Despite the major burden of seasonal influenza, only the threat of pandemics is of universal concern globally. Past pandemics are reviewed, identifying measures that will be of value going forward. These will also help in controlling seasonal influenza.
Keywords: influenza, influenza pandemic history, pandemic preparedness, influenza vaccines, influenza control
Abstract
Seasonal influenza is an annual occurrence, but it is the threat of pandemics that produces universal concern. Recurring reports of avian influenza viruses severely affecting humans have served as constant reminders of the potential for another pandemic. Review of features of the 1918 influenza pandemic and subsequent ones helps in identifying areas where attention in planning is critical. Key among such issues are likely risk groups and which interventions to employ. Past pandemics have repeatedly underscored, for example, the vulnerability of groups such as pregnant women and taught other lessons valuable for future preparedness. While a fundamental difficulty in planning for the next pandemic remains their unpredictability and infrequency, this uncertainty can be mitigated, in part, by optimizing the handling of the much more predictable occurrence of seasonal influenza. Improvements in antivirals and novel vaccine formulations are critical in lessening the impact of both pandemic and seasonal influenza.
Outbreaks of seasonal influenza are perennial occurrences in the temperate zones. Their impact on morbidity and mortality is highly variable but in some years can occur at levels that nearly disrupt the functioning of healthcare systems [1, 2]. During such seasonal outbreaks, questions usually center around the severity and how well the vaccine is protecting. But, regardless of disruptions, their impact is quickly forgotten.
By contrast, pandemics of influenza occur much less often but are viewed as more threatening because of their relative unfamiliarity and potential for catastrophic impact. Even a century later, much of the concern stems from recognition of the sheer number of deaths attributable to the 1918 influenza pandemic. While estimates of death have varied greatly, recent scholarship, largely based of previously omitted data from lower-income countries, such as India, has revised global estimates upwards [3] Now, the estimate of 50 million deaths is generally used as an overall global estimate, constituting nearly 3% of the world’s population at the time [4].
Pandemics are caused only by type A viruses. The current classification of A subtypes was developed in 1980 based on molecular evidence indicating that the previous nomenclature needed revision with, in addition, the inclusion of neuraminidase (NA) [5]. Table 1 shows the terminology used pre-1980 and the current terminology. Years listed are either the start of virologically confirmed pandemics or consensus dates reflecting when it was thought that a new subtype had emerged based on serology [6–9]. Influenza viruses were first isolated in the 1930s, and the etiology and timing of previous activity were based on testing of sera from individuals who had lived through the period in question. This approach, termed “seroarcheology,” resulted in occasional controversy. Most identified the 1889 influenza as caused by A2 viruses and postulated that A3 viruses had started to circulate in 1902, with no recognized pandemic occurrence. Persons who lived through the 1918 pandemic were found to have antibodies against “swine” influenza viruses, now designated as A(H1N1). The more recent reconstruction of that virus confirms the overall validity of the seroarcheologic technique [10, 11].
Table 1.
Previous and Current Influenza Type A Nomenclature for Subtypes Identified to be Circulating in Humans Since 1889
| Year of Identification | Activity | Pre-1980 Nomenclature | Current Nomenclature |
|---|---|---|---|
| 1889a | Pandemic | A2b | H2N2b |
| 1902 | Nonpandemic | A3b | H3N2b |
| 1918a | Pandemic | Asw (Swine)b | H1N1 |
| 1929 | Nonpandemic | A (A0) | H1N1 |
| 1947 | Nonpandemic | A′ (A prime) | H1N1 |
| 1957a | Pandemic | A2 (Asian) | H2N2 |
| 1968a | Pandemic | A3 (Hong Kong) | H3N2 |
| 1976 | Nonpandemic | Asw (Swine) | H1N1 |
| 1977 | Pseudo-pandemic | A1 (Russian) | H1N1 |
| 2009a | Pandemic | … | H1N1pdm09 |
aConfirmed pandemic.
bThese strains were identified by serology, but the specific identification is in dispute. Some have the 1889 virus as H3N8 but without a different subtype identified starting in 1902, a year when there was not a clear pandemic [6–9].
