Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is transmitted primarily via respiratory droplets, contact with contaminated surfaces, or free-floating aerosols.1 , 2 The American Academy of Ophthalmology recommends the use of surgical masks and commercially available slit-lamp shields (Breath Shields; Carl Zeiss AG, Oberkochen, Germany).3 However, a lack of evidence exists regarding the true efficacy of slit-lamp shields. We attempted to replicate the spread of infected aerosols and large droplets in the clinical setting of a slit-lamp examination to evaluate the efficacy of protective equipment in reducing the risk of viral transmission.
This study adhered to the Declaration of Helsinki and institutional review board approval was not required. Aerosols were defined as smaller light particles that remain suspended in the air because of slowly settling velocity, whereas large droplets were defined as heavier particles that fall rapidly after a downward trajectory.4 The experimental setup (Fig S1, available at www.aaojournal.org) consisted of a slit lamp (B900 Slit Lamp; Haag-Streit Holding AG, Köniz, Switzerland), a mannequin face that represented the ophthalmologist, and a spray bottle at the chin rest that represented respiratory particle production from the patient. A particle produced by the spray bottle had a peak velocity of 4.0 meters/second and a maximum horizontal distance of 2.35 m, which was comparable to particle behavior by coughing or sneezing. A high-speed camera capturing 1000 frames/second (Chronis 1.4; Kron Technologies, Inc., Burnaby, Canada) was used for video recordings (Fig 1 ). This process was repeated for 3 simulations: (1) no protective equipment; (2) commercially available slit-lamp breath shield installed; and (3) mask placed in front of the spray bottle (Fig S1). For simulation 3, 5 types of masks were used: an N95 respirator (N95 particulate respiratory 8210; 3M, Alexandria, MN), 3 surgical masks of different brands and bacterial filtration efficiencies ranging from 95% to 99%, and a cloth mask (bacterial filtration efficiency, 55%).
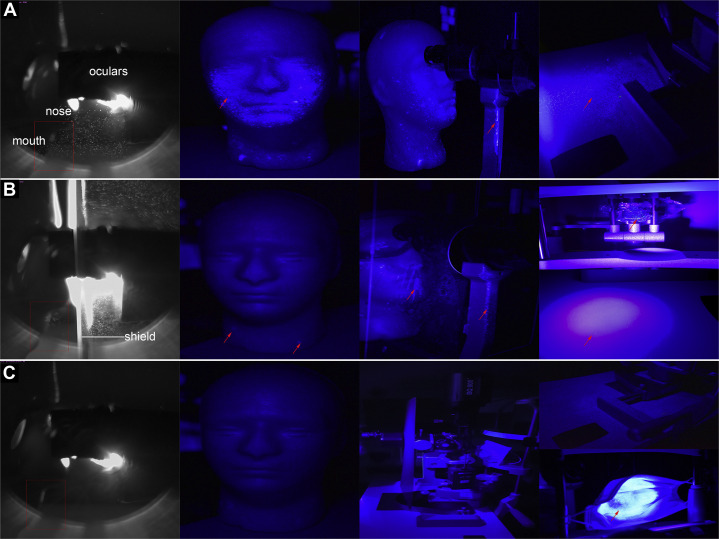
Figure 1.
Each row of pictures labeled (A), (B), and (C) represents the described simulations 1, 2, and 3, respectively. The first column shows selected freeze frames with the highest aerosol count from each simulation’s video recording. The positions of the oculars of the slit lamp, slit-lamp shield, mannequin’s nose, and mouth are labeled for reference. The rectangular area bordered by red represents the region of interest, with a standardized area used for manual counting of aerosol particle numbers. The subsequent 3 columns depict examination of the mannequin, slit-lamp apparatus, and table under ultraviolet A light. Red arrows indicate areas of hyperfluorescence. In simulation 1, hyperfluorescent areas were visualized on the mannequin, slit lamp, and table. In simulation 2, hyperfluorescent areas were not visualized on the mannequin’s face but were present on its neck, the slit-lamp apparatus and shield, and the table. In simulation 3, hyperfluorescent areas were not visualized on the mannequin, slit lamp, shield, or table, but were present on the inner surface of the face mask.
The outcome measure for aerosol transmission was the number of aerosol particles in a predefined region (Fig 1, rectangle area bordered in red [31.2 × 19.6 mm]). In total, we included 26 consecutive frames (6 ms apart) from the video recordings of each simulation. Two trained graders (Y.J.X., T.T.Y.F.) independently counted the number of aerosol particles within this region, with the mean of the 2 used as the final count. A 1-way analysis of covariance test was used to compare the number of particles in this region for each simulation. To determine the risk of large droplet transmission, identical simulations were repeated with Glo Germ liquid (Glo Germ Company, Moab, UT). The slit lamp, table, and mannequin were examined under ultraviolet A light for fluorescent droplets.
