80. Kruesi MJP,Grossman J,Pennington JM et al. Suicide and violence prevention: parent education in the emergency department.J Am Acad Child Adolesc Psychiatry.1999;38(3):250–255. [DOI] [PubMed] [Google Scholar]
- 81. Brent DA,Baugher M,Birmaher B et al. Compliance with recommendations to remove firearms in families participating in a clinical trial for adolescent depression.J Am Acad Child Adolesc Psychiatry.2000;39(10):1220–1226. [DOI] [PubMed] [Google Scholar]
- 82. Sherman ME,Burns K,Ignelzi J et al. Firearms risk management in psychiatric care.Psychiatr Serv.2001;52(8):1057–1061. [DOI] [PubMed] [Google Scholar]
- 83. Oatis PJ,Fenn Buderer NM,Cummings P et al. Pediatric practice based evaluation of the Steps to Prevent Firearm Injury program.Inj Prev.1999;5(1):48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Albright TL,Burge SK. Improving firearm storage habits: impact of brief office counseling by family physicians.J Am Board Fam Pract.2003;16(1):40–46. [DOI] [PubMed] [Google Scholar]
- 85. Carbone PS,Clemens CJ,Ball TM. Effectiveness of gun-safety counseling and a gun lock giveaway in a Hispanic community.Arch Pediatr Adolesc Med.2005;159(11):1049–1054. [DOI] [PubMed] [Google Scholar]
- 86. Forbis SG,McAllister TR,Monk SM et al. Children and firearms in the home: a Southwestern Ohio Ambulatory Research Network (SOAR-Net) study.J Am Board Fam Med.2007;20(4):385–391. [DOI] [PubMed] [Google Scholar]
- 87. Bonds DE,Ellis SD,Weeks E et al. Patient attitudes toward screening.N C Med J.2007;68(1):23–29. [PubMed] [Google Scholar]
- 88. Shaughnessy AF,Cincotta JA,Adelman A. Family practice patients’ attitudes toward firearm safety as a preventive medicine issue: a HARNET study. Harrisburg Area Research Network.J Am Board Fam Pract.1999;12(5):354–359. [DOI] [PubMed] [Google Scholar]
- 89. Haught K,Grossman D,Connell F. Parents’ attitudes toward firearm injury prevention counseling in urban pediatric clinics.Pediatrics.1995;96(4 pt 1):649–653. [PubMed] [Google Scholar]
- 90. Webster DW,Wilson MEH,Duggan AK et al. Parents’ beliefs about preventing gun injuries to children.Pediatrics.1992;89(5 pt 1):908–914. [PubMed] [Google Scholar]
- 91. May JP,Martin KL. A role for the primary care physician in counseling young African-American men about homicide prevention.J Gen Intern Med.1993;8(7):380–382. [DOI] [PubMed] [Google Scholar]
- 92. Radant LJ,Johnson TM. The Wisconsin Research Network Firearm Safety Survey.WMJ.2003;102(4):46–50. [PubMed] [Google Scholar]
- 93. Hemenway D,Miller M. Public health approach to the prevention of gun violence.N Engl J Med.2013;368(21):2033–2035. [DOI] [PubMed] [Google Scholar]
- 94. Wintemute GJ.Responding to the crisis of firearm violence in the United States: comment on “Firearm legislation and firearm-related fatalities in the United States.” JAMA Intern Med.2013;173(9):740. [DOI] [PubMed] [Google Scholar]
- 95. Sege RD.Help wanted: studies of firearms injuries affecting children.Pediatrics.2013;132(2):367–368. [DOI] [PubMed] [Google Scholar]
- 96. Halpern-Felsher BL,Ozer EM,Millstein SG et al. Preventive services in a health maintenance organization: How well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med.2000;154(2):173–179. [DOI] [PubMed] [Google Scholar]
- 97. Jones NE.Injury prevention: a survey of clinical practice.J Pediatr Health Care.1992;6(4):182–186. [DOI] [PubMed] [Google Scholar]
- 98. Yonaka L,Yoder MK,Darrow JB et al. Barriers to screening for domestic violence in the emergency department.J Contin Educ Nurs.2007;38(1):37–45. [DOI] [PubMed] [Google Scholar]
- 99. Vokes NI,Bailey JM,Rhodes KV. “Should I give you my smoking lecture now or later?” Characterizing emergency physician smoking discussions and cessation counseling.Ann Emerg Med.2006;48(4):406–414,414.e1–414.e7. [DOI] [PubMed] [Google Scholar]
- 100. Delgado MK,Acosta CD,Ginde AA et al. National survey of preventive health services in US emergency departments.Ann Emerg Med.2011;57(2):104–108.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Bernstein E,Bernstein J,Feldman J et al. An evidence based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization.Subst Abus.2007;28(4):79–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Burke RC,Sepkowitz KA,Bernstein KT et al. Why don't physicians test for HIV? A review of the US literature.AIDS.2007;21(12):1617–1624. [DOI] [PubMed] [Google Scholar]
- 103. Betz ME,Arias SA,Miller M et al. Change in emergency department providers’ beliefs and practices after use of new protocols for suicidal patients.Psychiatr Serv.2015;66(6):625–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Madsen TE,Riese A,Choo EK et al. Effects of a Web-based educational module on pediatric emergency medicine physicians’ knowledge, attitudes, and behaviors regarding youth violence.West J Emerg Med.2014;15(5):615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. D'Onofrio G,Fiellin DA,Pantalon MV et al. A brief intervention reduces hazardous and harmful drinking in emergency department patients.Ann Emerg Med.2012;60(2):181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Simonetti JA,Mackelprang JL,Rowhani-Rahbar A et al. Psychiatric comorbidity, suicidality, and in-home firearm access among a nationally representative sample of adolescents.JAMA Psychiatry.2015;72(2):152–159. [DOI] [PubMed] [Google Scholar]
