Abstract
Background
In cardiac implantable electronic device management, confused electrocardiograms are sometimes encountered.
Case summary
We experienced a case of dizziness and presyncope, which was accompanied by irregular pacing spikes following QRS complexes, pacing failure, sensing failure, or something else. The patient’s second active pacemaker in her left chest was functioning normally. However, her old abdominal pacemaker had automatically changed from the OVO to VVI mode because of an elective replacement indicator. As a result, her old and second pacemakers had an interaction. Old invalid pacing spikes induced oversensing of the current pacemaker, which interfered with valid pacing.
Discussion
We experienced a rare case of dizziness and presyncope with confused pacing spikes. Physicians should be aware of the unexpected interactions that are possible with devices with automatic mode changes.
Keywords: Irregular pacing, Pacemaker interaction, Automatic mode change, Case report
Learning points
Awareness of the kind of unexpected interactions that are possible with devices with automatic mode changes.
When two or more pacemakers are present at the same time, we have to pay attention not only to the latest one but also the old devices.
Introduction
In recent years, the functions of cardiac implantable electronic devices have become more complex. In addition, an increasing amount of patients are undergoing multiple operations because of a prolonged lifespan. When managing cardiac implantable electronic devices, we sometimes encounter confusing electrocardiographic results. Inaccurate electrocardiographic interpretation may cause misdiagnosis.1,2 Therefore, accurately understanding these results is important.
Timeline
| Time | Events |
|---|---|
| 1965 | The implantation of a permanent epicardial pacemaker in her upper left abdomen for complete atrioventricular block. |
| 2002 | Generator exchange and added right ventricular lead (total two epicardial leads). |
| 2006 | Generator exchange. |
| 2008 | Several syncopal episodes. Elevated V-lead impedance. |
| Increased pacing threshold over 3 V/0.4 ms. | |
| Twitching of her diaphragm by output over 3.5 V/0.4 ms. | |
| A second pacemaker implantation via the left axillary vein. The old generator in the left upper abdomen with switched off and OVO mode. | |
| 6 September 2015 | Developed dizziness and intermittent pulse. Irregular pacing spikes following the QRS complexes in her electrocardiogram. |
| 13 September 2015 | Pacemaker check of her old abdominal pacemaker revealed the cause of this mechanism leading to the confused pacing spikes. |
Case presentation
A 61-year-old woman underwent implantation of a permanent epicardial pacemaker in her upper left abdomen for complete atrioventricular block at 10 years of age. The device was programmed to VVI mode. The generator was exchanged, and a new epicardial right ventricular lead (Medtronic 5071; Medtronic, Minneapolis, MN, USA) was added at 47 years of age. The generator (Kappa KDR731; Medtronic) was exchanged for the second time at 51 years of age. No adverse events were seen at routine pacemaker check-ups. However, at 53 years of age, the patient presented with several syncopal episodes. On checking the pacemaker, V-lead impedance was markedly elevated to 8786 Ohm. We changed the V-lead from bipolar to unipolar, which improved the impedance to 400 Ohm.
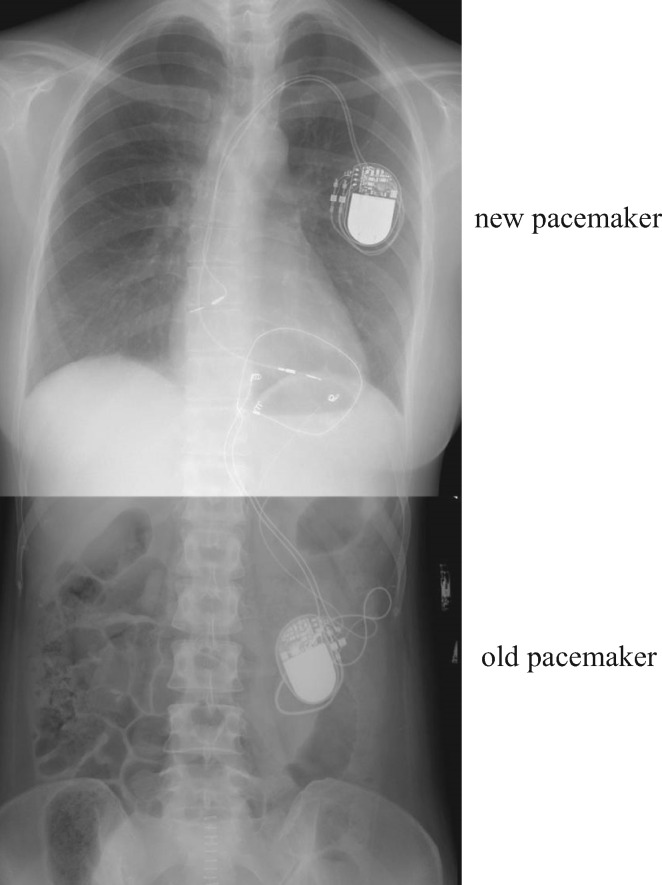
At 53 years of age, when the patient was hospitalized for a caesarean section, we performed another pacemaker check-up and found that the pacing threshold had increased. Therefore, we implanted a second pacemaker (EnPulse E2DR31; Medtronic) via the left axillary vein. The setting of the new pacemaker was DDD mode, and we set a lower rate of 50 ppm and an upper rate of 120 ppm. The old generator, which was placed in the left upper abdomen, was turned off and set to OVO mode. However, to avoid infection, we did not remove the old generator immediately after caesarean section, which would have required open surgery to remove her abdominal generator and leads. Open surgery would have been a high-risk procedure for the patient, especially postpartum. Therefore, both pacemakers were in place with the abdominal pacemaker not in use, and the other in use in her left chest (Figure 1). She was subsequently followed at our outpatient pacemaker clinic.
