1. Introduction and Background
1.1. About the Biennial Stevens Johnson Syndrome Symposium
The SJS Symposium was founded by Elizabeth Phillips, Professor of Medicine and Pharmacology and Director of Personalized Immunology at the Oates Institute for Experimental Therapeutics at Vanderbilt University Medical Center and Director of the Centre for Clinical Pharmacology and Infectious Diseases at the Institute for Immunology and Infectious Diseases, Murdoch University in Perth, Western Australia. Her current work focuses on defining genetic, molecular, and cellular signatures in severe cutaneous adverse drug reactions such as SJS/TEN that will guide prevention and management.
1.2.
Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) is an immunologically mediated and primarily drug-induced systemic disease that, although rare, has a high collective burden. SJS/TEN is an acute life-threatening disease; however, the high short- and long-term morbidity and mortality are also a significant burden on patients, their families, and society. SJS/TEN is the most severe type of drug-induced disease, characterized by skin necrosis, mucous membrane involvement inflammation, and ocular surface disease that can result in severe visual impairment.
Although multiple disciplines are involved in the research and care of SJS/TEN, provincial, national, and international coordination to maximize research efforts and networking has been challenging. On March 2, 2017, the first of such meetings, “SJS/TEN 2017: Building Multidisciplinary Networks to Drive Science & Translation,” was held in conjunction with the American Academy of Dermatology meeting in Orlando, Florida. The meeting attracted 142 participants, including 30 trainees (medical residents and fellows).
Although this is not an ophthalmology-specific meeting, ocular science always plays a central role in the meeting’s agenda. The 2019 symposium was scheduled just before the annual ARVO meeting in Vancouver, BC to expand the participation. There were 164 total attendees from 19 countries, of whom 23 (14%) were eye health specialists. The 19 countries represented were Australia, Brazil, Canada, China, France, Germany, India, Ireland, Israel, Japan, Netherlands, Republic of Korea, Singapore, South Africa, Spain, Taiwan, Thailand, UK, and US.
The next meeting is planned for 2021.
2. 2019 Biennial Meeting
2.1. General
The 2019 meeting was co-chaired by Elizabeth Phillips, Bruce Carleton, Professor of Pediatrics at the University of British Columbia, and Wen-Hung Chung, Professor and Director of Department of Dermatology at the Chang Gung Memorial Hospital in Taiwan. The meeting took place at the Sheraton Vancouver Wall Centre and the British Columbia Children’s Hospital Research Institute. In addition to ophthalmology over 10 specialties were represented including immunology, dermatology, genetics, gynecology, burn surgery and regulatory and governmental agencies such as the US Food and Drug Administration, Health Canada, The European Medicines Agency, Health Sciences Authority, Singapore, the National Institute of Allergy and Infectious Diseases (NIAID), National Human Genome Research Institute (NHGRI), National Institute of Arthritis and Musculoskeletal and Skin Disease (NIAMS), Genome British Columbia, Genome Canada and the Canadian Institute for Health Research. A highlight of the meeting was the representation of over 50 SJS/TEN patients and family members permanently impacted by SJS/TEN.
The topics covered included the implementation of pharmacogenomics, racial disparities in SJS/TEN, regional networks and registries, controversies in acute care, global regulation, genomic approaches to prediction and prevention, special populations and challenges, and updates in ocular science. The patients and families in attendance and their stories highlighted the long-term ocular morbidity associated with SJS/TEN.
This portion of the meeting summary highlights updates in ocular science.
2.2. Ocular Science
1 -. The first speaker was Hajirah (Haji) Saeed from Massachusetts Eye and Ear Infirmary who discussed acute ocular care in SJS/TEN
She described the medical and public health burden of ocular disease in SJS/TEN and the resultant need for prompt acute care to optimize short and long-term outcomes. Even cases with modest damage in the acute phase are at risk of developing chronic debilitating disease. The key risk factor for chronic progression appears to be a disordered eyelid margin anatomy.
