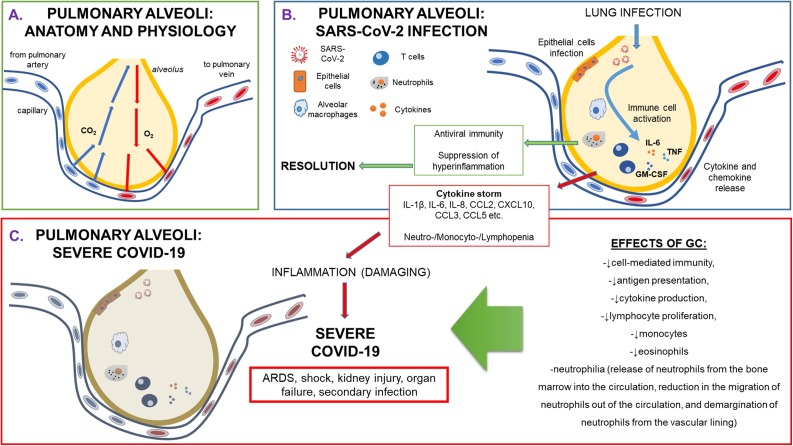
Fig. 1.
Physiology and pathophysiology of pulmonary alveoli during SARS-CoV-2 infection.
(A) Anatomy and physiology of healthy pulmonary alveoli, representing small air spaces in the lungs where carbon dioxide leaves and oxygen enters the blood. During inhalation air enters the lungs, travels through bronchi, bronchioles and then flows into approximately 300,000,000 alveoli. During exhalation, the carbon-dioxide-laden air is forced out of the alveoli through the same passageways. (B) Pathophysiology of pulmonary alveoli during SARS-CoV-2 infection. Infection of the novel Coronavirus, named SARS-CoV-2 creates an epithelial damage, followed by an immune response that is generated by a cytokine and chemokine release. This could lead to immune cell activation that might give rise to either resolution and severe COVID-19 with the consequent development of ARDS and of multi-organ failure. (C) Severe COVID-19: immune biological aspects. A sustained cytokine storm generates an inflammation that causes damage to the alveolar epithelium, giving rise to ARDS, shock, kidney injury, other organ failure and secondary infection.
Legend: ARDS: Adult Respiratory Distress Syndrome; CCL: C-C motif chemokine ligand; CXCL: C-X-C motif chemokine ligand; CO2:carbon dioxide; COVID-19: CoronaVirus Disease-19; GC: glucocorticoid; GM-CSF: granulocyte-monocyte colony stimulating factor; IL: interleukin; TNF: tumor necrosis factor.