Supplemental Digital Content is available in the text.
Abstract
Objectives:
The outbreak of coronavirus disease 2019 is becoming a worldwide pandemic. Mechanical ventilation is lifesaving for respiratory distress, this study was designed to delineate the clinical features of the coronavirus disease 2019 patients with mechanical ventilation from a national cohort in China.
Design:
Prospective observational study.
Setting:
The rapid spread of severe acute respiratory syndrome coronavirus 2 has infected more than 7.7 million people and caused more than 423,000 deaths.
Patients:
Adult hospitalized coronavirus disease 2019 patients with mechanical ventilation from 557 hospitals from China.
Interventions:
None.
Measurements and Main Results:
From a nationwide cohort, 141 coronavirus disease 2019 cases with mechanical ventilation were extracted from 1,590 cases. Cigarette smoke, advanced age, coexisting chronic illness, elevated systolic blood pressure, high body temperature, and abnormal laboratory findings are common in these ventilated cases. Multivariate regression analysis showed that higher odds of in-hospital death was associated with invasive mechanical ventilation requirement (hazard ratio: 2.95; 95% CI, 1.40–6.23; p = 0.005), and coexisting chronic obstructive pulmonary disease (hazard ratio, 4.57; 95% CI, 1.65–12.69; p = 0.004) and chronic renal disease (hazard ratio, 5.45; 95% CI, 1.85–16.12; p = 0.002). Compared with patients with noninvasive mechanical ventilation, patients who needs invasive mechanical ventilation showed higher rate of elevated d-dimer (> 1.5 mg/L) at admission (hazard ratio, 3.28, 95% CI, 1.07–10.10; p = 0.039).
Conclusions:
The potential risk factors of elevated d-dimer level could help clinicians to identify invasive mechanical ventilation requirement at an early stage, and coexisting chronic obstructive pulmonary disease or chronic renal disease are independent risk factors associated with fatal outcome in coronavirus disease 2019 patients with mechanical ventilation.
Outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is becoming a worldwide pandemic, the rapid spread of the virus has caused more than 7.7 million coronavirus disease 2019 (COVID-19) cases and more than 423,000 deaths globally (1–3). COVID-19 patients exhibit a spectrum of respiratory symptoms like cough and dyspnea, and some patients may develop hypoxemia (4). Most of the hypoxemic patients could be managed by oxygen therapy. However, there are some critically ill patients who require mechanical ventilation (MV) (5, 6). Here, by collecting a nationwide data through China, we sought to provide a delineation of the clinical features of COVID-19 patients with MV.
MATERIAL AND METHODS
On behalf of the National Clinical Research Center for Respiratory Disease, together with the National Health Commission of the People’s Republic of China, we performed a retrospective study to collect clinical information of COVID-19 cases throughout the country. The study was supported by National Health Commission and designed by the investigators, and approved by the institutional board of National Health Commission. Written informed consent was waived in light of the urgent need to collect data. By January 31, 2020, a cohort of 2007 hospitalized cases from 575 hospitals in China was established (7, 8). Medical history, epidemiological, and laboratory data were obtained. Four hundred and seventeen cases were excluded because of insufficient medical records. Data were analyzed and interpreted by the investigators. Continuous variables were expressed as medians and interquartile ranges (IQR). Wilcoxon rank-sum tests were applied to continuous variables, and chi-square tests or Fisher exact test were applied to categorical variables as appropriate. To estimate the hazard ratio (HR) associated with mortality or the requirement of invasive MV (IMV), variables including baseline characteristics, laboratory findings were analyzed by univariate Cox regression analyses, significant variables were further included in multivariate Cox regression analyses. The adjusted Kaplan-Meier survivor curve was used to estimate time-dependent hazards categorized by risk factors.
RESULTS
Among the 1,590 cases included in this study, 141 (8.9%) received MV, 122 received noninvasive mechanical ventilation (NIV), and 50 received IMV through trachea intubation. There were 31 cases (62% of total IMV) who received NIV before transition to IMV, these patients were grouped in IMV group for further analysis. Thus, there were 91 and 50 cases in NIV and IMV group, respectively.