SJS/TEN is characterized by widespread apoptosis of keratinocytes, caused by activation of natural killer cells, cytotoxic T-cells, and tumor necrosis factor alpha (TNF-a). Thus systemic immunosuppression has been proposed for SJS/TEN in the acute phase for both systemic and ocular disease. However, there is minimal data to support or refute its use for ocular disease.
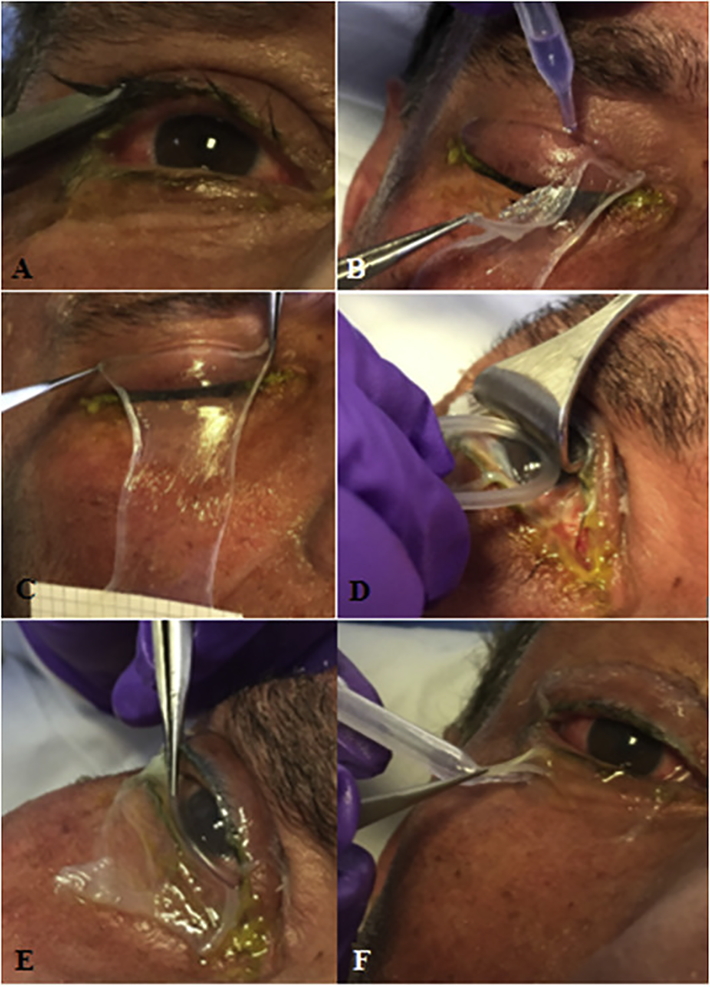
The only acute treatment known to mitigate chronic disease is amniotic membrane transplantation (AMT), possibly in conjunction with topical medications. Traditionally, AMT is performed by securing multiple amnion pieces to the eyelids (and sometimes also the globe) with sutures, often necessitating the use of an operating room. She described a new sutureless technique which uses cyanoacrylate glue and can be done at bedside in these acutely ill patients. (1) See Figure 1. It reduces length of procedure, time to procedure, patient and physician discomfort, and tissue manipulation. The level of sedation and pain control necessary is also significantly reduced. Her preliminary data shows no difference in efficacy and outcomes between the traditional sutured method and the newer glued method.
Figure 1. Procedure for sutureless amniotic membrane transplantation (AMT) in the right eye of a patient with Stevens-Johnson syndrome with ocular surface and eyelid margin epithelial defects.