SOME IMPLICATIONS OF THE 1918 PANDEMIC
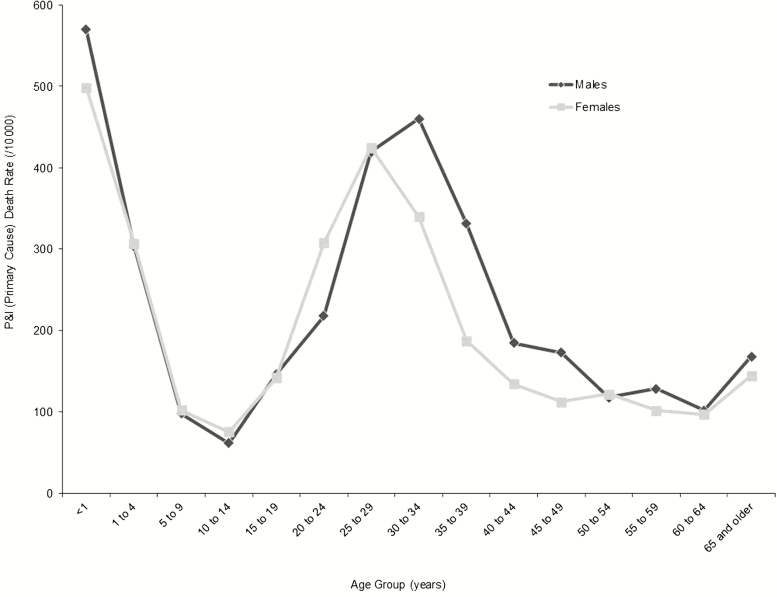
The most remarkable epidemiological feature of the 1918 pandemic was the unexpectedly high mortality among those aged 20–39 years [3]. Theories to explain this pattern abound but most involve an aberrant immune response [12]. One recent hypothesis postulates that prior infection of children in the 1889 pandemic rendered them particularly susceptible by immunologic imprinting to reinfection in 1918 when they were in their late 20s [13]. Current evidence suggests that older individuals may have actually been protected in 1918. This is in contrast to the traditional belief in the W-shaped epidemic curve, in which the high mortality in the elderly was a result of the erroneous inclusion of seasonal disease from the early months of 1918 [14]. Figure 1 shows the age-specific mortality in Philadelphia where the pandemic shut down the city and peaked at a weekly annualized rate of 140 deaths per 1000 population [3, 15, 16]. Another often overlooked but constant feature of all pandemics is the high mortality in the very young experiencing their first influenza infection [14]. These observations indicate that understanding the positive and negative effect of prior influenza exposure is critical [17].
Figure 1.
Sex- and age-specific annualized mortality rates for influenza and pneumonia (P&I) (primary cause) Philadelphia, Pennsylvania, October–December 1918 [15].
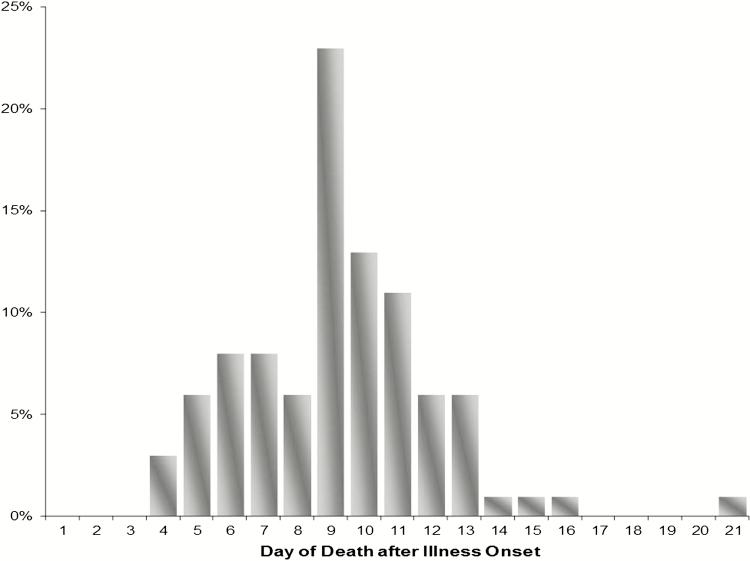
Other observations of relevance to planning efforts are indications of the usefulness of nonpharmaceutical interventions in mitigating community impact [18]. The susceptibility of pregnant women was well documented; it should not have been such a surprise during the 2009 influenza pandemic when it was rediscovered [3]. Sudden death has often been emphasized as a feature of 1918, but it took, on average, 9 or more days for death to occur [19] (Figure 2). This stresses the need for health systems to have the surge capacity necessary to handle patients with the more typical prolonged illness regardless of the severity of a pandemic. A proportion of the deaths were associated with bacterial complications. The global increase in antibiotic-resistant organisms is another major vulnerability [20].
Figure 2.
Distribution of day of death from influenza by day of disease as recorded at 2 US army general hospitals from the beginning of the pandemic until mid-December, 1918 [19].
