Abstract
Background
Electronic consultations (e-consults) are asynchronous clinician-to-clinician exchanges within the electronic health record (EHR).
Objective
We sought to demonstrate the utility of e-consults in allergy/immunology (A/I) inpatient consultations.
Methods
Inpatients ≥18 years of age for whom an A/I consultation was requested were eligible for an e-consult. An e-consult was completed if considered appropriate by the A/I physician with recommendations made in the EHR. In-person consultation was performed for inpatients if deemed necessary. Likert scale satisfaction data were collected from requesting providers after the e-consultation. Cost was calculated using time-based billing codes plus the cost of penicillin allergy evaluation, if appropriate.
Results
Of the 109 inpatient consults, 78 (71.6%) were completed through an e-consult and 31 (28.4%) were completed by an in-person consult. The most common indication for an inpatient consult was evaluation of penicillin allergy in 73 (67%) patients. The most common reason to complete an in-person consult was the need to complete penicillin skin testing in 17 of the 31 (55%) patients. E-consults were completed in less time than in-person consults (15 minutes, interquartile range [IQR]: 10-15 vs 60 minutes, IQR: 45-60, P < .001) and had a shorter turnaround time (1 hour, IQR: 0.5-2 vs 7 hours, IQR: 3-19, P < .001). Management recommendations were followed at a similar rate regardless of type of consult (88% of e-consults vs 96% of in-person consults, P = .162). A total of 97% of requesting providers reported an “excellent” or “good” impression of e-consults. E-consults were less costly than in-person consults.
Conclusions
E-consults have utility in providing inpatient A/I consultation and may have advantages over in-person evaluation, while adequately maintaining provider satisfaction.
Key words: E-consult, Electronic consultation, Allergy/immunology, Penicillin allergy, Inpatient
Abbreviations used: A/I, Allergy/immunology; COVID-19, Novel coronavirus infection; DC, Direct challenge; e-consult, Electronic consultation; EHR, Electronic health record; IQR, Interquartile range; PST, Penicillin skin test; RGH, Rochester General Hospital; WRVU, Work relative value unit
What is already known about this topic? There are outpatient data for electronic consultations (e-consults) in allergy/immunology (A/I) but no data for inpatient A/I consultations.
What does this article add to our knowledge? We demonstrate that A/I inpatient e-consults are feasible, potentially less costly, and maintain requesting provider satisfaction for certain conditions.
How does this study impact current management guidelines? E-consults are a strategy to improve A/I access in inpatient settings and are particularly relevant during the novel coronavirus infection pandemic.
Electronic consultations (e-consults) are asynchronous clinician-to-clinician exchanges within the electronic health record (EHR).1 E-consults are less formal than an in-person provider/patient consultation but more formal than a “curbside” consult between health care providers.1 Advantages of e-consults include improved patient access to specialist care, potential cost savings,2 and convenience for both health care providers and patients.1 The utility and feasibility of e-consults has been demonstrated across multiple specialties, including cardiology,3 , 4 gastroenterology,5 endocrinology,6 infectious disease,7 nephrology,8 and dermatology.9
Although the only data currently available addressing allergy/immunology (A/I) e-consults come from the outpatient setting,10 the inpatient setting is prime to incorporate asynchronous evaluations. Indeed, scarcity of inpatient A/I availability has been cited as a limiting factor for collaborating with inpatient antimicrobial stewardship programs,11 and e-consults could be a strategy to bridge this gap. A 2010 study of inpatient A/I consultations revealed a decline in A/I consults over the study period and showed that the most common referrals were for adverse drug reactions, urticaria/angioedema, and anaphylaxis.12 In the wake of a concerted effort toward multidisciplinary antibiotic stewardship at our institution, internal data reflected an increased demand for inpatient A/I consults over the past 4 years, predominately for the evaluation of adverse drug reactions. We therefore sought to demonstrate that a significant proportion of A/I inpatient consultations could be addressed through e-consults while preserving referring inpatient provider satisfaction.
