Abstract
Introduction
Interpersonal violence cases make up a significant portion of the trauma cases seen in emergency centres in South Africa. Community assaults are extremely violent attacks on suspected perpetrators by members of the community aimed at inflicting serious injury. The aim of this study was to profile the major interpersonal violence cases at Kalafong Hospital with emphasis on the community assaults and how this group compares with non- community assaults regarding demographics, surgical intervention and mortality.
Methods
A retrospective analysis was conducted of the major interpersonal violence cases seen over a one-year period (1 January 2016 to 31 December 2016) at Kalafong Hospital, Pretoria, South Africa. Data was manually collected and entered into a Microsoft Excel spreadsheet. The Stata 13 statistical program was used for data analysis.
Results
During the study period, a total of 578 cases were analysed. Penetrating trauma accounted for 446 (77.2%) cases and blunt trauma for 132 (22.8%) cases. The number of community assault cases was 75 (12.9%). A total of 28 deaths were recorded during this period. Community assaults accounted for 13 (46.4%) of these deaths. Community assault cases had a significantly higher mortality compared to non-community assault cases with 17.3% versus 3%; Odds ratio 6.82 (95% CI 3.04–15.33, p < 0.001). The community assault group also showed a statistically significant difference in the intensive care admission rate with 15.3% compared to 6.9% in the interpersonal violence cases; Odds ratio 2.41 (CI 1.07–5.43, p = 0.028).
Conclusion
Community assault cases may present with similar demographics when compared to non-community assault cases, but the difference in disposition and outcome was highlighted in this study with a higher intensive care unit admission rate and a higher mortality rate. A multi-centre follow-up study is recommended to compare demographics across Pretoria and to monitor trends in this subgroup of interpersonal violence cases.
Keywords: Interpersonal violence, Community assaults, Trauma
African relevance
-
•
character count correct
-
•
end centence after population with full stop
-
•
This study compared community assaults to non-community assaults regarding demographics, disposition and mortality.
Introduction
Interpersonal violence is defined as the intentional use of physical force against another person that results in injury, death or harm [1]. There are two specialized groups classified under interpersonal violence, family or partner violence and community violence [1]. The estimated mortality rate in 2011 due to interpersonal violence in low- and middle-income countries was 8 per 100,000 people, compared to 3.3 per 100,000 in high-income countries [1].
In South Africa interpersonal violence accounted for 14.1% of all non-natural deaths in 2015 [2]. A further prediction is that soon the injury mortality rate will exceed that of HIV, tuberculosis, malaria and obstetric-related deaths combined [3].
The United Nations Sustainable Development Goals Target 16.1 of 2015 sets out to reduce all forms of violence and related death rates by 2030 [4].
National data regarding non-fatal injuries are scarce. Single-centre studies have been published, but they cover limited periods and small geographic locations. Data from 2012 to 2016 in Kwazulu-Natal, provided an overview of the burden of trauma in the province [5]. Of the 197,219 trauma patients that visited the emergency centre in 2013–2014, 45% were admitted due to interpersonal violence [5].
Groote Schuur Hospital in Cape Town treated 9236 trauma patients in 2010–2011, with interpersonal violence accounting for 71.6% of the total number of patients treated [6]. Ten percent of these injuries were attributed to community assault [6].
A five-year review of all major trauma cases in Ngwelezane Hospital from 2009 to 2013 found that interpersonal violence accounted for 67.4% of the cases, with 9.1% as a result of community assaults [7].
Community assaults have been described as unstructured, extremely violent attacks on suspected perpetrators by members of the community [8]. The aim is to inflict serious injury to punish the perpetrator and serve as a warning to others [9]. The most common weapon used is a sjambok – a robust leather whip that produces extensive soft tissue trauma [10]. Sjamboks are about 1 m long, cylindrical in cross-section tapering to a fine point and made of firm leather [11].
A study in Cape Town identified 148 cases and indicated higher injury-severity scores compared to non-community assaults [10]. Ngwelezane Hospital in Kwazulu-Natal demonstrated a 15.9% mortality rate in this group [9].
The aim of this study was to profile the major interpersonal violence cases at Kalafong Hospital with emphasis on the community assault cases and how this group compares with non- community assaults regarding demographics, surgical intervention and mortality. There have not been any previous publications regarding interpersonal violence or community assaults from this centre. Kalafong Hospital is a tertiary, 709 bed public hospital associated with the University of Pretoria in the Western suburbs of Pretoria, South Africa.
Methods
This was a descriptive retrospective observational study. Cases from 1 January 2016 to 31 December 2016 were included in the study. The cases were identified in the emergency centre register book containing manual entries by nursing staff of patients seen in the resuscitation area. It consists of patient details, mechanism of injury and disposition. All patients older than eighteen years with a classification of Red (Emergency) or Orange (Very urgent) as classified by the South African Triage Scale [12], with the mechanism of injury due to interpersonal violence were included. Patients with burn wounds were excluded due to the referral of these patients to burn centres in other hospitals.