AN INTERVAL OF NEARLY 40 YEARS AND THE PANDEMIC OF 1957
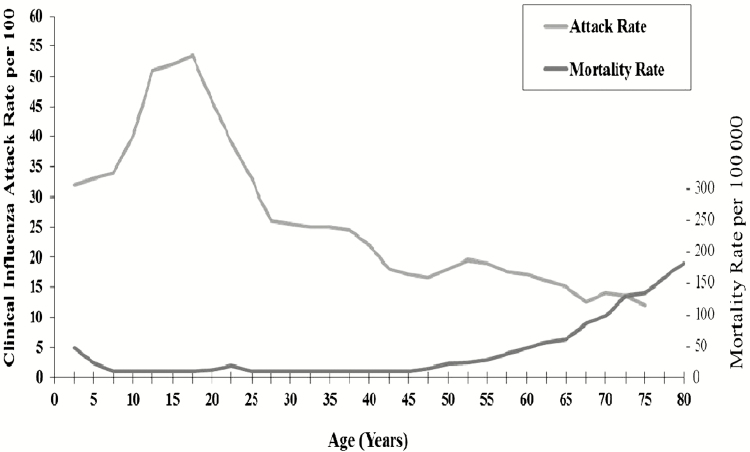
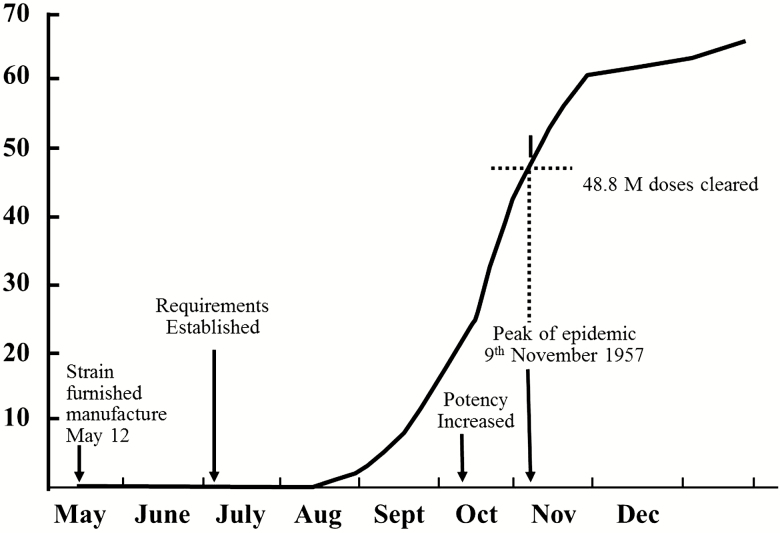
Most pre-1980 lists of influenza pandemics included one in 1947 despite lack of documentation of global outbreaks (Table 1). In that year, seasonal vaccine became ineffective and it was thought that a new subtype named “A prime” had emerged [21, 22]. This understanding was important in developing the doctrine of original antigenic sin. It is now understood that an intrasubtypic reassortment occurred in 1947, which resulted in a major antigenic change of the A(H1N1) viruses [23]. A new subtype, A(H2N2), actually emerged in 1957 when 3 gene segments coding for hemagglutinin (HA), NA, and an internal component moved from an avian virus into the circulating A(H1N1) virus through genetic reassortment [24, 25]. The resulting A(H2N2) virus, which was called “Asian influenza” since it emerged from China, totally replaced the A(H1N1) viruses. Since this was the first true pandemic since 1918, there was immediate concern about its potential impact and great relief when it was found to resemble seasonal influenza with morbidity highest in children and mortality at the extremes of age [26, 27] (Figure 3). In the United States, the virus emerged in the spring of 1957, but outbreaks intensified only after schools in the southern United States opened in August, underscoring the importance of children in dissemination [28]. Although vaccine was available in the United States late in the first wave, it had to be reformulated because of subpotency and standardization issues, concerns still being addressed [29] (Figure 4). With little vaccine available, attention was paid to other ways to reduce transmission. A controlled experiment conducted at the Veterans Administration hospital in Livermore, California, demonstrated reduced transmission from the use of ultraviolet lights [30]. That tantalizing observation has been used recently to strengthen the suggestion that small-particle aerosol transmission of influenza viruses is of importance.
Figure 3.
Incidence of influenza-like illness by age among 1355 families, Kansas City, Missouri, July–October 1957, and pneumonia and influenza mortality by age, United States, 1957. Data from references [26] and [27].
Figure 4.
Asian (H2N2) influenza vaccine cleared for release in the United States (millions of milliliters). Data from reference [29].