Figure 1.
Chest X-ray and abdominal X-ray images showing the new pacemaker in the patient’s left chest and the older pacemaker in her abdomen.
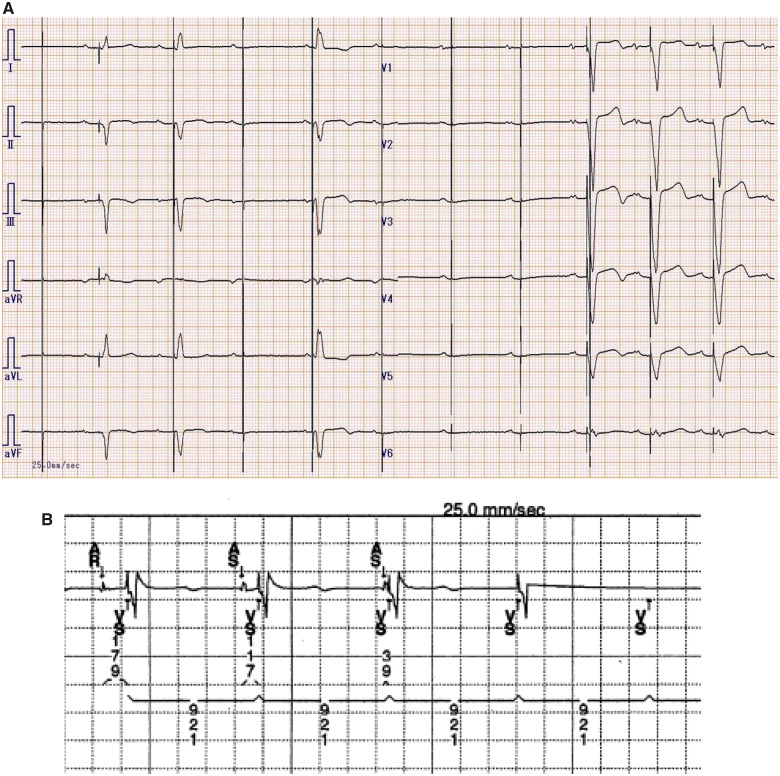
The patient developed dizziness and an intermittent pulse on 6 September 2015, and she visited our outpatient pacemaker clinic. Her electrocardiogram and intracardiac electrogram showed confusing pacing spikes following or not following QRS complexes (Figure 2A and B). Her Holter monitor showed waveform-like pacing failure, and she was admitted to our hospital because of dizziness and presyncope later in September 2015. We questioned whether the mechanism underlying the confusing pacing spikes was pacing failure, sensing failure, or something else.
Figure 2.
(A) Electrocardiogram. Old pacing spikes without QRS complexes secondary to pacing failure, new valid pacing spikes and QRS complexes following the P wave, and old and new pacing spikes and a fusion QRS complex can be seen. In addition, old valid pacing spikes and QRS complexes not following the P wave, new pacing spikes with QRS following the P wave, and old pacing spikes just after new pacing spikes can be seen. (B) Intracardiac electrogram.
