Abstract
Psychiatric hospitals play an important role in supporting patients with mental illness to relieve symptoms and improve functioning in a physically and psychologically safe environment. However, these hospitals are also vulnerable to emerging infectious diseases. In early 2020, a psychiatric hospital and a psychiatric unit were reported to have nosocomial coronavirus disease 2019 (COVID-19) infection. A large number of patients and staff were severely impacted. This type of nosocomial infection threatens patient safety and quality of care.
By learning from previous experiences of severe acute respiratory syndrome (SARS) and previous studies, psychiatric hospitals can provide safeguards to prevent nosocomial infection among patients and staff during an epidemic or biological disaster. These strategies include a series of actions such as following national guidelines for infection control, reserving adequate support for disinfection equipment, providing relevant and sufficient pro-service and in-service education and training, establishing regular surveillance of hand hygiene habits, proper communication and health education, and providing opportunities for vaccination if possible. Based on the harm reduction concept, staff division of office breaks and ward classification and shunting are recommended and should be further implemented.
Keywords: Coronavirus disease 2019 (COVID-19), Severe acute respiratory syndrome (SARS), Biological disaster, Psychiatric hospital, Infection control, Hospital accreditation, Patient safety
1. Introduction-- the unique challenge of infection control in psychiatric hospitals
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a “Public Health Emergency of International Concern” on 30 January 2020 and scaled it up to a “pandemic” on 11 March. As of 20 June 2020, there were over 10 million confirmed cases and over 500,000 deceased in 216 countries (World Health Organization, 2020). Cities and even states have been on lockdown, and medical systems in countries with a higher number of patients are seriously challenged. Given the numbers of people infected and affected as well as the socioeconomic domains affected (Tandon, 2020), COVID-19 has become an overwhelming biological disaster in modern history.
Even after the deinstitutionalization era, in most countries, psychiatric hospitals continue to play an important role in the treatment and rehabilitation of people with mental illness who need longer support and treatment. Two events in two different countries during the COVID-19 epidemic underline the importance and necessity of infection control in psychiatric hospitals. In China, more than 50 patients and 30 staff members were infected in the Wuhan Mental Health Center (Gan et al., 2020; Shih et al., 2020). In South Korea, 99 out of 102 patients were infected in a psychiatric ward of Daenam Hospital (Song, 2020). These events highlight the vulnerability of infection prevention and control in psychiatric hospitals. As part of medical service delivery, psychiatric hospitals cannot escape the COVID-19 epidemic. Therefore, infection control issues should be addressed in psychiatric hospitals.
2. Taiwan’s response to COVID-19
Of 23 million Taiwanese workers, 85,000 are in Mainland China, and Taiwan is only 130 km from mainland China. COVID-19 was initially expected to quickly and severely influence Taiwan. Onboard quarantine of all direct flights departing from Wuhan was implemented on December 31, 2019, and the Central Epidemic Command Center (CECC), a branch of the National Health Command Center led by the Minister of the Ministry of Health and Welfare, was organized on January 20, 2020, one day before the first imported COVID-19 case was identified.
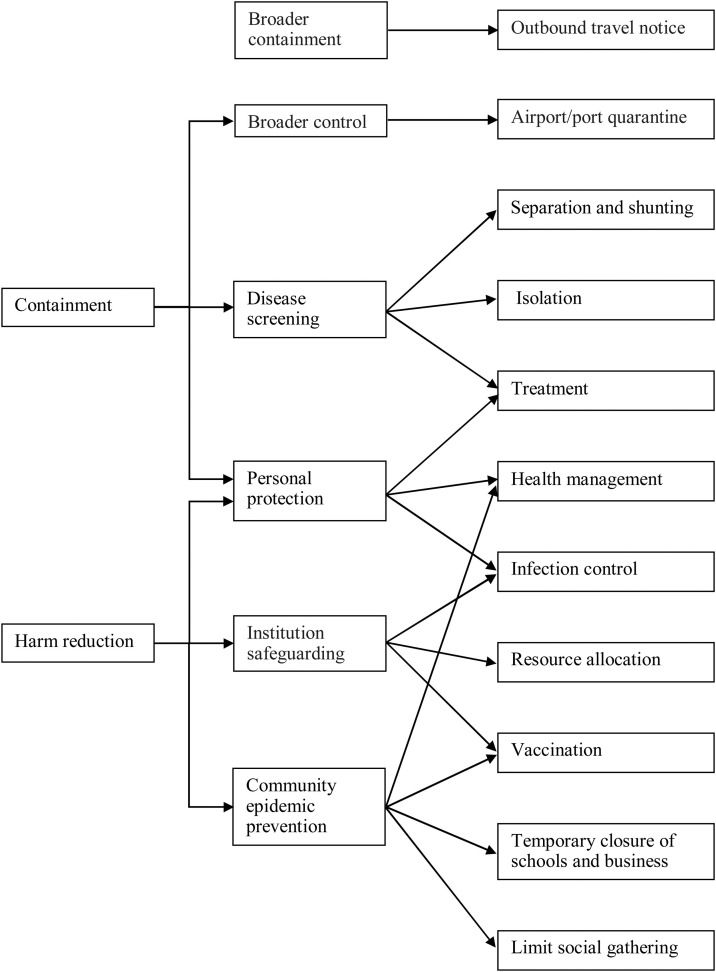
Since the first imported case was identified, tension has spread nationwide. The CECC took further steps quickly to respond. According to Wang et al. (2020), the CECC announced 124 actions from January 20 to February 24, including (1) border control from the air and sea, including travel restrictions and cruise ship bans; (2) case identification (using new data and technology) and the integration of patients’ 14-day travel history into the National Health Insurance Administration and Immigration Agency database; (3) quarantine of suspicious cases and electronic monitoring of quarantined individuals via government-issued cell phones; (4) proactive case finding; (5) resource allocation (assessing and managing capacity), such as setting up test sites and taking over production of surgical and N95 masks (more than 10 million per day); (6) reassurance and education of the public while fighting fake messages, such as investigating rumors that started a toilet paper panic and prosecuting a man for claiming that cyanide wards off the coronavirus; (7) negotiation with other countries and regions; (8) the formulation of policies for schools and childcare; and (9) relief to businesses. In summary, Taiwan surprised the world by successfully slowing a large-scale epidemic outbreak of COVID-19 by adopting data analytics and rapidly applying new technology and proactive testing (Wang et al., 2020). The major tasks of CECC and whole nation are summarized in Fig. 1 (Chen, 2020).