OBSERVATIONS FROM THE 1968 PANDEMIC
The A(H2N2) period lasted only 11 years until mid-1968. In July of that year, a major outbreak in Hong Kong signaled that another reassortment event had occurred [31]. Avian influenza genes, one coding for HA and the other an internal component, replaced the existing counterparts in the circulating A(H2N2) virus; the NA gene was not replaced [24, 25]. Emergence of A(H2N2) and A(H3N2) viruses and later events led to the concept that “novel” influenza viruses are most likely to come from East Asia. At the time, it was conjectured that reassortment (or “shift”) of avian and human influenza viruses occurred in a nonhuman “mixing vessel” because humans were believed not to have the right cellular entry receptors for avian influenza viruses. Pigs have receptors for both human and avian influenza viruses, and since influenza viruses replicate in these animals they were considered to be the mixing vessel [32]. This was further supported by the observation that humans, poultry, pigs, and wild birds live in close proximity in East Asia, providing ample opportunity for reassortment to occur there.
The A(H3N2) pandemic exhibited the same patterns of morbidity and mortality as the earlier A(H2N2) pandemic. In terms of reasons for emergence of a pandemic variant after only 11 years, it is of interest that the last outbreak of A(H2N2) in 1967–1968 was extensive, as measured by pneumonia and influenza (P and I) mortality. This indicates that a considerable percentage of the population still remained susceptible to A(H2N2) [33, 34]. However, the new A(H3N2) virus completely replaced the previous subtype, and its variants, more than 50 years later, have been responsible for the greatest proportion of mortality from influenza viruses.
The first A(H3N2) pandemic wave occurred in the United States in midwinter 1968–1969 at a time typical of seasonal influenza but which in some parts of the world was delayed. There has been speculation that the delay was a result of protection from the unchanged NA. Even in the United States, contemporaneous studies showed reduction in infection in those with higher anti-NA titers, indicating an independent protective effect beyond anti-HA [35]. The role of anti-NA remains an issue in present-day efforts to improve vaccine [36].
THE SWINE INFLUENZA AFFAIR OF 1976 AND THE RETURN OF A(H1N1) IN 1977
In January 1976, an outbreak of severe influenza occurred at the US military’s Fort Dix, New Jersey. The causative virus was surprisingly found to be a variant of swine influenza, now recognized to be an A(H1N1) virus [37]. Since previous serologic studies had shown that the 1918 pandemic was probably caused by swine influenza (Table 1), there was strong concern that the Fort Dix outbreak could herald another severe pandemic [38]. In the United States, vaccine production was begun after liability concerns of the manufacturers had been addressed. Even though no further human outbreaks were detected, mass vaccinations were begun and stopped only when a relationship between the vaccine and Guillain-Barré was identified. This “affair” has been studied extensively in terms of potential pitfalls in pandemic response and decision making [39].
In the following year, a different A(H1N1) virus, one that had been circulating before 1957, was identified [40]. Transmission of this virus, termed “Russian influenza” since the reports first came from the far east of the Soviet Union, was unexpected because the virus had not been detected for 20 years. Infections were widespread, generally mild, and limited to younger individuals; residual protection was nearly complete in older individuals [41]. This event has never been considered a true pandemic because so much of the world’s population was not susceptible and because of the uncertain origin of the virus. The re-emerged A(H1N1) virus remained in persistent circulation worldwide along with A(H3N2) viruses and continued to evolve until it disappeared in 2009. Before this, when a new A subtype began circulating, it completely replaced the previous one.
THE CONTINUING PANDEMIC THREATS OF AVIAN INFLUENZA BEGIN
The concept that avian influenza viruses could not directly infect humans ended in 1997 when avian A(H5N1) viruses spread directly from poultry to humans, causing a small but highly important outbreak in Hong Kong. This event, which raised global concern, resulted in the deaths of 6 of 18 patients with documented infection [42, 43]. Once control measures, especially culling of poultry, were put into place, new cases abruptly stopped. No further human cases were detected until, in 2003, when, in conjunction with die-offs of poultry, the spread of A(H5N1) to humans occurred, mainly in Southeast Asia [44–46]. Most human infections were the result of contact with poultry, but examples of limited human-to-human transmission were documented [47]. Because human cases were often severe and resulted in respiratory failure and death, there was high global concern that a pandemic of this virus would be severe if sustained human-to-human transmission occurred [48]. The nature of the threat, arising in animals but directly of concern to humans, highlighted the generally poor coordination and often rigid separation between animal and human health authorities at national and international levels, as well as a general lack of national planning. The adoption of new International Health Regulations in 2005, which was strongly influenced by the emergence of SARS (severe acute respiratory syndrome) and the re-emergence of A(H5N1) in 2003, constituted a major step forward [49]. In the United States, there was particular attention directed to nonpharmaceutical interventions, a result of the recognition that pandemic-specific vaccines would be available relatively late and that influenza-specific antiviral drugs, while important, would be limited in quantity. There were discussions as to whether the use of antivirals might be able to contain human transmission of an emerging virus at the source; these plans were mainly predicated on the emergence occurring in Asia [50, 51].
