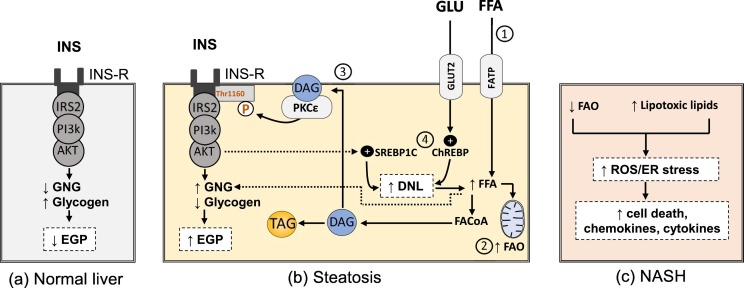
Fig. 2.
Altered signaling and pathogenic mechanisms in hepatocytes during NAFLD progression a) insulin signaling in healthy hepatocytes suppress endogenous glucose production through inhibition of gluconeogenesis and increasing glycogen synthesis b) steatotic hepatocytes are characterized by disturbed lipid metabolism i.e., 1) there is increase in FFA influx which enters the liver through fatty acid transport proteins (FATP) and leads to 2) increased mitochondrial fatty acid oxidation, 3) formation of lipid toxic intermediates e.g. sn 1,2 DAG which stimulates PKCε to phosphorylate Thr1160 in insulin receptor leading to hepatic insulin resistance i.e., increased gluconeogenesis and decreased glycogen synthesis. Again, FFA metabolites e.g. acetyl CoA could directly stimulate gluconeogenesis [25] 4) increased glucose enters the liver mainly through glucose transporter (GLUT2) and activates ChREBP pathway. Insulin-signaling activates SREBP1C pathway too. Both pathways increase DNL c) after progression to NASH, mitochondrial flexibility is lost leading to decreased fatty acid oxidation. Together with other toxic intermediate lipid, ER stress and ROS generation increase leading to hepatocytes death and release of inflammatory cytokines and chemokines. AKT, protein kinase B; ChREBP, carbohydrate response element-binding protein; DAG, sn 1,2 diacylglycerol; DNL, de novo lipogenesis; EGP, endogenous glucose production; ER, endoplasmic reticulum; FAO, fatty acid oxidation; FFA, free fatty acids; GLU, glucose; GNG, gluconeogenesis; INS, insulin; INS-R, insulin resistance; IR, insulin receptor; PI3K, phosphatidylinositol-3-kinase; PKC, protein kinase C; ROS, reactive oxygen species; SREBP1C; sterol regulatory element-binding proteins; TAG, triacylglycerol.