Of the 141 ventilated COVID-19 cases included in this study, the median age was 64 years (IQR, 55–70 yr) , 70% were men and 70% were smokers. There were 89 (63%) cases with one or more coexisting medical conditions, the most common coexisting conditions were hypertension (45%), diabetes (26%), cerebrovascular disease (9.2%), and coronary artery disease (8.5%). The duration from admission to NIV and IMV were 3 days (1.0–8.0 d) and 5 days (1.8–10.0 d), respectively. The physical signs were shown in Table E1 (Supplemental Digital Content 1, http://links.lww.com/CCM/F609), the most common abnormal signs of these ventilated cases at admission were elevated respiratory rate (>20/min, 57%), elevated systolic blood pressure (≥ 140 mmHg, 30%), and high body temperature (>37.3°C, 36.2%). As shown in Table E2 (Supplemental Digital Content 1, http://links.lww.com/CCM/F609), among the patients who underwent laboratory tests at admission, most patients showed lymphocytopenia (87%), elevated level of C-reactive protein (CRP) (82%), lactate dehydrogenase (88%), aspartate aminotransferase (62%), and d-dimer (53%). Multivariate regression indicated that higher odds of in hospital death was associated with IMV requirement (hazards ratio [HR], 2.95; 95% CI, 1.40–6.23; p = 0.005), and coexisting chronic obstructive pulmonary disease (COPD) (HR, 4.57, 95% CI, 1.65–12.69; p = 0.004) and chronic renal disease (HR, 5.45; 95% CI, 1.85–16.12; p = 0.002) (Fig. 1A). The adjusted survivor curve showed time-dependent hazards of these factors (Fig. 1B–E).
Figure 1.
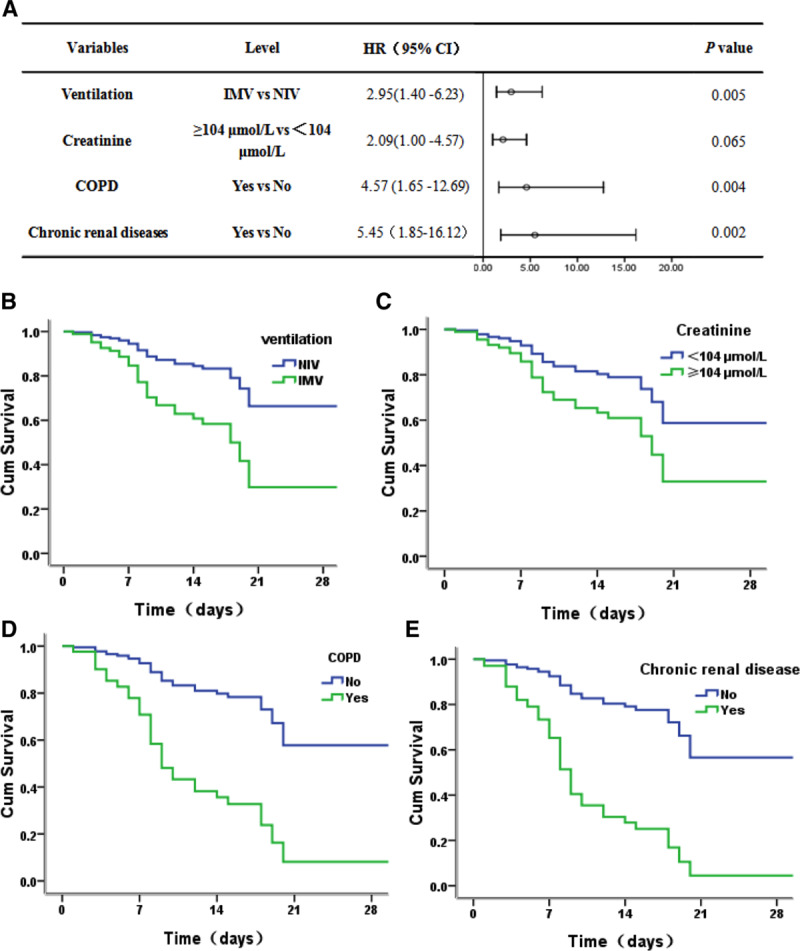
Risk factor of the fatal outcome in the proportional hazards model. A, The hazards ratio (HR) and the 95% CI associated with the endpoint. B–E, The adjusted survival curves for time dependent hazards of different variables by multivariate Cox regression. COPD = chronic obstructive pulmonary disease, cum = cumulative, HR = hazard ratio, IMV = invasive mechanic ventilation, NIV = noninvasive mechanical ventilation.