THE 2009 A(H1N1) PANDEMIC
Continuing concern about outbreaks of avian influenza was interrupted when the first pandemic of the 21st century unexpectedly started in Mexico in 2009 [52]. As a result of intrasubtypic reassortment, the A(H1N1) variant involved was antigenically highly distinct from previously circulating influenza A(H1N1) viruses [53]. The previous prevailing dogma was that pandemic influenza was the result of the emergence of a new virus subtype. However, the subsequent global spread indicates that a pandemic is better defined by the global population’s immunological susceptibility and antigenic distance of the new virus from other influenza viruses, rather than rigid applications of virologic rules involving antigenic shift [54].
The 2009 A(H1N1) virus was associated with lower attack rates in older individuals, presumably because of prior exposure to older A(H1N1) viruses. Its spread in North America in the spring extended quickly to other parts of the world, highlighting the importance of air travel in accelerating dissemination. In the United States, the spring wave slowed with the beginning of school summer vacations only to pick up again as schools opened in the autumn, reconfirming the importance of children in transmission.
This most recent pandemic has been extensively documented. Severe disease developed in a small proportion of healthy adults, many of whom had no underlying conditions, which was reminiscent of 1918 but at a much smaller scale [55]. Particularly vulnerable groups included indigenous populations, well-documented in Canada in the first spring wave [56]. This was not observed in the second wave, most likely related to modifications in response, including careful employment of antivirals. The association of severity with pregnancy was another clear reminder of the 1918 pandemic. A newly observed risk was morbid obesity [57]. The new pandemic virus completely replaced the prior circulating seasonal A(H1N1) but cocirculation of the influenza A(H3N2) virus continued.
A societal issue of considerable importance, which is essential to address for future pandemics as well as for seasonal influenza planning efforts, was the perception promoted by some that the 2009 pandemic was a “fake” pandemic [58, 59]. The claim, amplified by social media, was that the public health response was a conspiracy by governments and the World Health Organization (WHO) to benefit the sale of influenza vaccines. The overall pattern of mortality, which was less extensive than in 20th-century pandemics, was an important component [55]. But perhaps the more fundamental observation is that the accusations were consistent with a broader erosion of trust within society. The need to focus on communications and trust building in all phases of a pandemic is an essential lesson for improving planning for pandemics and responding to seasonal influenza.
GENERAL OBSERVATIONS FROM PAST PANDEMICS
During the past 100 years since 1918, each of the 4 influenza pandemics has presented both common and unique challenges. None has been predictable in terms of timing, location of onset ,or the causative influenza virus. Those that started in 1957 and 1968 had the most similar morbidity and mortality patterns, with severe complications and deaths that were highest at the extremes of age. The practical consequences for planning are the need to direct interventions to cover such groups while recognizing that other groups may also be at a higher than usual risk [60]. The age groups most at risk may be the same as in seasonal influenza but may not.
Questions about “severity” are to be expected early, but determining such levels is particularly challenging. The impact on morbidity and mortality may differ, and perception of severity may also differ widely depending on place and time. During the start of events, the information available to health authorities is often limited and highly uncertain. Nonetheless, severity assessments are likely to be important for justifying the use of nonpharmaceutical interventions, such as closing schools and restricting population movement. Such actions, which apparently had an effect in 1918, are socially disruptive and likely to be divisive. Reducing impact may benefit from using more resources early while communicating the uncertainties involved and the consequences of inaction.
Since 1957, vaccine has always been available late, often after the first wave. In 2009, the current system of virus sharing through frameworks already established at WHO worked well but vaccine was still not available widely nor equitably. New technologies, such as a universal vaccine, may eventually change this situation but not in the near term. The prepandemic use of vaccines containing known potential pandemic viruses, often with adjuvants, has been proposed, but there are significant uncertainties in choosing what viruses might go into such a vaccine or for taking the inherent risks [61, 62].
FUTURE APPROACHES TO MITIGATE INFLUENZA IMPACT
Preparing for, and responding to, a pandemic is a complex phenomenon, combining science, societal beliefs, practical operational considerations, and political will. Some countries and regions have continued to update plans, but others have not. This is a reflection, in part, of uncertainties following the 2009 pandemic but also what has been termed “pandemic fatigue.” The latter issue has been made worse by the repeated recognition of the pandemic potential of different avian influenza virus variants that have infected humans [63–65].