Methods
Setting and data collection
This was a single-center, prospective study conducted at Rochester General Hospital (RGH), a 528-bed tertiary care medical center, from October 1, 2019, through March 31, 2020. Of note, at RGH, approximately 15% to 20% of inpatients report a penicillin allergy (internal data). The study was approved by the RGH institutional review board, and the e-consult pilot program was also endorsed by the RGH Department of Medicine.
Inpatients ≥18 years of age for whom an A/I consultation was requested by the primary team or for whom a consultation was recommended by the Antimicrobial Stewardship team were considered eligible for an e-consult. Inpatient coverage was split equally among 4 A/I physicians for 7 days (Monday AM to Monday AM) of coverage at a time. The decision as to whether an e-consult was appropriate was determined by the on call A/I physician.
For patients deemed appropriate for e-consults, the A/I physician reviewed the EHR for completeness of the medical history and confirmed with the primary team if an e-consult was acceptable to them and the patient. If necessary, in the case of drug allergy consultations, inpatient stewardship or infectious disease pharmacists were available to confirm the drug allergy history with the patient per AI physician request. Management recommendations included a standardized disclaimer (Figure 1 ). In-person consultation was performed for patients in whom this was deemed necessary. For penicillin allergy e-consults, recommendations included continued avoidance of penicillin-based antibiotics, a direct challenge (DC) to penicillin as previously described,13 or a challenge to a cephalosporin. If penicillin skin testing (PST) was deemed necessary based on the historical reaction, this was completed as an in-person consult. We surveyed referring providers regarding satisfaction after the e-consult. The 3 survey questions were based on a 5-point Likert scale ranging from 1 (strongly disagree or poor) to 5 (strongly agree to excellent).
Figure 1.
E-consult template. EHR, Electronic health record.
Cost analysis
Time-based billing codes used for e-consults were 99446 (5-10 minutes), 99447 (11-20 minutes), 99448 (21-30 minutes), and 99449 (>30 minutes), and cost of the e-consult was determined based on codes billed. For in-person consultations, billing codes were 99221, 99222, and 99223, and cost of the in-person consultation was based on codes billed. In the case of inpatient PST performed, the cost of penicilloyl polylysine, penicillin G, and skin testing supplies ($128.05) was added to the procedure time ($326.50) plus the amount billed for the A/I inpatient consult. Cost for the PST procedure was determined per the Revenue Integrity fee schedule, which is Rochester Regional Health's fee schedule of usual and customary prices billed for the specific type of testing. For patients who underwent DC, the cost of amoxicillin plus pharmacist preparation time ($15) was added to the amount billed for the A/I consult.
Outcome measures and data analysis
We collected the following data: patient age and gender, reason for consultation, primary service, time to complete consult (time spent performing e-consult or inpatient consult noted by the A/I physician), turnaround time (time from when consult requested until complete), whether recommendations were implemented, and referring provider satisfaction scores. STATA software (StataCorp LLC, College Station, TX) was used for statistical analysis. Baseline characteristics are reported as medians and interquartile ranges (IQRs) for continuous variables and proportions for binomial variables. We used a nonparametric, Wilcoxon-rank sum test to compare variables of interest between the in-person and e-consult cohort. Microsoft Excel software (Office 365; Microsoft Corporation, Redmond, WA) was used to create the figures.
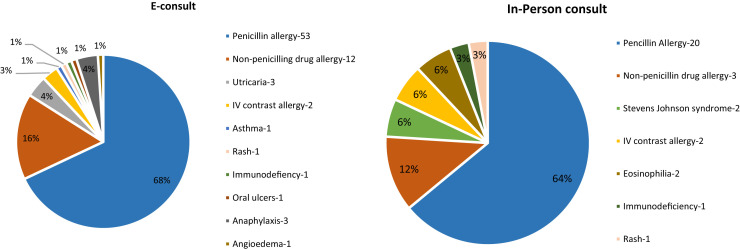
Results
We analyzed 109 inpatient consults (mean of 4.2 per week). Of these, 68 (62.4%) of the patients were female, and 41 (37.6%) were male. The median age of the entire cohort was 62 (IQR: 47.8-73.3) years. The internal medicine service requested 85 (78.0%) consults, followed by 14 (12.8%) requested by surgery and 5 (4.6%) each by obstetrics/gynecology and emergency medicine. The most common indications for consultation were evaluation of a history of penicillin allergy in 73 (67.0%) patients and other historical drug allergies in 15 (13.8%) patients. Other less common indications for requesting a consultation are listed in Table I .