Fig. 1.
National strategies of infection control in Taiwan.
The Taiwanese government has also prepared medical services nationwide for possible epidemics. The first step is to cross-check the databases of immigration and National Health Insurance to help clinicians obtain travel histories early. A history of travel, occupation, contact and cluster (TOCC) is required when individuals arrive at hospitals and clinics, and the travel history is shown on individuals’ National Health Insurance card. The level of infection control in hospitals and long-term care institutions has also tightened along with the worsening outbreaks of COVID-19 in other countries. Staff in these services are required to be separated by groups, spaces, and time schedules to prevent cross-infection between communities and hospitals. Online training courses were provided quickly after the epidemic started. The necessary steps, which resulted from the lessons of the severe acute respiratory syndrome (SARS) epidemic in 2003, have changed constantly and quickly nationwide to respond to the COVID-19 epidemic worldwide.
3. Implementing a nationwide infection control system
SARS, which first appeared in China, was the first serious new emerging infectious disease in this century (World Health Organization, 2003). Nosocomial infection was the major route of transmission in Taiwan (Lee et al., 2003; McDonald et al., 2004), and a regional hospital in North Taiwan and a medical center in Southern Taiwan announced lockdown to prevent the spread of the virus. A high mortality rate was reported, and 181 of 668 probable cases (27 %) died (Chen et al., 2005). Without previous experience with this pathogen, all Taiwanese people faced unprecedented fears. Anxiety and panic were common. The impacts of the medical shortage and burnout, social isolation and discrimination, as well as a lack of transportation and economic downturn were harsh enough to be considered psychological trauma in many Taiwanese.
After SARS, infection prevention and control throughout Taiwan was critically inspected (Taiwan Centers of Disease Control (2013)). A series of steps were planned, ranging from border control to public awareness (Chen et al., 2005). The government established a more centralized disaster management center to focus on large-outbreak responses. Investment in laboratories for screening tests and vaccines for any type of infectious disease increased. Collaborations between different public sectors under the power of authorized command centers were improved. The goal of all of these efforts was to contain an outbreak at an early stage, which provides a greater chance of success than a later response and clearly puts less strain on the healthcare system.
4. Implementation of infection prevention and control in psychiatric hospitals
Infection prevention and control has been one of the mandated domains in the accreditation process of psychiatric hospitals for 20 years in Taiwan (Taiwan Joint of Commision, 2019) and 30 years in the United States (Loving et al., 1992). These requirements are not different from the infection control standards for general hospitals. For example, to receive accreditation, there should be a particular commission for infection control at the administrative level and sufficient manpower specialized in infection control with appropriate continuing education hours. In addition, contingency plans, regulations and protocols, environmental designs and machine sterilization management, and continuous surveillance and staff education schedules are mandatory components. Psychiatric hospitals are also required to have a proper supply of adequate protective equipment and other disinfection goods (Taiwan Joint of Commision, 2019). Nonetheless, few studies have addressed infection control in psychiatric clinical settings in recent decades. In a recent meta-analysis, only 1 (<1%) out of more than 300 good-quality patient safety studies focused on infection control compared to other issues such as violence and suicide (Thibaut et al., 2019).