Given this context, it is important to recognize that seasonal influenza occurs every year and many of the essential control measures for pandemics are based on those used for seasonal influenza. It is critical to avoid viewing pandemic and seasonal influenza as unrelated. Seasonal influenza is a cause of significant morbidity and mortality, and the vaccine supply used for seasonal influenza sets, in a real-world sense, the production capacity for a pandemic. Some countries that will want access to pandemic vaccine do not consider seasonal influenza as a priority. This will limit their capacities to vaccinate their most vulnerable subpopulations in a pandemic, even if vaccine is available. This situation is especially true of lower-resource countries, and continued efforts to document the impact of seasonal influenza and, concomitantly, to develop the health system capabilities needed to support a pandemic response remain high priorities. Determining the possible reduction in seasonal severe disease from the use of vaccine can be evaluated in a vaccine probe study in which the vaccine is given under controlled conditions to young children in underresourced areas, similar to studies that documented the need for pneumococcal vaccine [66]. The need for all countries to have and use vaccine in a pandemic is an issue of the equitable distribution of resources on both a national and global scale. Scientific advances have positioned the world to respond better to both seasonal and pandemic threats of influenza. However, to make the most of such advances before the next pandemic will still require consistent attention and both scientific and political leadership.
Note
Potential conflicts of interest. A. S. M. reports consulting fees from Sanofi, Seqirus, and Roche, outside the submitted work. K. F. has no potential conflicts to disclose. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Note
References
- 1. Paules CI, Sullivan SG, Subbarao K, Fauci AS. Chasing seasonal influenza—the need for a universal influenza vaccine. N Engl J Med 2018; 378:7–9. [DOI] [PubMed] [Google Scholar]
- 2. Garten R, Blanton L, Elal AIA, et al. . Update: influenza activity in the United States during the 2017-18 season and composition of the 2018-19 influenza vaccine. MMWR Morb Mortal Wkly Rep 2018; 67:634–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jordan E. Epidemic influenza: a survey. Chicago: American Medical Association, 1927. [Google Scholar]
- 4. Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull Hist Med 2002; 76:105–15. [DOI] [PubMed] [Google Scholar]
- 5. A revision of the system of nomenclature for influenza viruses: a WHO memorandum. Bull World Health Organ 1980; 58:585–91. [PMC free article] [PubMed] [Google Scholar]
- 6. Davenport FM. Influenza viruses. In: Evans AS, ed. Viral infections of humans: epidemiology and control. New York: Plenum, 1984:373–96. [Google Scholar]
- 7. Mulder J, Masurel N. Pre-epidemic antibody against 1957 strain of Asiatic influenza in serum of older people living in the Netherlands. Lancet 1958; 1:810–4. [DOI] [PubMed] [Google Scholar]
- 8. Marine WM, Workman WM, Webster RG. Immunological interrelationships of Hong Kong, Asian and equi-2 influenza viruses in man. Bull World Health Organ 1969; 41:475–82. [PMC free article] [PubMed] [Google Scholar]
- 9. Masurel N, Marine WM. Recycling of Asian and Hong Kong influenza A virus hemagglutinins in man. Am J Epidemiol 1973; 97:44–9. [DOI] [PubMed] [Google Scholar]
- 10. Taubenberger JK, Reid AH, Krafft AE, Bijwaard KE, Fanning TG. Initial genetic characterization of the 1918 “Spanish” influenza virus. Science 1997; 275:1793–6. [DOI] [PubMed] [Google Scholar]
- 11. Tumpey TM, Basler CF, Aguilar PV, et al. . Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 2005; 310:77–80. [DOI] [PubMed] [Google Scholar]
- 12. Kobasa D, Jones SM, Shinya K, et al. . Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature 2007; 445:319–23. [DOI] [PubMed] [Google Scholar]
- 13. Worobey M, Han GZ, Rambaut A. Genesis and pathogenesis of the 1918 pandemic H1N1 influenza A virus. Proc Natl Acad Sci USA 2014; 111:8107–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nguyen-Van-Tam JS, Hampson AW. The epidemiology and clinical impact of pandemic influenza. Vaccine 2003; 21:1762–8. [DOI] [PubMed] [Google Scholar]
- 15. US Bureau of the Census. Special tables for mortality from influenza and pneumonia, September 1 to December 31, 1918. Washington: US Government Printing Office, 1920. [Google Scholar]
- 16. Starr I. Influenza in 1918: recollections of the epidemic in Philadelphia. Ann Intern Med 1976; 85:516–8. [DOI] [PubMed] [Google Scholar]