Table I.
Demographics
| E-consult | In-person consult | |
|---|---|---|
| Patients, n (%) | 78 (72) | 31 (28) |
| Age (y) | 61 (range, 47-73) | 67 (range, 52-76) |
| Female, n (%) | 51 (65) | 17 (54) |
| Primary service, n (%) | ||
| Internal medicine | 58 (74) | 27 (87) |
| Surgery | 12 (15) | 2 (7) |
| Emergency medicine | 4 (5) | 1 (3) |
| Obstetrics and gynecology | 4 (5) | 1 (3) |
| Indication for consult, n (%) | ||
| Penicillin allergy | 53 (68) | 20 (64) |
| Nonpenicillin drug allergy | 12 (16) | 3 (12) |
| Anaphylaxis | 3 (4) | 0 |
| IV contrast allergy | 2 (3) | 2 (6) |
| Urticaria | 3 (4) | 0 |
| Stevens Johnson syndrome | 0 | 2 (6) |
| Eosinophilia | 0 | 2 (6) |
| Rash | 1 (1) | 1 (3) |
| Immunodeficiency | 1 (1) | 1 (3) |
| Asthma | 1 (1) | 0 |
| Angioedema | 1 (1) | 0 |
| Oral ulcers | 1 (1) | 0 |
IV, Intravenous.
Of the 109 inpatient consults, 78 (71.6%) were completed through an e-consult and 31 (28.4%) were completed by an in-person consult. Thirteen of the 78 (16.7%) e-consults used assistance from the inpatient stewardship pharmacist to confirm the details of the patient history. There was no difference in the age of the cohort evaluated through an e-consult (61 [IQR: 47-73] years) versus an in-person consult (67 [IQR: 52-76] years), P = .479 (Table II ). There was also no difference in the gender of patients evaluated through an e-consult (65% female) versus an in-person consult (54% female), P = .209. E-consults were completed in significantly less time than an in-person consult, with a median time of 15 (IQR: 10-15) minutes, versus 60 (IQR: 45-60) minutes for an in-person consult, P < .001. In addition, the turnaround time to complete an e-consult was 1 hour (IQR: 0.5-2 hours), versus 7 (IQR: 3-19) hours for an in-person consult, P < .001. Management recommendations made by the A/I consultant were followed at a similar rate regardless of type of consults (88% of e-consults vs 96% of in-person consults, P = .162).
Table II.
Comparison of variables between e-consults and in-person consults
| E-consult (n = 78) | In-person consult (n = 31) | P value | |
|---|---|---|---|
| Age (y) | 61 (47-73) | 67 (52-76) | .479 |
| Female, n (%) | 51 (65) | 17 (54) | .209 |
| Time taken to complete∗ (min) | 15 (10-15) | 60 (45-60) | <.001 |
| Turnaround time† (h) | 1 (0.5-2) | 7 (3-19) | <.001 |
| Recommendations followed, n (%) | 69 (88) | 30 (96) | .162 |
| Work relative value units | 0.7 (0.4-0.7) | 2.6 (1.9-3.8) | <.001 |
| Physician reimbursement ($) | 42.05 (21.2-42) | 221.18 (163.4-327.4) | <.001 |
Continuous variables are reported as medians and interquartile ranges; binary variables are reported as proportions.
Bold indicates statistical significance.
Includes review of relevant patient information including examination (in-person consult only).
Time to complete evaluation from the time consult was requested.
