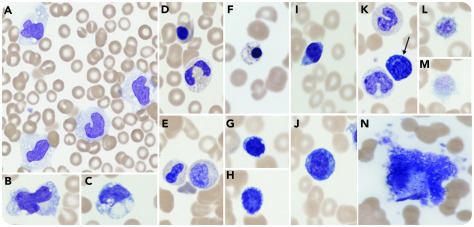
An 81-year-old man presented with shortness of breath, fever, hypoxia, and widespread diffuse infiltrates on a chest radiograph. Oral swab testing was positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; RNA reverse transcriptase–polymerase chain reaction RdRp gene). Despite therapy with oxygen and antibiotics, the patient deteriorated and required ventilator support. Comorbidities included hypertension, chronic renal disease, and restrictive lung disease. A blood film was prepared upon transfer to intensive care, 48 hours prior to death. Laboratory parameters at that time were: hemoglobin, 90 g/L; neutrophils, 2.78 × 109/L; lymphocytes, 1.06 × 109/L; monocytes, 2.5 × 109/L; and platelets, 44 × 109/L. Inflammatory markers linked to poor outcome rose during the admission with C-reactive protein reaching 406 mg/L and troponin reaching 1852 ng/L. The blood film (panels A-N; original magnification ×1000 for all panels; May-Grünwald–Giemsa stain) revealed: increased pleomorphic (panel A) and vacuolated monocytes (panels B-C); leukoerythroblastic features (panels D-E); nucleated red cells with dyserythropoiesis/basophilic stippling (panel F); lymphopenia, some with cytoplasmic vacuolation (panels G-H); lymphoplasmacytoid lymphocytes (panels I-J); an occasional plasma cell (panel K arrow); thrombocytopenia, giant platelets (panels L-M); and a circulating megakaryocyte (panel N).
None of these features is pathognomonic of SARS-CoV-2 infection but, in addition to previously reported lymphopenia and left-shifted granulopoiesis, we also note monocytosis, giant platelets, dyserythropoiesis, lymphoplasmacytoid lymphocytes, and leukoerythroblastic features commonly seen in patients requiring intensive support.