- 17. Petrie JG, Parkhouse K, Ohmit SE, Malosh RE, Monto AS, Hensley SE. Antibodies against the current influenza A(H1N1) vaccine strain do not protect some individuals from infection with contemporary circulating influenza A(H1N1) virus strains. J Infect Dis 2016; 214:1947–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Markel H, Stern AM, Navarro JA, Michalsen JR, Monto AS, DiGiovanni C. Nonpharmaceutical influenza mitigation strategies, US communities, 1918-1920 pandemic. Emerg Infect Dis 2006; 12:1961–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roberts D. The unidentified pandemic disease. Am J Med Sci 1919; 158:397–406. [Google Scholar]
- 20. Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis 2007; 195:1018–28. [DOI] [PubMed] [Google Scholar]
- 21. Kilbourne ED, Loge JP. Influenza A prime: a clinical study of an epidemic caused by a new strain of virus. Ann Intern Med 1950; 33:371–9. [DOI] [PubMed] [Google Scholar]
- 22. Kilbourne ED, Smith C, Brett I, Pokorny BA, Johansson B, Cox N. The total influenza vaccine failure of 1947 revisited: major intrasubtypic antigenic change can explain failure of vaccine in a post-World War II epidemic. Proc Natl Acad Sci USA 2002; 99:10748–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nelson MI, Viboud C, Simonsen L, et al. . Multiple reassortment events in the evolutionary history of H1N1 influenza A virus since 1918. PLoS Pathog 2008; 4:e1000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Scholtissek C, Rohde W, Von Hoyningen V, Rott R. On the origin of the human influenza virus subtypes H2N2 and H3N2. Virology 1978; 87:13–20. [DOI] [PubMed] [Google Scholar]
- 25. Kawaoka Y, Krauss S, Webster RG. Avian-to-human transmission of the PB1 gene of influenza A viruses in the 1957 and 1968 pandemics. J Virol 1989; 63:4603–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chin TD, Foley JF, Doto IL, Gravelle CR, Weston J. Morbidity and mortality characteristics of Asian strain influenza. Public Health Rep 1960; 75:149–58. [PMC free article] [PubMed] [Google Scholar]
- 27. Dauer CC, Serfling RE. Mortality from influenza 1957–1958 and 1959–1960. Am Rev Respir Dis 1961; 83:15–28. [Google Scholar]
- 28. Langmuir AD. Epidemiology of Asian influenza: with special emphasis on the United States. Am Rev Respir Dis 1961; 83(2)Pt 2:2–14. [DOI] [PubMed] [Google Scholar]
- 29. Murray R. Some problems in the standardization and control of influenza vaccine in 1957. Am Rev Respir Dis 1961; 83:160–7. [DOI] [PubMed] [Google Scholar]
- 30. Jordan WS., Jr The mechanism of spread of Asian influenza. Am Rev Respir Dis 1961; 83(2)Pt 2:29–40. [DOI] [PubMed] [Google Scholar]
- 31. Cockburn WC, Delon PJ, Ferreira W. Origin and progress of the 1968-69 Hong Kong influenza epidemic. Bull World Health Organ 1969; 41:345–8. [PMC free article] [PubMed] [Google Scholar]
- 32. Scholtissek C. Pigs as “mixing vessels” for the creation of new pandemic influenza A viruses. Med Princ Pract 1990; 2:65–71. [Google Scholar]
- 33. Housworth WJ, Spoon MM. The age distribution of excess mortality during A2 Hong Kong influenza epidemics compared with earlier A2 outbreaks. Am J Epidemiol 1971; 94:348–50. [DOI] [PubMed] [Google Scholar]
- 34. Sharrar RG. National influenza experience in the USA, 1968-69. Bull World Health Organ 1969; 41:361–6. [PMC free article] [PubMed] [Google Scholar]
- 35. Monto AS, Kendal AP. Effect of neuraminidase antibody on Hong Kong influenza. Lancet 1973; 1:623–5. [DOI] [PubMed] [Google Scholar]
- 36. Krammer F, Fouchier RAM. Eichelberger MC, et al. . NAction! How can neuraminidase-based immunity contribute to better influenza virus vaccines? Mbio 2018; 9:e02332-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Top FH Jr, Russell PK. Swine influenza A at Fort Dix, New Jersey (January-February 1976). IV. Summary and speculation. J Infect Dis 1977; 136 Suppl:S376–80. [DOI] [PubMed] [Google Scholar]
- 38. Dowdle WR. Influenza A virus recycling revisited. Bull World Health Organ 1999; 77:820–8. [PMC free article] [PubMed] [Google Scholar]
- 39. Neustadt RE, Fineberg HV.. The Swine flu affair: decision-making on a slippery disease. Washington: US Government Printing Office, 1978. [PubMed] [Google Scholar]
- 40. Gregg MB, Hinman AR, Craven RB. The Russian flu: its history and implications for this year’s influenza season. JAMA 1978; 240:2260–3. [DOI] [PubMed] [Google Scholar]
- 41. Monto AS, Koopman JS, Longini IM Jr. Tecumseh Study of Illness. XIII. Influenza infection and disease, 1976-1981. Am J Epidemiol 1985; 121:811–22. [DOI] [PubMed] [Google Scholar]