A) Upper and lower eyelashes are trimmed. B) Cyanoacrylate glue is used to secure the amniotic membrane (AM) sheet (5 × 10 cm) to the upper eyelid. Care is taken to ensure glue is placed at least 4 mm above the eyelid margin. C) AM is held across the upper eyelid for 30 s to ensure adhesion. D) Desmarres lid retractor is used to retract the upper eyelid to allow the symblepharon ring to be placed in the superior fornix. E) The symblepharon ring is then tucked into the inferior fornix. F) The inferior margin of the AM is secured to the lower eyelid with cyanoacrylate glue. The patient should be able to close the eye without any lagophthalmos caused by the symblepharon ring. Reprinted from Shanbhag et al. (1) with permission from Elsevier.
2 -. Next, Alfonso Iovieno from University of British Columbia discussed corneal pathophysiology
Ocular complications are often the only long-term complication of SJS/TEN, with acute disease leading to chronic complications. Acutely, SJS/TEN results in varying degrees of necrosis and ulceration of conjunctival and corneal epithelium. There is conjunctival monocytic perivascular infiltrate and conjunctival elastotic degeneration. In the chronic phase, epithelial hyperplasia/metaplasia, substantia propria fibrosis, and chronic inflammatory infiltration is seen.
The most common chronic symptom is dry eye and involves all components of the tear film (aqueous, lipid and mucous layers). Squamous metaplasia of the meibomian gland (MG) orifices, and inspissation and atrophy of the MGs affect the lipid layer; scarring of primary and accessory lacrimal gland ductules, and primary inflammation of the lacrimal glands result in aqueous deficiency; and loss of conjunctival goblet cells result in mucous layer deficiency. Additionally, alteration of eyelid mechanics from cicatrization contribute to chronic irritation and exposure.
Clinically, the chronic phase may be characterized by symblephara, ankyloblephara, cicatrizing conjunctivitis, cicatricial entropion, trichiasis, fornix foreshortening, distichiasis, and/or eyelid margin keratinization. The friction of the disordered eyelid margin against the ocular surface can result in corneal epithelial defects, ulcers, scarring, pannus, and limbal stem cell deficiency (LSCD) and corneal perforation. LSCD presents a therapeutic challenge in these complex eyes (discussed below).
Other significant chronic complications include microbial keratitis, ectasia, and recur- rent/persistent inflammation. Early involvement of an ophthalmologist in the acute phase is crucial to mitigate these chronic complications.
3 -. Mee Kum Kim from Seoul National University College of Medicine discussed the management of ocular complications with a focus on limbal stem cell deficiency
The goals for acute disease include downregulating inflammation, preventing eyelid malposition, and preserving limbal stem cell function. Targeted acute care with topical steroids, antibiotics, and amniotic membrane transplantation when indicated can reduce the incidence and severity of complications associated with these problems.
Her discussion of the treatment of chronic ocular surface disease in SJS revolved primarily around limbal stem cell deficiency. She described several approaches to treatment including conjunctivolimbal allograft (CLAL), living donor related keratolimbal graft (Lr KLAL), and keratolimbal allograft (KLAL). Autograft procedures cannot be done in SJS/TEN given the bilateral nature of the disease. Adjunctive treatment includes correction of eyelid abnormalities and scleral contact lenses. Keratoprosthesis may also be considered. Surgical reconstruction of the ocular surface generally does not fare well in SJS/TEN and the rejection rate of limbal allograft transplantation is higher than that of other indications.