Infection control remains a major challenge in psychiatric hospitals despite these regulations. Healthcare-related (nosocomial) infections are not uncommon in psychiatric hospitals. In a survey of healthcare-related infection measures and rates in 284 private psychiatric hospitals in the United States, 103 responded (Loving et al., 1992). The reported median healthcare-related infection rate was 0.04 (n = 28) measured by the patient discharge rate and 0.01 (n = 10) measured by patient-days. Almeida and Pedroso (1999) investigated the infection rate in a 30-bed male ward of a public psychiatric hospital and found that 16 individuals had 18 infections during 7 months. The healthcare-related infection rate was 6.7 per 1000 patient-days. Half of these infections were the common cold. However, the cost of treatment increased due to the use of antibiotics and other supportive treatments (Almeida and Pedroso, 1999). Healthcare-related infections also increase the burden and care load of staff (Li et al., 2019). Below, implementation strategies will be discussed according to three levels of psychiatric hospital, mainly administrative level, staff level, and patient level.
4.1. Infection control on the administrative level
The medical system in Taiwan was badly affected during the SARS period. Fortunately, psychiatric hospitals survived and had no nosocomial infection at that time. To date, psychiatric hospitals in Taiwan still receive strict infection control regulations. These regulations include several domains (Taiwan Centers of Disease Control, 2019). The audit process is quite strict; an audit must be performed at least once by the local health authority, and national hospital accreditation must be processed every three or four years. These strict standards guide psychiatric hospitals to prepare infection control for any kind of infectious disease, such as scabies, tuberculosis, influenza, and dengue fever.
According to the standards of the Taiwan CDC, at the administrative level, there should be an infection control committee. A nurse and doctor specializing in infection control should be employed, and these individuals must have an adequate amount of related training every year. Infection control education hours and personal protection equipment for staff should be properly supplied. These are not only essential for safety but also serve as a psychological boost. According to insider views reported in news articles, staff in Wuhan Mental Health Center overlooked the risk of COVID-19 infection; combined with the lack of supplies, this led to the spread of COVID-19 (Shih et al., 2020). These opinions highlight the importance of provision of adequate education and training on infection control in psychiatric hospitals.
Space issues are also critical in infection prevention and control. The possible infectious routes of COVID-19 in hospitalized patients with mental illness include: (1) before admission, (2) visiting physicians outside for other physical conditions, or seeing family and friends in communities, and (3) becoming a victim of nosocomial infection. Most psychiatric hospitals have space arrangement plans for environmental support when people with mental illness also have infectious diseases in accordance with above possible infectious sources, usually include “observation area” for the newly admitted, “quarantine area” for the suspected contact, and “ordinary area” for people without any contact with COVID-19 victims. The standards for infection control by the Taiwan CDC require psychiatric hospitals to have separate routes and spaces for outpatient clinics and wards (Taiwan Centers of Disease Control, 2019).
In crowds or areas where people live close together, people are more likely to be infected (Association for Professionals in Infection Control and Epidemiology (2020)). People in psychiatric wards might attend groups or use recreational equipment, which may also predispose them to infection (Fukuta and Muder, 2013). The emphasis on prevention of nosocomial COVID-19 infection are more rigorous than usual since the infectious route of COVID-19 is not well identified so far. Not only space rearrangement, but also procedures of disinfection. Professionals should wash their hands when they move from one area to another area of different degree of infection control. Environmental support of disinfection is also needed. Well-designed directions, visual guidance, and convenient devices, such as hooks of hanging clean gowns before leaving ordinary area, should be considerate in order to prove accurate execution of infection control.
Rapid emergency operations usually require advance planning. The Taiwan CDC has asked hospitals to formulate contingency plans for emerging infectious diseases or large-scale infections and to formulate principles and sequences for supporting units and personnel (Taiwan Centers of Disease Control, 2019). In the event of an emerging infectious disease epidemic or a large-scale infection event, epidemic prevention measures and action plans should be implemented in accordance with the latest regulations of the competent health authority. Recently, staff in psychiatric hospitals in Taiwan have been required to be separated by groups, spaces, and time schedules to prevent cross-infection between communities and hospitals. These necessary steps, which emerged from the lessons of the SARS epidemic in 2003, have changed constantly and quickly nationwide to respond to the COVID-19 epidemic worldwide.
