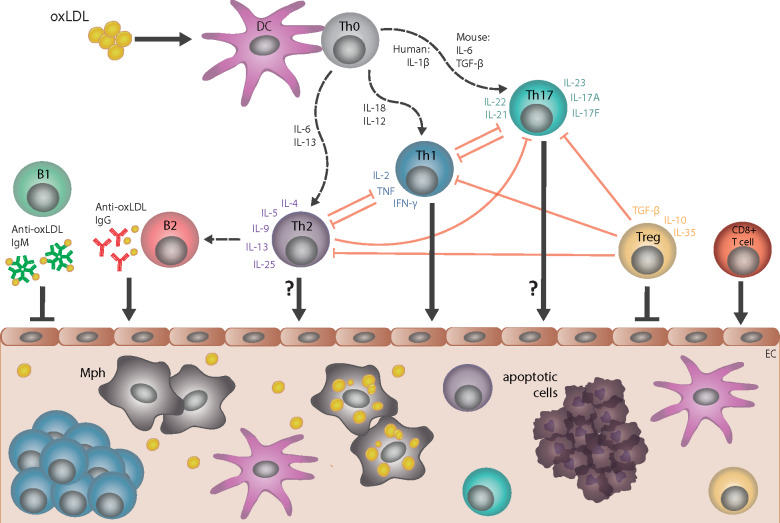
Figure 3.
Cellular and humoral immune responses in atherosclerosis. Dendritic cells (DC) take up several forms of modified low-density lipoprotein (LDL), including oxidized LDL (oxLDL), and present specific epitopes (e.g. apolipoprotein B peptides) to naive T cells (Th0), which induces differentiation into CD4+ T helper 1 (Th1), T helper 2 (Th2), T helper 17 (Th17), or T regulatory (T reg) cell subtypes; multiple cytokines control such differentiation. CD4+ T-cell subtypes, together with specific cytokines that they secrete, provide help to B cells and regulate the activity of other T-cell subtypes. The pro-atherogenic role of interferon gamma (IFN-γ)-secreting Th1 cells and the anti-atherogenic effect of interleukin-10/transforming growth factor beta (IL-10/TGF-β)-secreting T regulatory cells are well established. However, the role of Th2 and Th17 in atherogenesis is less clear, as opposing effects of cytokines associated with these respective subtypes have been described. Cytotoxic CD8+ T cells can promote atherogenesis. Anti-oxLDL immunoglobulin (Ig)M antibodies produced by B1 cells are atheroprotective, whereas anti-oxLDL IgG antibodies produced by B2-cell subsets are likely pro-atherogenic. All of these cell types may infiltrate the arterial wall at sites of ongoing plaque development, with the possible exception of Th2 and Th17 cell types. EC, endothelial cell; Mph, monocyte-derived macrophage.