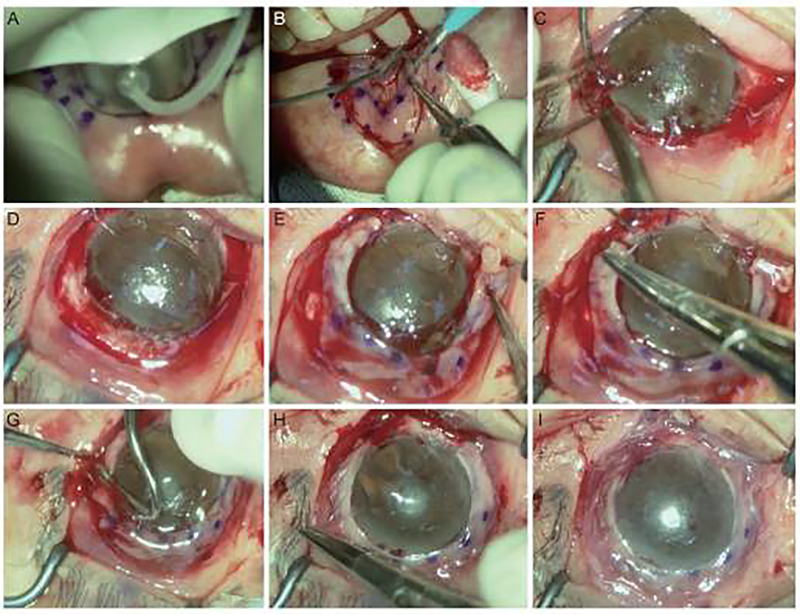
An alternative to limbal allografts is cultivated oral mucosal epithelial transplantation (COMET) which has comparable short-term results to KLAL and may have better outcomes in the long-term. It also precludes the need for systemic immunosuppression. However, the cost and resources needed for cultivation can be prohibitive due to limited resources. Dr. Kim described then use of a “simple” oral mucosal epithelial transplantation (SOMET) which involves direct transplantation of a circumferentially-trephined oral mucosal graft for ocular surface reconstruction (Figure 2). Short-term results in SJS/TEN patients appear favorable. (2)
Figure 2. Key surgical steps of autologous oral mucosal graft transplantation in patients with limbal stem cell deficiency.
(A) Markings for inside incisions are made with a 9-mm- diameter donor vacuum trephine using gentian violet ink, and outside markings are made with a 14-mm intraoperative keratometer. (B) The oral mucosal graft is dissected using a Beaver mini-blade or Vanna scissors in a ring or a crescent-shaped strip of 5-mm width and 250-pm depth. (C) Prior to graft transplantation, the fibrotic vascular membrane and pannus overlying the cornea are fully removed and (D) a conjunctival peritomy is circumferentially performed along the limbal stem cell-deficient area. (E) The free mucosal graft is placed onto the limbus and (F) the inside margin of the graft was fixed with 10–0 nylon anchoring sutures. (G) Tissue glue is used to firmly attach the mucosal graft to the bed. (H) After trimming excess tissue in the outside margin of the graft, it is sutured to the conjunctiva with continuous 10–0 nylon sutures to hold the graft onto the limbus. (I) Transient amniotic membrane transplantation is performed to protect the transplanted graft during the healing process. Reprinted from Choe et al. (2) with permission from The Korean Ophthalmological Society https://creativecommons.org/licenses/by-nc/3.0/.
4 -. The last speaker was Mayumi Ueta of Kyoto Prefectural University of Medicine. She discussed the immunogenetics of SJS/TEN
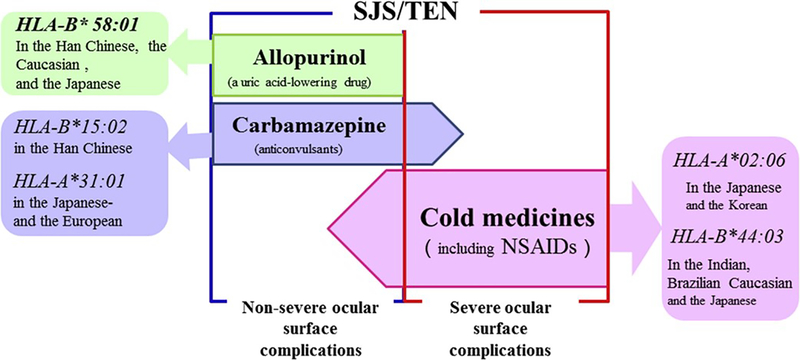
Her work suggests that there are different phenotypes of ocular involvement in SJS/TEN: those with severe ocular complications (SOCs) and those without SOCs. Genetic studies in different populations suggest there are certain genetic predispositions to developing SOCs. The etiology of these SOCs may be associated with cold-medicine induced SJS/TEN. “Cold medicine” includes a combination of NSAIDs, paracetamol, and other drugs.