For e-consults, the frequency of time-based billing codes was as follows: 99447 used for 45 (57.5%) encounters, 99446 used for 26 (33.3%) encounters, 99448 used for 4 (5.1%) encounters, and 99449 used for 3 (3.8%) encounters. For in-person consults, 99221 was used for 7 (22.6%) encounters, 99222 for 20 (64.5%) encounters, and 99223 for 4 (12.9%) encounters. The work relative value units (WRVUs) for e-consults were 0.7 (IQR: 0.4-0.7) WRVUs, versus 2.6 (IQR: 1.9-3.8) WRVUs for an in-person consult, P < .001. Median reimbursement for e-consults was $42.05 (IQR: $21.20-$42.00), versus $221.18 (IQR: $163.40-$327.40) for in-person consults, P < .001. For the evaluation of reported penicillin allergy, the most common indication for inpatient AI consultation, the median cost of the evaluation by an e-consult was $57.05 (IQR: $36.20-$99.50), versus $657.73 (IQR: $657.70-$657.70) for an in-person consult, P < .001.
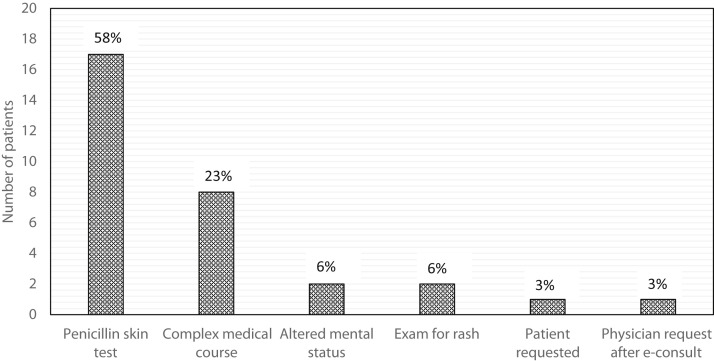
Indications for inpatient consultation were similar for both e-consult and in-person consult (Figure 2 ). The most common reason to complete an in-person consult rather than an e-consult was the need to complete PST in 17 (58%) patients, followed by the A/I consultant feeling that the patient warranted an in-person consult due to having a complex medical course (23%) (Figure 3 ). Additional reasons included the patient having altered mental status (6%), the patient requiring a physical examination for evaluation of a rash (6%), and 1 patient (3%) requesting an in-person consult. One additional in-person consult was completed after an e-consult where recommendations were not followed.
Figure 2.
Indications for e-consults versus in-person consults. IV, Intravenous.
Figure 3.
Reason for completing in-person consult rather than e-consult.
Of the 78 e-consults performed, 73 (93.6%) of the requesting providers answered 3 brief provider satisfaction questions (Table III ). Fifty-three of 73 (73%) reported an “excellent” overall impression for e-consults for an inpatient A/I consultation. An additional 18 (25%) reported a “good” impression, whereas 1 provider reported a “neutral” impression and another reported a “fair” impression. When asked if they were satisfied with their e-consult encounter, 60 (82%) providers “strongly agreed,” whereas 11 (15%) agreed and 2 (3%) were neutral. Lastly, when asked if an e-consult was as satisfactory as an in-person evaluation, 44 (60%) providers “strongly agreed” with this statement, 26 (36%) providers “agreed,” and 3 (4%) providers were “neutral.” No providers felt that an e-consult was “poor” for inpatient A/I consultation, and no providers expressed dissatisfaction with their e-consult experience or disagreed that an e-consult was as satisfactory as an in-person consult.
Table III.
Provider satisfaction survey scores for e-consults (n = 73)
| Question | Poor | Fair | Neutral | Good | Excellent |
|---|---|---|---|---|---|
| What is your overall impression of an e-consult for an in-patient allergy evaluation? n (%) | 0 | 1 (1) | 1 (1) | 18 (25) | 53 (73) |
| Statement | Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
|---|---|---|---|---|---|
| Overall, I was satisfied with my e-consult encounter, n (%) | 0 | 0 | 2 (3) | 11 (15) | 60 (82) |
| An e-consult was as satisfactory as an in-person evaluation, n (%) | 0 | 0 | 3 (4) | 26 (36) | 44 (60) |
Discussion
Although a previous work by Phadke et al10 showed the applicability of A/I e-consults in the outpatient setting, our study is the first to demonstrate the feasibility and utility of inpatient A/I e-consults, including novel insights gained from provider satisfaction questions. There are unifying themes between the study by Phadke et al and ours, most notably how e-consults can help expand A/I access in the inpatient as well as outpatient settings. We also demonstrate that historical adverse reactions to drugs, most notably a remote history of penicillin allergy (where a direct oral challenge is appropriate), are particularly fitting for an e-consult.