Discussion
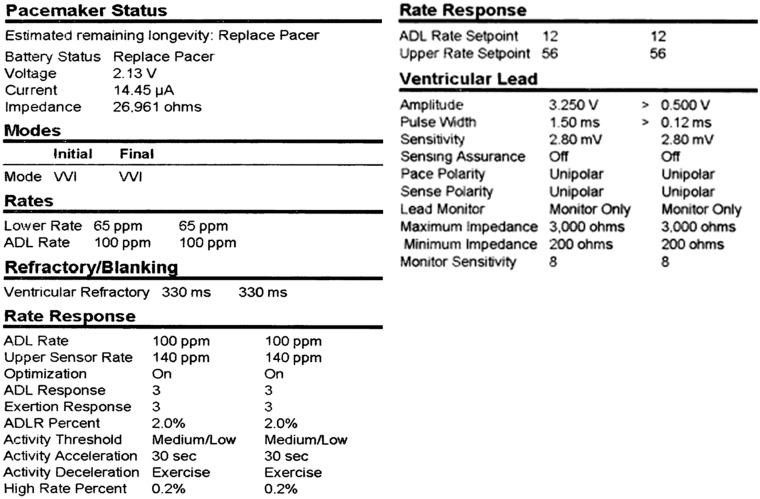
At a pacemaker check-up after admission, the patient’s active pacemaker in her left chest was functioning normally; therefore, we checked the older abdominal pacemaker. When we implanted the new subclavian pacemaker, we turned off the older pacemaker and set it to OVO mode. However, the abdominal pacemaker had automatically changed to VVI mode and 65 b.p.m. because of an elective replacement indicator (ERI) (Figure 3). The output from the ERI induced a pacing spike with and without captured QRS complexes. Old invalid pacing spikes induced oversensing of the newer pacemaker, which interfered with valid pacing and caused the confusing pacing spikes. Figure 2A shows old pacing spikes without QRS complexes secondary to pacing failure, new valid pacing spikes and QRS complexes following the P wave, and old and new pacing spikes and a fusion QRS complex. Figure 2A also shows old valid pacing spikes and QRS complexes not following the P wave, new pacing spikes with QRS following the P wave, and old pacing spikes just after new pacing spikes. One reason for these findings is that we checked only the active pacemaker in the patient’s chest. Another reason is that we overlooked the change in mode when the older pacemaker reached the trigger for the ERI. The final reason is that we did not extract the old generator when we implanted the new pacemaker.
Figure 3.
The patient’s old abdominal device parameters. The pacing mode automatically changed from OVO to VVI at 65 ppm.
Changing the mode of the older abdominal generator is impossible. Therefore, we changed the output of the older abdominal generator to the minimum setting and the sensitivity of the ventricular lead of the current generator from 2.0 mV to 4.0 mV. This change avoided interference from the old generator; interactions between the two pacemakers did not recur, and the patient’s dizziness resolved. We removed the old abdominal generator during the next generator exchange.
To the best of our knowledge, only one published case report described dual pacemaker interaction with an epicardial ventricular pacemaker.3 Electrocardiographic and clinical manifestations might have been poorly recorded or interpreted, and this condition might have been misdiagnosed.
The clinical indications for cardiac rhythm management devices, such as pacemakers, have expanded. The phenomenon observed in our patient is rare. However, in the future, a number of patients with congenital heart disease may need to exchange their cardiac rhythm management devices and have them moved from their abdomen to the left axillary vein.4 Our case raises awareness of the unexpected interactions that are possible with devices with automatic mode changes. In addition, when patients have two or more pacemakers in place concurrently, we must be aware of both the latest and older devices.
Patient perspective
After discovering the cause of the patient’s symptoms and changing the pacemaker settings, she was satisfied and experienced no further dizziness, fainting, and presyncope.
Lead author biography

Toshiya Kojima is an Assistant Professor of Department of Cardiovascular Medicine, The University of Tokyo. He had cardiology training in Sakakibara Heart Institute and The University of Tokyo Hospital.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Supplementary Material
Acknowledgements
The case report was approved by the Institutional Review Board of the University of Tokyo, Tokyo, Japan (2650). The authors thank Jane Charbonneau, DVM, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
References
- 1. Myers GH, Kresh YM, Parsonnet V.. Characteristics of intracardiac electrograms. Pacing Clin Electrophysiol 1978;1:90–103. [DOI] [PubMed] [Google Scholar]
- 2. Perrins EJ, Suttan R.. Arrhythmias in pacing. Med Clin North Am 1984;68:1111–1138. [DOI] [PubMed] [Google Scholar]
- 3. Haim M, Chaudhry MG, Orlov MV, Haffajee CI.. Two pacemaker systems in a patient with complete heart block: double trouble? Pacing Clin Electrophysiol 2008;31:1046–1047. [DOI] [PubMed] [Google Scholar]
- 4. Czosek RJ, Meganathan K, Anderson JB, Knilans TK, Marino BS, Heaton PC.. Cardiac rhythm devices in the pediatric population: utilization and complications. Heart Rhythm 2012;9:199–208. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.