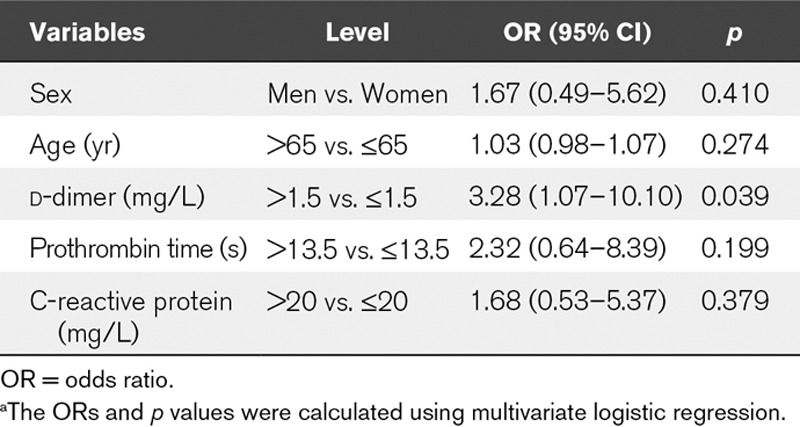
Compared with NIV group, IMV cases had higher levels of lactate dehydrogenase, d-dimer, CRP and WBC count, and lower levels of albumin and oxygenation index (Table E2, Supplemental Digital Content 1, http://links.lww.com/CCM/F609); and showed a higher incidence of elevated d-dimer at admission with multivariate logistic regression analysis (>1.5 mg/L; HR, 3.05; 95% CI, 1.07–8.69, p = 0.037) (Table 1). The secondary infection rate in the IMV group (14/50, 28%) was higher than NIV group (15/91, 16.5%), though not statistically different (p = 0.106). And there was no statistical significance in any of the coexisting chronic conditions between NIV and IMV group. By the time of data collection, 19 (17%) and 25 (50%) cases died in NIV and IMV group, respectively, 4 (4.4%) and 0 (0%) patients recovered and discharged from hospital in NIV and IMV group, respectively (p < 0.01); the remaining cases were still under treatment in the hospital, and IMV were successfully removed in two cases.
TABLE 1.
Variables Associated With Invasive Mechanic Ventilation Requirement in Ventilated Coronavirus Disease 2019 Patientsa
In the Diagnosis and Treatment Protocol for COVID-19 (Trial Version 7) released by National Health Commission & State Administration of Traditional Chinese Medicine in China: NIV is recommended to COVID-19 patients with respiratory distress and/or hypoxemia, which cannot be alleviated with standard or high-flow nasal cannula oxygen therapy; whereas IMV is recommended to be applied in a timely manner if the oxygen saturation or respiratory distress do not improve or even get worse within 1–2 hours after NIV. Among the 122 cases who initially received NIV in our study, 31 progressed to IMV, and these cases demonstrated higher level of CRP (p = 0.016), and no significant difference of the other laboratory findings at admission compared with those remained with NIV (Table E3, Supplemental Digital Content 1, http://links.lww.com/CCM/F609).