In simulation 1 (Fig 1A), aerosols remained suspended in the air, with the highest density anterior to the mannequin’s mouth and nose. This density was reduced in simulation 2 (Fig 1B). In simulation 3 (Fig 1C), no particles could be observed for all 5 types of masks. The mean ± standard deviation number of particles in the region of interest was 42.7 ± 34.5 for simulation 1, 12.3 ± 5.7 for simulation 2, and 0.0 ± 0.0 for simulation 3 (P < 0.001; Fig S2, available at www.aaojournal.org). Post hoc analysis showed that simulation 3 had a statistically significantly lower aerosol count than simulation 2, which in turn had a lower aerosol count than simulation 1 (P < 0.05). Hyperfluorescent areas were found on the lower half of the mannequin, slit lamp, and table for simulation 1. In simulation 2, hyperfluorescent areas were seen on the mannequin’s neck, the shield, the slit lamp, and the table. In simulation 3, the hyperfluorescent area was observed only on the inner surface of the masks (Fig 1).
The close proximity between the ophthalmologist and the patient increases risk of respiratory transmission of virus.4 With or without the slit-lamp shield, aerosols congregated at the highest density in the region of the ophthalmologist’s nose and mouth. Because SARS-CoV-2 remains viable in aerosols for hours,2 a high concentration of aerosols poses an inhalation threat to ophthalmologists. Although slit-lamp shields reduced the risk of large-droplet transmission, they were limited in protection against infectious aerosols that were present on the side of the shield facing the mannequin (Fig 1B). This could be because of minor leaks at the oculars of the slit lamp where the shield is attached. Studies have demonstrated a lower efficacy of face shields against smaller aerosols because they can travel around the face shields.5 When using a slit-lamp shield alone, the slit lamp, shield, and table can act as fomites for contact transmission; proper disinfection practices are needed because SARS-CoV-2 has surface stability for up to 72 hours.2
Our study showed that all 5 types of face masks on patients provided the most complete protection against aerosol and droplet transmission. This could be explained because bacterial filtration efficiency was a measurement of particles filtered out at a pore size of 1.0 to 5.0 μm, which was too small to be detected by the camera. Ma et al6 demonstrated that surgical masks can block up to 97% of SARS-CoV-2 via aerosol transmission. However, some studies involving human participants demonstrated poor efficacy of face masks, which could be attributed to poor facial fit, leading to leakage of infectious particles. In our study, the mask provided complete coverage over the small spray nozzle, which could have accounted for a better level of protection.
Limitations included technological constraints of the camera, which might have missed smaller aerosol particles. Statistical significance in reduction referred exclusively to count consistency and was not a direct estimate of reduced infection risk. The use of a spray bottle to simulate droplet or aerosol production from the patient cannot exactly replicate the actions of coughing or sneezing. Further studies are needed to interrogate the efficacy of shields and masks against viable SARS-CoV-2 in respiratory particles exceeding the minimal infectious dose. These ideally should be examined with a validated cough aerosol simulator.
In conclusion, slit-lamp shields provide added protection for ophthalmologists but should be used together with other forms of personal protective equipment. All patients should wear face masks because of their efficacy in reducing aerosol and droplet transmission.
Footnotes
Financial Disclosure(s): The author(s) have no proprietary or commercial interest in any materials discussed in this article.
HUMAN SUBJECTS: No human subjects were included in this study. The National University of Singapore deemed this study exempt from IRB approval. All research adhered to the tenets of the Declaration of Helsinki. Informed consent was not required.
No animal subjects were included in this study.
Author Contributions:
Conception and design: Chuan, Bin Razali, Shaffiee, Xing, Fei, Chee, Koh
Analysis and interpretation: Chuan, Bin Razali, Chee, Koh
Data collection: Bin Razali, Shaffiee, Xing, Fei
Obtained funding: N/A; Study was performed as part of the authors' regular employment duties. No additional funding was provided.
Overall responsibility: Chuan, Bin Razali, Shaffiee, Xing, Fei, Chee, Koh
Supplementary Data
References
- 1.Burki T.K. Coronavirus in China. Lancet Respir Med. 2020;8(3):238. doi: 10.1016/S2213-2600(20)30056-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Academy of Ophthalmology Important coronavirus updates for ophthalmologists. 2020. https://www.aao.org/headline/alert-important-coronavirus-context Accessed 15.04.20.
- 4.Kutter J.S., Spronken M.I., Fraaij P.L. Transmission routes of respiratory viruses among humans. Curr Opin Virol. 2018;28:142–151. doi: 10.1016/j.coviro.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberge R.J. Face shields for infection control: a review. J Occup Environ Hyg. 2016;13(4):235–242. doi: 10.1080/15459624.2015.1095302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma QX, Shan H, Zhang HL, et al. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020; Mar 31. https://doi.org/10.1002/jmv.25805. Online ahead of print. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.