Files were requested from records and data were captured manually onto a data sheet; personal identifiers were excluded. Data were entered into a standard Microsoft Excel spreadsheet Version 1910 of Microsoft Office 2016 (Microsoft Corporation, Redmond, Washington, USA). The Stata 13 statistical analysis software program (StataCorp LLC, Texas, USA) was used for data analysis. Descriptive statistics along with 95% confidence intervals were recorded. Both univariable and multivariable data analysis were employed to assess the association with mortality. Testing was at the 0.05 level of significance.
Approval for this study was obtained from the chief executive officer and manager of Kalafong Hospital. Ethical approval was obtained from the University of Pretoria Ethics Committee.
Results
During the study period, a total number of 598 interpersonal violence cases were identified. Of these, 578 could be traced and analysed. The mean age was 30.9 years (standard deviation of 8.8 years). Most of the cases were male (n = 549, 94.9%), with females accounting for 29 cases (5.1%).
December was the busiest month (n = 92, 15.9%), followed by October (n = 54, 9.3%). Most injuries occurred over weekends and on public holidays (N = 405, 70%).
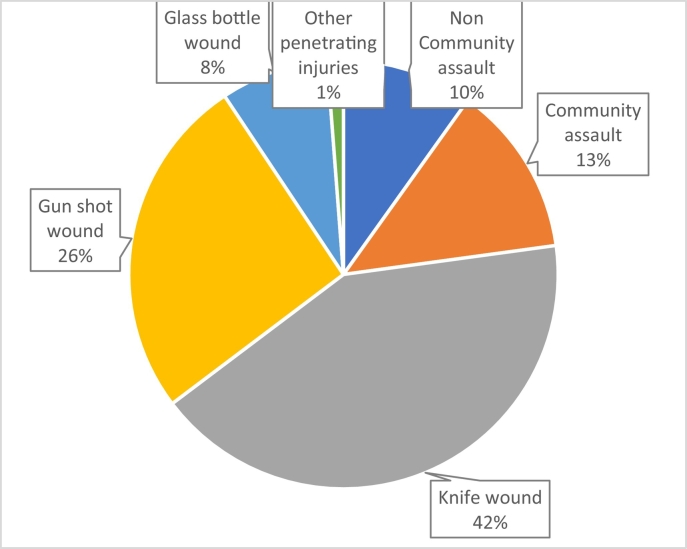
Penetrating trauma accounted for 446 (77.2%) cases and 132 (22.8%) were due to blunt trauma. Penetrating trauma involved knife wounds (n = 242, 53.7%), gun-shot wounds (n = 150, 33.3%) and glass bottle wounds (n = 47, 10.4%). The number of community assault cases totalled 75 (12.9%) (Fig. 1).
Fig. 1.
Distribution of mechanism of injury.
The disposition of the patients was as follows: admission to hospital (n = 462, 79.9%), demise in emergency centre (n = 13, 2.2%) and discharge from emergency centre (n = 103, 17.8%).
One hundred and eighty major primary surgical interventions were performed comprising of general surgery (n = 85, 47.2%), orthopaedic surgery (n = 63, 35%) and neurosurgery (n = 21, 11.7%). There was no statistical significance difference between the community assault cases compared to non-community assault cases regarding surgical interventions.
A total of 28 deaths were recorded during this period. There were 17 blunt cases (60.7%) and 11 penetrating cases (39.3%). Thirteen deaths (46.4%) occurred in the emergency centre and 15 (53.6%) in the Intensive care unit.
Community assaults accounted for 13 deaths. Two (15.4%) were due to renal failure secondary to traumatic rhabdomyolysis, they demised in the intensive care unit. Six (46.1%) were due to isolated severe traumatic brain injury as confirmed on computed tomography radiological investigations. Five (38.5%) demised before any radiological investigations could be done, they presented with extensive blunt trauma to the head, neck, torso, abdomen and extremities.
When community assault cases were compared to non-community assault cases, there was a significantly higher mortality in this group: a 17.3% mortality versus a 3% mortality in non-community assault cases. (OR 6.82, 95% CI [3.04–15.33], p-value <0.001) There was also a significantly higher rate of intensive care unit admissions in the community assault group. (OR 2.41, 95% CI [1.07–5.43], p-value 0.023). See Table 1.
Table 1.
Characteristics and outcome comparison.
| Non-community assaults N = 503 |
Community assaults N = 75 |
p-Value | |
|---|---|---|---|
| Gender N(%) | |||
| Male | 474(94.2) | 75(100) | |
| Female | 29(5.8) | 0(0) | |
| Age | |||
| Mean ± SD | 31.1 ± 8.9 | 30.1 ± 7.9 | 0.39 |
| Disposition N(%) | |||
| Ward admission | 375(93.1) | 50(84.7) | |
| ICU admission | 28(6.9) | 9(15.3) | 0.023 |
| Outcome N(%) | |||
| Demised | 15(3) | 13(17.3) | p < 0.001 |
Discussion
This is the first published data for interpersonal violence cases treated in a Pretoria hospital. The demographics are in keeping with previous studies regarding interpersonal violence in South Africa. It is evident that young men are most at risk. Penetrating trauma was responsible for the majority of cases with knife wounds accounting for more than half of those.
