FIGURE 4.
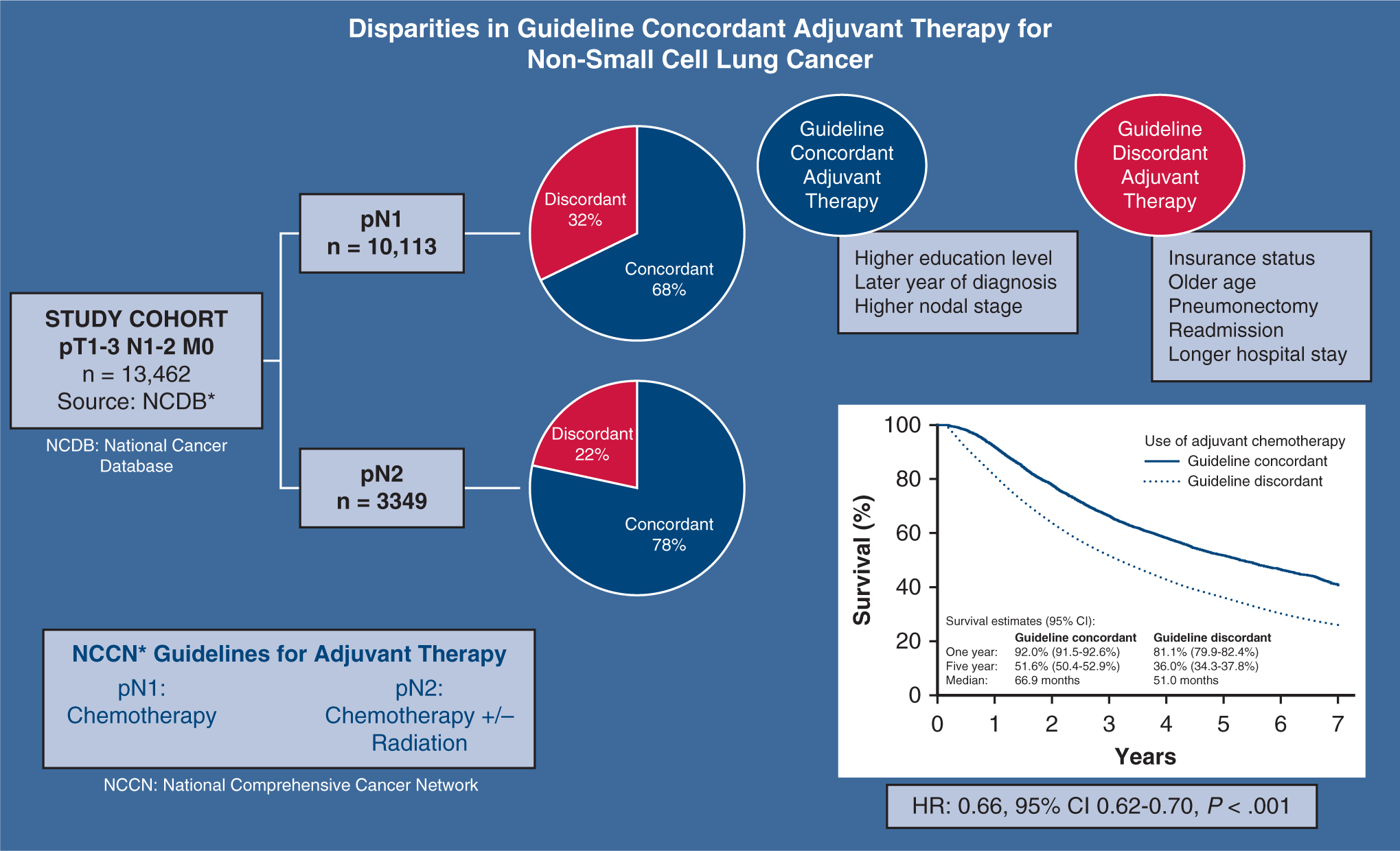
This study identified patients with resected T1–3 N1–2 M0 non-small cell lung cancer in the National Cancer Database (NCDB) between 2006 and 2013, and evaluated guideline-concordance with adjuvant therapy to determine the relationship between socioeconomic factors, use of recommended postoperative adjuvant therapy, and outcomes. Among patients with pN1 disease (n = 10,113) and pN2 disease (n = 3349), guideline-concordant adjuvant therapy was used in 6844 (67.7%) patients with pN1 and 2622 (78.3%) patients with pN2. After multivariable adjustment, insurance status, older age, pneumonectomy, readmission, and longer postoperative stays were associated with lower likelihood of guideline concordance, whereas increased education level, later year of diagnosis, and greater nodal stage were associated with greater concordance. Overall, patients treated with guideline-concordant therapy had superior survival (5-year survival: 51.6 vs 36.0%; hazard ratio [HR], 0.66; 95% confidence interval [CI], 0.62–0.70, P < .001). Socioeconomic factors, including insurance status and geographic region, are associated with disparities in use of adjuvant therapy as recommended by National Comprehensive Cancer Network (NCCN) guidelines, which significantly impact patient survival.