- 107. Grossman DC,Mueller BA,Riedy C et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries.JAMA.2005;293(6):707–714. [DOI] [PubMed] [Google Scholar]
- 108. Carter PM,Walton MA,Newton MF et al. Firearm possession among adolescents presenting to an urban emergency department for assault.Pediatrics.2013;132(2):213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Yarnall KS,Pollak KI,Østbye T et al. Primary care: Is there enough time for prevention? Am J Public Health.2003;93(4):635–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Cunningham RM,Chermack ST,Zimmerman MA et al. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up.Pediatrics.2012;129(6):1083–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Cunningham RM,Whiteside LK,Chermack ST et al. Dating violence: outcomes following a brief motivational interviewing intervention among at-risk adolescents in an urban emergency department.Acad Emerg Med.2013;20(6):562–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Loftin C,McDowall D,Wiersema B et al. Effects of restrictive licensing of handguns on homicide and suicide in the District of Columbia.N Engl J Med.1991;325(23):1615–1620. [DOI] [PubMed] [Google Scholar]
- 113. Kreitman N.The coal gas story. United Kingdom suicide rates, 1960–71.Br J Prev Soc Med.1976;30(2):86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Cantor CH,Slater PJ. The impact of firearm control legislation on suicide in Queensland: preliminary findings.Med J Aust.1995;162(11):583–585. [DOI] [PubMed] [Google Scholar]
- 115. Lester D,Leenaars A. Suicide rates in Canada before and after tightening firearm control laws.Psychol Rep.1993;72(3 pt 1):787–790. [DOI] [PubMed] [Google Scholar]
- 116. Snowdon J,Harris L. Firearms suicides in Australia.Med J Aust.1992;156(2):79–83. [DOI] [PubMed] [Google Scholar]
- 117. Hawton K,Simkin S,Deeks J et al. UK legislation on analgesic packs: before and after study of long term effect on poisonings.BMJ.2004;329(7474):1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Mott JA,Wolfe MI,Alverson CJ et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality.JAMA.2002;288(8):988–995. [DOI] [PubMed] [Google Scholar]
- 119. Beautrais AL.Effectiveness of barriers at suicide jumping sites: a case study.Aust N Z J Psychiatry.2001;35(5):557–562. [DOI] [PubMed] [Google Scholar]
- 120. Bennewith O,Nowers M,Gunnell D. Effect of barriers on the Clifton suspension bridge, England, on local patterns of suicide: implications for prevention.Br J Psychiatry.2007;190:266–267. [DOI] [PubMed] [Google Scholar]
- 121. Kapusta ND,Etzersdorfer E,Krall C et al. Firearm legislation reform in the European Union: impact on firearm availability, firearm suicide and homicide rates in Austria.Br J Psychiatry.2007;191:253–257. [DOI] [PubMed] [Google Scholar]
- 122. Gunnell D,Fernando R,Hewagama M et al. The impact of pesticide regulations on suicide in Sri Lanka.Int J Epidemiol.2007;36(6):1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Barber CW,Miller MJ. Reducing a suicidal person's access to lethal means of suicide: a research agenda.Am J Prev Med.2014;47(3 suppl 2):S264–S272. [DOI] [PubMed] [Google Scholar]
- 124. Ranney ML,Choo EK,Cunningham RM et al. Acceptability, language, and structure of text message-based behavioral interventions for high-risk adolescent females: a qualitative study.J Adolesc Health.2014;55(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Ranney ML,Choo EK,Wang Y et al. Emergency department patients’ preferences for technology-based behavioral interventions.Ann Emerg Med.2012;60(2):218–227 e48. [DOI] [PubMed] [Google Scholar]
- 126. Rhodes KV,Lauderdale DS,Stocking CB et al. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department.Ann Emerg Med.2001;37(3):284–291. [DOI] [PubMed] [Google Scholar]
- 127. The Brady Center to Prevent Gun Violence, American Academy of Pediatrics.ASK campaign.Washington, DC:The Brady Center; http://askingsaveskids.org/sites/default/files/ASK-Toolkit_0.pdfPublished June 2014Updated June 20, 2015Accessed June 24, 2015. [Google Scholar]
- 128. Education Development Center, Inc.Children's safety network.Waltham, MA:Education Development Center; http://www.childrenssafetynetwork.org/firearm-resource-guide-2013Published April 2013Accessed February 23, 2015. [Google Scholar]
- 129. Liberati A,Altman DG,Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration.Ann Intern Med.2009;151(4):W65–W94. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.