Significantly reduced turnaround time to a completed e-consult and a shorter time spent on the e-consult as compared with in-person consults mirror the experience from previous studies.10 An e-consult can be completed by a thorough review of medical records in the EHR during the course of an A/I physician's outpatient responsibilities without the need for travel to the hospital, significantly reducing work hours as compared with an in-person consult. Furthermore, our analysis shows that an e-consult was completed a median of 6 hours sooner as compared with an in-person consult. The expedited specialty recommendations to the primary team may facilitate more timely transition to first-line antibiotics for patients evaluated for adverse drug reactions or could potentially impact patient length of stay in the hospital, an important metric for hospital efficiency.14
We have previously shown the utility and safety of inpatient DC to penicillin-based antibiotics in patients with a remote history of cutaneous-only reactions in place of PST.13 In the current study, we demonstrate that these types of low-risk historical penicillin reactions can transition a step further to an e-consult. Penicillin allergy was the most common indication for an A/I inpatient consultation, accounting for 67% of all consults. We found that almost 73% of the consults for evaluation of reported penicillin allergy were accomplished via e-consult and subsequent DC. The ability to remotely delabel penicillin allergy is a significant advancement for antimicrobial stewardship, yet keeps this skill under the purview of the A/I specialist. The benefits of inpatient penicillin allergy delabeling have been well established,15, 16, 17 and more widespread uptake of e-consults by A/I physicians could expand access to this important area of expertise.
Although our cost analysis is rudimentary, it suggests that e-consults may be cost saving for the health system. For the evaluation of inpatient penicillin allergy, the potential cost savings are even more pronounced, given the additional cost associated with PST versus a DC. Although time-based reimbursement for the A/I physician is significantly less for an e-consult as compared with an in-person consult, conducting an inpatient evaluation through an e-consult saves time and affords the specialist the ability to be more productive in the outpatient setting. For A/I specialists who do not currently provide inpatient consultative services, an integration of e-consults into their practice would provide an additional, albeit modest, opportunity for revenue and networking with a referral base.
Importantly, we demonstrate that requesting providers were satisfied with e-consults. The majority of requesting providers (98%) had a “good” or “excellent” opinion of e-consults, with the vast majority reporting overall satisfaction with the e-consult compared with a traditional in-person consult. There are no similar studies gauging referring provider satisfaction with e-consults in A/I, but our data are similar to a study surveying primary care physician impressions of e-consults from multiple specialties that showed that the majority of those surveyed (>75%) reported that an e-consult improved their patient care plan.18 In addition, 88% of our e-consult recommendations were followed by the requesting providers, corresponding with previously published A/I and other specialty data. In the outpatient setting, Phadke et al10 reported that 73% of A/I e-consult recommendations were followed, whereas Wrenn et al19 reported that 65% to 85% of other subspecialty recommendations (cardiology, gastroenterology, pulmonary, endocrinology, nephrology, rheumatology) were followed by primary care.
Our data also suggest that certain conditions may not be appropriate for an e-consult. In our analysis, A/I physicians decided whether an inpatient consult should be completed electronically or in-person. However, in other models, primary providers place the referral for e-consults,10 , 20 so developing specialty-specific criteria for appropriate indications for e-consultation will be important if asynchronous telemedicine is going to be increasingly used. Certain evaluations, such as PST, obviously require an in-person or telemedicine evaluation.21 Although the numbers in our study were low, we believe that larger cohorts would support that severe cutaneous adverse reactions to drugs, such as drug reaction with eosinophilia and systemic symptoms or Stevens Johnson syndrome, along with potentially complex medical conditions, such as eosinophilia, would be best served by in-person consultations.