A 17.3% mortality in the community assault subgroup was recorded. In Ngwelezane Hospital, Kwazulu-Natal, the mortality rate was found to be 15.9% in 2009 [9]. Whether this trend correlates with the rest of Gauteng remains to be investigated. It is clear from the data that there is a higher mortality associated with community assault cases compared to non-community assault cases (p-value <0.001). The study also indicated the need for specialised care and resource allocation as demonstrated by the intensive care unit admission rate in the community assault group.
A limitation of this study is that it was retrospective and restricted to a single centre over a one-year period. Twenty files could not be traced due to wrong entry details; either file number or presenting complaint. After discharge patients were not followed up, mortalities could have been missed if they presented to another health establishment. Severe non-accidental burn injuries were excluded due to difficulty with follow up.
Once thought of as rough justice aimed at teaching a lesson, community assaults now seem to be more violent with more severe injuries. They may present with similar demographics when compared to non-community assault cases, but the difference in disposition and outcome was highlighted with a higher intensive care unit admission rate and a higher mortality rate. A multi-centre follow-up study is recommended to compare demographics across Pretoria and to monitor trends in this subgroup of interpersonal violence cases. It could also highlight areas prone to community assaults to aid in preventative programs and community education.
Dissemination of results
Results of this study were shared with emergency unit staff members at Kalafong and Steve Biko academic hospital through a presentation. It was also shared with the management of Kalafong hospital through an e-mail highlighting the findings of the study.
Authors' contribution
Authors contributed as follow to the conception or design of the work; the acquisition analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content:
RH contributed 80% and MG contributed 20%.
All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Mercy J., Hillis S., Butchart A., Bellis M., Ward C., Fang X. Interpersonal violence: global impact and paths to prevention. In: Mock C, Nugent R, Kobusingye O, Smith K, editors. Injury prevention and environmental health. 3rd ed. The International Bank for Reconstruction and Development/The World Bank; Washington: 2017. pp. 71–96. [PubMed] [Google Scholar]
- 2.Statistics South Africa Mortality and causes of death in South Africa, 2015: findings from death notifications. 2015. http://www.statssa.gov.za/publications/P03093/P030932015.pdf
- 3.Lozano R., Naghari M., Foreman K., Lim S., Shibuya K., Aboyans V. Global and regional mortality from 235 causes of death for age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Transforming our world: the 2030 agenda for sustainable development. 2015. https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Susrainable%20Development%20web.pdf;
- 5.Lutge E., Moodley N., Tefera A., Sartorius B., Hardcastle T., Clarke D. A hospital based surveillance system to assess the burden of trauma in KwaZulu-Natal Province South Africa. Int J Care Injur. 2016;47:135–140. doi: 10.1016/j.injury.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Nicol A., Knowlton L.M., Schuurman N., Matzopoulos R., Zargaran E., Cinnamon J. Trauma surveillance in Cape Town, South Africa: an analysis of 9 236 consecutive trauma centre admissions. J Am Med Assoc Surg. 2014;149(6):549–556. doi: 10.1001/jamasurg.2013.5267. [DOI] [PubMed] [Google Scholar]
- 7.Lewis C., Wood D. Interpersonal violence as a major contributor towards skewed burden of trauma in KwaZulu-Natal, South Africa. S Afr Med J. 2015;105(10):827–830. doi: 10.7196/SAMJnew.8380. [DOI] [PubMed] [Google Scholar]
- 8.Buur L., Jensen S. Introduction: vigilantism and the policing of everyday life in South Africa. J Afr Stud. 2004;63(2):139–152. [Google Scholar]
- 9.Proctor M., Carter N., Barker P. Community assault – the cost of rough justice. S Afr Med J. 2009;99(3):160–161. [PubMed] [Google Scholar]
- 10.Forgus S., Delva W., Hauptfleisch C., Govender S., Blits J. Community v. non-community assault among adults in Khayelitsha, Western Cape, South Africa: a case count and comparison of injury severity. S Afr Med J. 2014;104(4):299–301. doi: 10.7196/samj.7615. [DOI] [PubMed] [Google Scholar]
- 11.Smith W., Hardcastle T. A crushing experience: the spectrum and outcome of soft tissue injury and myonephropathic syndrome at an urban South African university hospital. Afr J Emerg Med. 2011;1:17–24. [Google Scholar]
- 12.Emergency Medicine Society of South Africa The South African Triage Scale. 2012. http://emssa.org.za/sats/ [Internet]. Available from: accessed 18 November 2019.