DISCUSSION
In this study, we reported critically ill COVID-19 cases who required MV from a nationwide cohort for the first time. Consistent with the severe COVID-19 cases in previous reports (6, 9), patients in our cohort are aged population with a high rate of comorbidities including cardiovascular diseases and diabetes. And patients with coexisting COPD or chronic renal disease is associated with higher mortality risk, which may suggest that intensive surveillance should be considered in case of rapid deterioration in COVID-19 patients with these chronic conditions.
MV is the cornerstone in the management of respiratory failure via aiding patients to get adequate oxygen and clear carbon dioxide. For patient with respiratory failure, NIV as an initial ventilation support has been reported to reduce mortality and the need of intubation in viral pneumonia (10). In our cohort, with the support of NIV, four cases (4.4%) recovered from respiratory failure and two cases in our cohort was successfully removed from IMV. However, MV, especially NIV, is considered as of high infection risk because of increased aerosolization; however, patients with IMV may have a higher demand of medical resources and a higher rate of secondary infection. So, in our COVID-19 management protocol, NIV is first introduced to COVID-19 patients with respiratory distress, and IMV is recommended to be applied if NIV failed to improve the respiratory distress or hypoxemia. After COVID-19 outbreak, 3,387 healthcare workers have been infected in China, but we do not worry about SARS-CoV-2 transmission in hospital because COVID-19 patients are separated from other patients, and healthcare workers wear personal protective equipment including caps, N95 masks, gloves, gowns, and face shields, and follow strict hygiene steps. In China, most of the healthcare worker infections occurred at the early stage of COVID-19 outbreak because the strong infectivity was not fully recognized and thus personal protection was not adequate at that time. With appropriate personal protection, the healthcare worker infections can be avoided even when the patients are with NIV, which were evidenced by few healthcare worker infections at the late period (February and March 2020) of COVID-19 outbreak in China.
CONCLUSIONS
Our data suggest that advanced age, coexisting chronic illness, and abnormal laboratory findings are common in the ventilated cases. Elevated d-dimer (>1.5 mg/L) at admission may suggest an increased possibility of IMV requirement with the progress of the disease, and coexisting COPD or chronic renal disease could help clinicians to identify COVID-19 patients with poor prognosis at an early stage.
ACKNOWLEDGMENTS
We thank all medical staff who are fighting against this public crisis and all the patients involved in the study. We also thank the hospital staffs for their efforts in collecting the data. We express sincere sympathies and deep condolences to the victims and bereaved families.
Supplementary Material
Footnotes
Drs Wang, Tang, Chen, and Ruan contributed equally and are joint first authors.
Dr. Li had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Li was responsible for concept and design. Drs. Wang, Tang, Chen, Liang, Guan, Sang, Tang, and Ruan were responsible for acquisition, analysis, or interpretation of data. Drs. Wang, Tang, Chen, and Ruan drafted the manuscript. Drs. Zhong and Li were responsible for critical revision of the manuscript for important intellectual content. Drs. Chen, Tang, and Ruan were involved in statistical analysis. Drs. Zhong and Li provided administrative, technical, and material support. Dr. Li supervised the project.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Azman AS, Luquero FJ. From China: hope and lessons for COVID-19 control. Lancet Infect Dis 2020; 20:30264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang F, Deng L, Zhang L, et al. Review of the clinical characteristics of Coronavirus Disease 2019 (COVID-19). J Gen Intern Med 2020; 35:1545–1549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020; 368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alhazzani W, Moller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Crit Care Med 2020; 48:e440–e469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 2020; 55:2000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang WH, Guan WJ, Li CC, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicenter) and outside Hubei (non-epicenter): A Nationwide Analysis of China. Eur Respir J 2020; 55:2000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020; 323:1061–1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung TM, Yam LY, So LK, et al. Effectiveness of noninvasive positive pressure ventilation in the treatment of acute respiratory failure in severe acute respiratory syndrome. Chest 2004; 126:845–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