The strengths of our study include its focus on the inpatient setting, our characterization of both e-consults and in-person consults, and the cost comparison of the 2 modalities. Gauging provider satisfaction with the e-consult platform could help further support adoption of this evaluation strategy in our field. Our report of the utility of e-consults is particularly timely given the unprecedented social distancing recommendations due to novel coronavirus infection (COVID-19).22 E-consults can be employed while maintaining social distancing and preserving personal protective equipment for essential inpatient health care providers. E-consults are also an avenue for A/I specialists to continue to offer expertise in both the inpatient and outpatient setting during COVID-19 restrictions.
We acknowledge limitations to our study. Increased patient numbers would be optimal, but we terminated our data collection sooner than planned due to rapidly instituted COVID-19 institutional restrictions. We recognize our lack of patient outcomes data and believe that this area deserves further study. Our cost analysis is rudimentary, though we strongly suspect that more robust economic analyses will continue to demonstrate favorable overall cost comparisons for e-consults versus in-person consultations. We also did not formally track physician travel time with in-person consults, but have demonstrated this to significantly improve in prior work where A/I physicians provided inpatient management recommendations without traveling to the hospital.21 Lastly, we did not track patient satisfaction data, which would augment our results, though we only had 1 e-consult converted to an in-person consultation per patient request. As with any single-center study, the generalizability may be limited depending on the characteristics of other hospital settings.
In conclusion, our study demonstrates the feasibility and utility of inpatient A/I e-consults. Inpatient e-consults are efficient, potentially cost saving, and provide management recommendations that are followed while maintaining adequate provider satisfaction. The application of e-consults is timely in the current era of COVID-19, and we envision this approach to be an important strategy to optimize access to inpatient A/I care. E-consults allow A/I physicians to provide their expertise not by working harder but by working smarter.
Footnotes
No funding was received for this work.
Conflicts of interest: S. Shahzad Mustafa received research grant from CSL Behring; and is in speaker's bureau at Sanofi/Regeneron, Genentech, AstraZeneca, and CSL Behring. A. Ramsey received research grant from CSL Behring; and is in speaker's bureau at Sanofi/Regeneron. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Vimalananda V.G., Gupte G., Seraj S.M., Orlander J., Berlowitz D., Fincke B.G. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21:323–330. doi: 10.1177/1357633X15582108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson D., Villagra V.G., Coman E., Ahmed T., Porto A., Jepeal N. Reduced cost of specialty care using electronic consultations for Medicaid patients. Health Aff (Millwood) 2018;37:2031–2036. doi: 10.1377/hlthaff.2018.05124. [DOI] [PubMed] [Google Scholar]
- 3.Bauer B.S., Nguyen-Phan A.L., Ong M.K., Ziaeian B., Nguyen K.L. Cardiology electronic consultations: efficient and safe but consultant satisfaction is equivocal. J Telemed Telecare. 2020;26:341–348. doi: 10.1177/1357633X19828130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raber I., McCarthy C.P., Wasfy J.H. Integrating inpatient electronic consultations in cardiology fellowship. J Am Coll Cardiol. 2019;74:1151–1155. doi: 10.1016/j.jacc.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 5.Bhavsar I., Wang J., Burke S.M., Dowdell K., Hays R.A., Intagliata N.M. Electronic consultations to hepatologists reduce wait time for visits, improve communication, and result in cost savings. Hepatol Commun. 2019;3:1177–1182. doi: 10.1002/hep4.1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson D., Porto A., Koppel J., Macri G., Wright M. Impact of endocrinology eConsults on access to endocrinology care for Medicaid patients. [published online ahead of print February 5, 2020]. Telemed J E Health. [DOI] [PubMed]