HLA Class I genes have been found to be associated with cold-medicine induced SJS and SOCs in Brazilian, Indian, Thai, Japanese, and Korean populations. Allopurinol and carbamazepine induced SJS/TEN, on the other hand, may be associated with less SOCs (Figure 3).
Figure 3. Particular HLA alleles are associated with different causative drugs.
Reprinted from Ueta et al (3) with permission from Elsevier.
There are strong genetic associations between SJS/TEN caused by certain drugs and specific ethnicities. Carbamazepine demonstrates the strongest of these associations, with HLA-B*15:02 implicated in the Han Chinese. Other associations include those between allopurinol-induced SJS/TEN and HLA-B*58:01 in the Han Chinese, Caucasians, and Japanese, and carbamazepine- induced SJS/TEN and HLA-A*31:01 in the Japanese and Europeans.
Other non-HLA polymorphisms have also been associated with SJS/TEN including single nucleotide polymorphisms in the toll-like receptor 3 (TLR3) gene and the Ikaros family zinc finger 1 gene (IKZF1). These have both been associated with cold-medicine induced SJS/TEN in the Japanese population. Dr. Ueta hypothesized that the multiple genes associated with SJS/TEN might constitute a network of interactions in the setting of abnormal host immunity. A resultant lack of balance between genes and epistatic interactions between HLA and genes outside of the MHC may trigger the mucocutaneous inflammation seen in SJS with SOCs. (4)
4. Acknowledgments
Funding for this conference was made possible (in part) by NIH (1 R13-AR74889-01) National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and all co-funding support provided by: National Human Genome Research Institute (NHGRI), National Center for Advancing Translational Sciences (NCATS), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Eye Institute (NEI), National Institute of Allergy and Infectious Diseases (NIAID), U.S. Food and Drug Administration, Canadian Institutes of Health Research, Genome British Columbia.
Funding was also supported by the University of British Columbia Faculty of Medicine; University of British Columbia Faculty of Pharmaceutical Sciences; BC Children’s Hospital Research Institute; Dr. Hongsheng Wang (Institute of Dermatology, Chinese Academy of Medical Sciences & Peking Union Medical College) and Dr. Wen-Hung Chung (Chang Gung Memorial Hospital); British Columbia Provincial Health Services Authority; Stevens-Johnson Syndrome Consulting Group, Inc; Eli Lilly Canada, Inc; Murdoch Global University, Australia, Dubai, Singapore; Dynacare; Illumina; Sandoz Canada, Biopharmaceuticals; Tissue Tech/Ocular Surface; Pharmigene, Inc.
Footnotes
Declarations of interest
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shanbhag SS, Chodosh J, Saeed HN. Sutureless amniotic membrane transplantation with cyanoacrylate glue for acute Stevens-Johnson syndrome/toxic epidermal necrolysis . Ocul Surf. 2019. July;17(3):560–564. Epub 2019 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choe HR, Yoon CH, Kim MK. Ocular Surface Reconstruction Using Circumferentially- trephined Autologous Oral Mucosal Graft Transplantation in Limbal Stem Cell Deficiency. Korean J Ophthalmol. 2019. February;33(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ueta M, Sawai H, Sotozono C, et al. IKZF1, a new susceptibility gene for cold medicine-related Stevens-Johnson syndrome/toxic epidermal necrolysis with severe mucosal involvement. J Allergy Clin Immunol. 2015. June;135(6):1538–45.e17. [DOI] [PubMed] [Google Scholar]
- 4.Ueta M Results of Detailed Investigations into Stevens-Johnson Syndrome With Severe Ocular Complications. Invest Ophthalmol Vis Sci. 2018. November;59(14):DES183–DES191. [DOI] [PubMed] [Google Scholar]