- 42. Subbarao K, Klimov A, Katz J, et al. . Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 1998; 279:393–6. [DOI] [PubMed] [Google Scholar]
- 43. Bridges CB, Lim W, Hu-Primmer J, et al. . Risk of influenza A (H5N1) infection among poultry workers, Hong Kong, 1997-1998. J Infect Dis 2002; 185:1005–10. [DOI] [PubMed] [Google Scholar]
- 44. Peiris JS, Yu WC, Leung CW, et al. . Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 2004; 363:617–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li KS, Guan Y, Wang J, et al. . Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature 2004; 430:209–13. [DOI] [PubMed] [Google Scholar]
- 46. Tran TH, Nguyen TL, Nguyen TD, et al. ; World Health Organization International Avian Influenza Investigative Team Avian influenza A (H5N1) in 10 patients in Vietnam. N Engl J Med 2004; 350:1179–88. [DOI] [PubMed] [Google Scholar]
- 47. Wang H, Feng Z, Shu Y, et al. . Probable limited person-to-person transmission of highly pathogenic avian influenza A (H5N1) virus in China. Lancet 2008; 371:1427–34. [DOI] [PubMed] [Google Scholar]
- 48. Monto AS. The threat of an avian influenza pandemic. N Engl J Med 2005; 352:323–5. [DOI] [PubMed] [Google Scholar]
- 49. World Health Organization. International Health Regulations [serial on the Internet]. 2005. 24 January 2013. Available at: https://www.who.int/ihr.en. Accessed 16 January 2019. [Google Scholar]
- 50. Ferguson NM, Cummings DA, Cauchemez S, et al. . Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 2005; 437:209–14. [DOI] [PubMed] [Google Scholar]
- 51. Longini IM Jr, Nizam A, Xu S, et al. . Containing pandemic influenza at the source. Science 2005; 309:1083–7. [DOI] [PubMed] [Google Scholar]
- 52. Domínguez-Cherit G, Lapinsky SE, Macias AE, et al. . Critically ill patients with 2009 influenza A(H1N1) in Mexico. JAMA 2009; 302:1880–7. [DOI] [PubMed] [Google Scholar]
- 53. Garten RJ, Davis CT, Russell CA, et al. . Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 2009; 325:197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Morens DM, Folkers GK, Fauci AS. What is a pandemic? J Infect Dis 2009; 200:1018–21. [DOI] [PubMed] [Google Scholar]
- 55. Viboud C, Miller M, Olson D, Osterholm M, Simonsen L. Preliminary estimates of mortality and years of life lost associated with the 2009 A/H1N1 pandemic in the US and comparison with past influenza seasons. PLoS Curr 2010; 2:RRN1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kumar A, Zarychanski R, Pinto R, et al. ; Canadian Critical Care Trials Group H1N1 Collaborative Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA 2009; 302:1872–9. [DOI] [PubMed] [Google Scholar]
- 57. Van Kerkhove MD, Vandemaele KA, Shinde V, et al. ; WHO Working Group for Risk Factors for Severe H1N1pdm Infection Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med 2011; 8:e1001053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Report of the Review Committee on the Functioning of the International Health Regulations (2005) in relation to Pandemic (H1N1) 2009. 2011. (Fineberg Report). Available at: https://apps.who.int/gb/ebwha.pdf_files/WHA64/A64_10-en.pdf. Accessed 16 January 2019. [Google Scholar]
- 59. Monto AS, Black S, Plotkin SA, Orenstein WA. Response to the 2009 pandemic: effect on influenza control in wealthy and poor countries. Vaccine 2011; 29:6427–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Reed C, Biggerstaff M, Finelli L, et al. . Novel framework for assessing epidemiologic effects of influenza epidemics and pandemics. Emerg Infect Dis 2013; 19:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Goodman JL. Investing in immunity: prepandemic immunization to combat future influenza pandemics. Clin Infect Dis 2016; 62:495–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Erbelding EJ, Post DJ, Stemmy EJ, et al. . A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases. J Infect Dis 2018; 218:347–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Peiris M, Yuen KY, Leung CW, et al. . Human infection with influenza H9N2. Lancet 1999; 354:916–7. [DOI] [PubMed] [Google Scholar]
- 64. Gao R, Cao B, Hu Y, et al. . Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 2013; 368:1888–97. [DOI] [PubMed] [Google Scholar]
- 65. Wang G, Deng G, Shi J, et al. . H6 influenza viruses pose a potential threat to human health. J Virol 2014; 88:3953–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gessner BD, Brooks WA, Neuzil KM, et al. . Vaccines as a tool to estimate the burden of severe influenza in children of low-resourced areas (November 30-December 1, 2012, Les Pensieres, Veyrier-du-Lac, France). Vaccine 2013; 31:3222–8. [DOI] [PubMed] [Google Scholar]