- 7.Strymish J., Gupte G., Afable M.K., Gupta K., Kim E.J., Vimalananda V. Electronic consultations (E-consults): advancing infectious disease care in a large veterans affairs healthcare system. Clin Infect Dis. 2017;64:1123–1125. doi: 10.1093/cid/cix058. [DOI] [PubMed] [Google Scholar]
- 8.Schettini P., Shah K.P., O'Leary C.P., Patel M.P., Anderson J.B., Cho A.H. Keeping care connected: e-consultation program improves access to nephrology care. J Telemed Telecare. 2019;25:142–150. doi: 10.1177/1357633X17748350. [DOI] [PubMed] [Google Scholar]
- 9.Naka F., Lu J., Porto A., Villagra J., Wu Z.H., Anderson D. Impact of dermatology eConsults on access to care and skin cancer screening in underserved populations: a model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78:293–302. doi: 10.1016/j.jaad.2017.09.017. [DOI] [PubMed] [Google Scholar]
- 10.Phadke N.A., Wolfson A.R., Mancini C., Fu X., Goldstein S.A., Ngo J. Electronic consultations in allergy/immunology. J Allergy Clin Immunol Pract. 2019;7:2594–2602. doi: 10.1016/j.jaip.2019.05.039. [DOI] [PubMed] [Google Scholar]
- 11.Trubiano J.A., Beekmann S.E., Worth L.J., Polgreen P.M., Thursky K.A., Slavin M.A. Improving antimicrobial stewardship by antibiotic allergy delabeling: evaluation of knowledge, attitude, and practices throughout the emerging infections network. Open Forum Infect Dis. 2016;3:ofw153. doi: 10.1093/ofid/ofw153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otto H.F., England R.W., Quinn J.M. Inpatient allergy/immunology consultations in a tertiary care setting. Allergy Asthma Proc. 2010;31:244–251. doi: 10.2500/aap.2010.31.3331. [DOI] [PubMed] [Google Scholar]
- 13.Ramsey A., Mustafa S.S., Holly A.M., Staicu M.L. Direct challenges to penicillin-based antibiotics in the inpatient setting. J Allergy Clin Immunol Pract. 2020;8:2294–2301. doi: 10.1016/j.jaip.2020.02.033. [DOI] [PubMed] [Google Scholar]
- 14.Rotter T., Kinsman L., James E., Machotta A., Gothe H., Willis J. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;3:CD006632. doi: 10.1002/14651858.CD006632.pub2. [DOI] [PubMed] [Google Scholar]
- 15.Shenoy E.S., Macy E., Rowe T., Blumenthal K.G. Evaluation and management of penicillin allergy: a review. JAMA. 2019;321:188–199. doi: 10.1001/jama.2018.19283. [DOI] [PubMed] [Google Scholar]
- 16.Blumenthal K.G., Lu N., Zhang Y., Walensky R.P., Choi H.K. Recorded penicillin allergy and risk of mortality: a population-based matched cohort study. J Gen Intern Med. 2019;34:1685–1687. doi: 10.1007/s11606-019-04991-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macy E., Contreras R. Health care use and serious infection prevalence associated with penicillin “allergy” in hospitalized patients: a cohort study. J Allergy Clin Immunol. 2014;133:790–796. doi: 10.1016/j.jaci.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 18.Olayiwola J.N., Potapov A., Gordon A., Jurado J., Magana C., Knox M. Electronic consultation impact from the primary care clinician perspective: outcomes from a national sample. J Telemed Telecare. 2019;25:493–498. doi: 10.1177/1357633X18784416. [DOI] [PubMed] [Google Scholar]
- 19.Wrenn K., Catschegn S., Cruz M., Gleason N., Gonzales R. Analysis of an electronic consultation program at an academic medical centre: primary care provider questions, specialist responses, and primary care provider actions. J Telemed Telecare. 2017;23:217–224. doi: 10.1177/1357633X16633553. [DOI] [PubMed] [Google Scholar]
- 20.Ahmed S., Kelly Y.P., Behera T.R., Zelen M.H., Kuye I., Blakey R. Utility, appropriateness, and content of electronic consultations across medical subspecialties: a cohort study. Ann Intern Med. 2020;172:641–647. doi: 10.7326/M19-3852. [DOI] [PubMed] [Google Scholar]
- 21.Staicu M.L., Holly A.M., Conn K.M., Ramsey A. The use of telemedicine for penicillin allergy skin testing. J Allergy Clin Immunol Pract. 2018;6:2033–2040. doi: 10.1016/j.jaip.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention CDC coronavirus disease 2019 (COVID 19) https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html Available from: