Abstract
Coronavirus disease (COVID-19) emerged in Wuhan, China, in December 2019 and rapidly became a global pandemic, with the number of confirmed infections worldwide reaching 1 million by the start of April 2020 and 3 million less than a month later. COVID-19 can be encountered with different clinical presentations. We present the case of a patient with COVID-19 in the etiology presenting with acute renal failure.
Keywords: Acute renal failure, SARS-CoV-2, acute respiratuary distress syndrome
Introduction
Coronavirus disease (COVID-19) emerged in Wuhan, China, in December 2019 and rapidly became a global pandemic, with the number of confirmed infections reaching 1 million by the start of April 2020 and 3 million less than a month later, worldwide. Acute respiratory failure is among the leading causes of death due to COVID-19. Although it usually presents with respiratory failure in older patients, individuals with mild COVID-19 may be asymptomatic or present with subtler symptoms, such as loss of taste and smell, sore throat, fatigue, and joint pain [1, 2].
In this case report, we describe a patient who presented to the emergency department with metabolic acidosis resulting from acute renal failure and was subsequently diagnosed with COVID-19 by nasopharyngeal swab polymerase chain reaction (PCR).
Case Report
An 80-year-old man presented to our emergency department with complaints of poor general condition and fatigue for the last 18 h. The patient’s relatives reported that the patient had not left his home for the past 15 days and had no contact with anyone suspected of having COVID-19. However, his son was delivering groceries to his home once a week. Based on the statement given by his relatives, the patient had no known diseases and had undergone surgery in 2015 to repair an inguinal hernia.
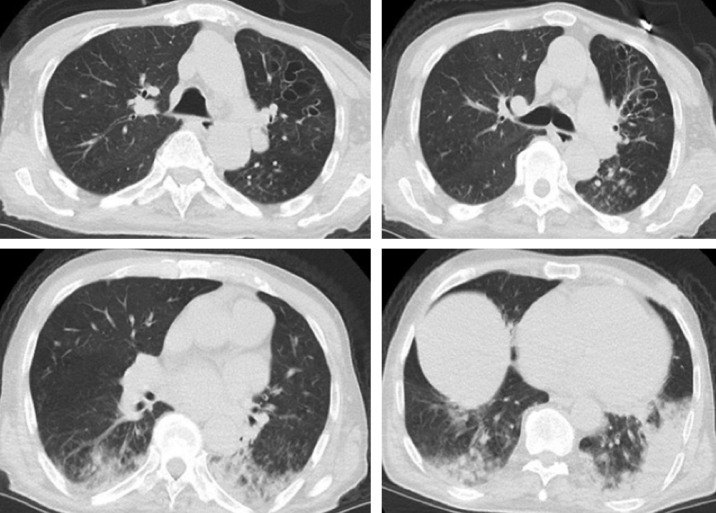
On physical examination, the patient’s blood oxygen saturation was 86% at room temperature, respiratory rate was 38/min, blood pressure was 170/110 mmHg, and brachial/radial heart rate was 150 beats/min and regular. The patient exhibited disorientation to time and space, and the results of neurological evaluation indicated that he had delirium. Posterior lung auscultation revealed bilateral basal inspiratory rales. Laboratory tests results were as follows: white blood cells=16,760/μL, lymphocyte count=330/μL, neutrophils=15,870/μL, hemoglobin=20.4 g/dL, platelets=119,000/μL, lactate dehydrogenase=557 U/L, calcium=7.8 mg/dL, albumin=3.01 g/dL, creatine=7.42 mg/dL, sodium=131 mmoL/L, blood-urea nitrogen=139.25 mg/dL, glomerular filtration rate=8.09 mL/min, troponin=88.1 ng/dL, D-dimer=3012 ng/mL, fibrinogen=890 mg/dL, prothrombin time=20.4 s, C-reactive protein=26.2 mg/dL, and ferritin=1124 ng/mL. On blood gas analysis, pH=7.23, SaO2=92.4%, PaO2=74 mmHg, PaCO2=28.1 mmHg, and HCO3=14.4 mEq/L. Posterior-anterior chest X-ray showed increased prominence of the bronchovascular structures with areas of pleural-based consolidation in the lower lobes of both lungs. Chest computed tomography revealed tubular and cystic bronchiectatic dilations in the bronchial structures in the upper lobe of the left lung, especially those leading to the anterior segment, with bronchial wall thickening at these levels. Areas of ground-glass opacity were noted adjacent to the areas of cystic bronchiectasis. The lower lobes of both lungs showed areas of ground-glass opacity and tree-in-bud appearance surrounding consolidation that contained air bronchograms, and the findings were reported as being primarily indicative of viral pneumonia (Figure 1). The diffusion MRI scan of the brain ordered due to delirium was reported as normal. The patient was admitted to the pulmonary diseases intensive care unit with acute renal failure and suspected COVID-19. PCR analysis of the nasopharyngeal swab sample was positive for COVID-19. In line with the Ministry of Health guidelines for management of adult patients, renal dose-adjusted treatment was initiated with hydroxychloroquine 200 mg every 12 h loading dose and 50 mg maintenance dose, favipiravir 1600 mg every 12 h loading dose and 600 mg maintenance dose, azithromycin 500 mg/day loading dose and 250 mg/day maintenance dose, and enoxaparin 0.5 mg/kg every 12 h. In light of the patient’s laboratory parameters and clinical condition, 400 mg tocilizumab was also given to manage the cytokine storm. The patient’s clinical symptoms improved after 24 h of treatment and follow-up is ongoing.
Figure 1.
Chest CT shows tubular and cystic bronchiectatic dilations in the bronchial structures of the upper lobe of the left lung, especially those leading to the anterior segment, and areas of ground-glass opacity and tree-in-bud appearance surrounding consolidation containing air bronchograms in the lower lobes of both lungs
Discussion
The novel coronavirus was detected in the city of Wuhan, China, at the end of 2019. Of the seven coronavirus strains known to affect humans, the betacoronaviruses are most associated with potentially severe disease. This new virus was named as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses and the associated disease was named as COVID-19 by the World Health Organization [3]. SARS-CoV-2 is closely related to SARS-CoV and MERS-CoV, which were responsible for past outbreaks that caused considerable morbidity and mortality. The rapid spread of COVID-19 caused an epidemic in China and has now become a global pandemic. At the time of writing this article, the number of confirmed COVID-19 cases worldwide will exceed 3 million.
The presenting complaints of COVID-19 usually include fever, coughing, and shortness of breath; less commonly, patients may also present to emergency departments with confusion, diarrhea, sore throat, chest pain, nausea, and vomiting. Less common presenting symptoms also include loss or attenuation of smell and taste sensation and palpitations due to myocardial wall involvement as a complication of viral respiratory tract infections [4]. Prompt initiation of antibiotics to prevent infection and support the immune system may reduce treatment complications and mortality in populations with reduced immune function, such as elderly patients, people with diabetes or HIV infection, patients on long-term immunosuppressive therapy, and pregnant women [5, 6].
Laboratory tests reveal that many patients have lymphopenia. This result suggests that SARS-CoV-2 may primarily affect lymphocytes, especially T lymphocytes, just like SARS-CoV [7]. Virus particles spread from the respiratory mucosa and infect other cells, triggering a cytokine storm. T lymphocyte damage is believed to play a major role in the development of the cytokine storm. Therefore, lymphopenia is believed to be a reference parameter that can be used in COVID-19 diagnosis. Numerous proinflammatory cytokines, mainly tumor necrosis factor-alpha, interleukin (IL)-1, IL-2, IL-6, and nitric oxide are released as a result of the cytokine storm. These cytokines increase vascular permeability and can lead to impaired tissue perfusion as well as endothelial damage and microthrombus formation. Treatment with IL-1 receptor antagonist anakinra and IL-6 antagonist tocilizumab was used in an attempt to quickly interrupt this cascade in COVID-19, and promising results were obtained [8].
As opposed to the more frequent COVID-19 symptoms, our patient presented to the emergency department with poor general condition and delirium, which are less commonly encountered. Our finding of acute renal failure in the etiology of metabolic acidosis suggested that the primary cause of this clinical picture was the cytokine storm syndrome secondary to COVID-19 rather than acute respiratory failure. In addition to the antiviral therapies used in the literature, 400 mg/day tocilizumab was administered as two doses at 24-h intervals to manage the cytokine storm. After treatment, there was improvement in the patient’s severe lymphopenia, increased glomerular filtration rate, and decreased creatine levels, which confirmed our preliminary diagnoses. In light of these findings, the patient’s acute renal failure was attributed to impaired renal perfusion secondary to cytokine storm and endothelial damage.
Acute renal failure is commonly observed in elderly patients presenting to emergency departments, generally due to infective causes and dehydration. Our aim in presenting this case is to raise awareness that COVID-19, although not as common a cause, should be included in the differential diagnosis of acute renal failure during the pandemic.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - B.K., M.A.; Design - B.K., M.A.; Supervision - N.D, M.A.; Resources - B.K., M.A.; Materials - B.K., N.D.; Data Collection and/or Processing - B.K.; Analysis and/or Interpretation - B.K., M.A.; Literature Search - N.D., M.A.; Writing Manuscript - B.K.; Critical Review - M.A., N.D.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lovato A, de Filippis C. clinical presentation of COVID-19: A systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020 doi: 10.1177/0145561320920762. 0145561320920762. [DOI] [PubMed] [Google Scholar]
- 3.Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature. 2020;5:536–44. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng JH, Liu Y-X, Yuan J, et al. First case of COVID-19 infection with fulminant myocarditis complication: Case report and insights. Infection. 2020:1–5. doi: 10.20944/preprints202003.0180.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immun. 2020 doi: 10.1016/j.jaci.2020.04.006. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus Disease 2019 (COVID-19) and Pregnancy: What obstetricians need to know. Am J Obstet Gynecol. 2020;222:415–26. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Di. 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]