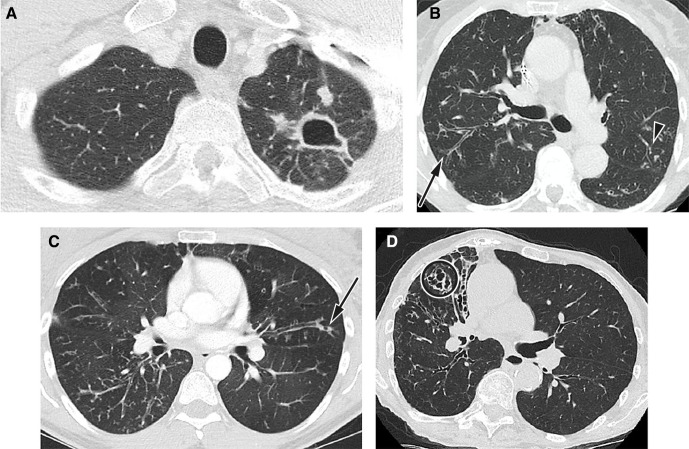
Figure 1.
Radiological imaging features typical of NTM lung infection. (A) Fibrocavitatory NTM-PD in a patient who has M. kansasii. Axial CT image shows a cavity in the apex of the left upper lobe with adjacent satellite nodules. (B) Nodular–bronchiectatic NTM-PD. CT image from a 75-year-old female patient with MAC. Axial CT image at the carina shows bronchiectasis and bronchial wall thickening in the posterior segment of the right upper lobe (arrow) with additional scattered areas of peripheral bronchiectasis, mucus plugging and centrilobular nodularity in the left upper (arrowhead) and lower lobes. (C) Nodular–bronchiectatic NTM-PD in a patient with variant cystic fibrosis who has grown MAC and M. abscessus. Axial CT image just below the carina shows widespread bronchiectasis and bronchial wall thickening with centrilobular nodules in the right lower lobe. Peripheral mucus plugging is a more common finding in NTM-PD and air bubbles or lucency is often seen within the mucus (arrow). There is an ancillary finding of air trapping causing lucent areas of lung. (D) Nodular–bronchiectatic NTM-PD in a patient who has MAC. There is more severe bronchiectasis in the middle lobe, which is cystic and varicose in appearance (circle). There are ancillary findings of chest wall deformity with volume loss in the right hemithorax and little chest wall body fat. Reproduced by the kind permission of Dr Joanne Cleverley and Dr Besma Musaddaq of the Department of Radiology, Royal Free Hospital, London, UK. CT, computerised tomography; MAC, Mycobacterium avium complex; NTM, non-tuberculous mycobacteria; NTM-PD, non-tuberculous mycobacterial pulmonary disease.