4.2. Staff-level infection prevention in psychiatric hospitals
Facing with the new and emergent COVID-19, no place could fully prepare beforehand. However, staff ignored or overlooked the risk of COVID-19 infection, which may have contributed to the spread of COVID-19 in Wuhan Mental Health Center (Shih et al., 2020). Staff are also at risk of developing anxiety, depression and sleep disturbance (Huang and Zhao, 2020). Unbiased and instant information provision is critical to maintain mental health (Banerjee and Nair, 2020; Hiremath et al., 2020). To avoid misinformation, the Taiwan CDC has offered 2 live conferences and 12 online courses to improve the understanding of staff at all levels of hospitals and facilities in early March.
Both adequate knowledge and appropriate training are needed to maintain the quality of infection control in psychiatric hospitals. Piai-Morais, Fortaleza, and Figueiredo (2015) reported that 40.6 % of nursing procedures presented a moderate to high risk of biohazard exposure, including low adherence to hand hygiene (1.2 % before procedures, 2.9 % after procedures), inappropriate use of gloves, and other instances of noncompliance with the standards of good practice for preventing and controlling infection, such as a lack of concurrent/terminal cleaning of dirty beds (132 instances) and careless manipulation of sharp devices (Piai-Morais et al., 2015). This study highlights the need to establish a standard of operations and surveillance of procedures in infection control.
4.3. Infection control at the patient level
Environmental and patient characteristics contribute to the complexity of infection control in psychiatric hospitals. Untreated or undertreated mental illness puts patients at increased risk of infection because of risky behavior and an unsafe environment (Association for Professionals in Infection Control and Epidemiology, 2020). People with mental illnesses may have decreased resistance to infection because of age, underlying medical conditions, substance abuse (especially smoking), and other comorbid physical and psychiatric conditions (Kavoor, 2020). Mental illness can have both short-term and long-term negative effects by leading to poor health behaviors, diminished immune functioning, and negative disease outcomes (Association for Professionals in Infection Control and Epidemiology, 2020). In addition, psychiatric symptoms and comorbidities, such as impaired judgment, poor impulse control, reduced self-care, irregular or poor medication compliance, lack of personal hygiene, poor nutrition, and a lack of health management, might predispose people with mental illness to infectious risks (Association for Professionals in Infection Control and Epidemiology, 2020).
In psychiatric hospitals or long-term care facilities, people with mental illnesses are often ambulatory, stay longer than patients in general hospitals, and might have limited cognition to comprehend rules and follow sterilization procedures. Group events such as group therapies and recreational activities may also contribute to the dissemination of infection (Fukuta and Muder, 2013).
People with mental illnesses are also at increased risk of infection in the community (Kavoor, 2020). During the COVID-19 outbreak, there have been debates regarding whether day care programs in psychiatric hospitals, rehabilitation, or long-term care facilities should be closed. Proponents worry that patients in these programs might also become victims of nosocomial infection, and viruses could be spread between patients in the same program. Opponents assert that patients might wander around the community. Without a structured program and supervised health behaviors, patients are more likely to become infected. This might be related to the household or type of facility in which they live as well as their self-care behaviors, which could lead to an increased risk for infections that could spread to their family members, other residents, and professionals they might encounter (Association for Professionals in Infection Control and Epidemiology, 2020).
Unlike health professionals who have basic training in infection control, people might not comprehend infection control operations, such as the importance of quarantine and hand washing, which may result in the violation of regulations. Knowledge of communicable infections should be provided, and infection control should be addressed through a good communication process for patients and their family members. The individuality and uniqueness of this communication should take into account the family and cultural context (Santos de Aguiar et al. (2015)) and should include skill teaching, such as hand washing and cough control (Fedoriw and Meijer, 2013).
Patients should be encouraged to receive vaccinations whenever possible. When there is an infected person in the ward, patients are encouraged to wear masks and increase the intensity of hand hygiene. Influenza monitoring and alerts are essential for laboratory-confirmed cases. Influenza was present in a total of 20 episodes during the studied period. A maximum of 25 % (5/20) of units were affected in 2008−2009. Rapid influenza diagnostic tests allowed quick identification with an average time of 1.5 days. In particular, control measures limited the spread of the influenza virus in units with patients not at high risk of complications. On the other hand, antiviral curative treatment and chemoprophylaxis are essential in units with patients at high risk of complications (Fukuta and Muder, 2013; Gaspard et al., 2014; Mada et al., 2018).
5. To prevent worst scenario -- harm reduction strategies for outbreaks in psychiatric hospitals
Based on the above review, the vulnerability of people with mental illness and the knowledge and skills of staff members might easily expose them to epidemics. People with mental illness might also become infected prior to admission, and staff might become infected after working in the community. It is crucial to identify ways to manage people with both COVID-19 and mental illness. Therefore, a contingency plan based on the harm reduction concept should be carefully developed.
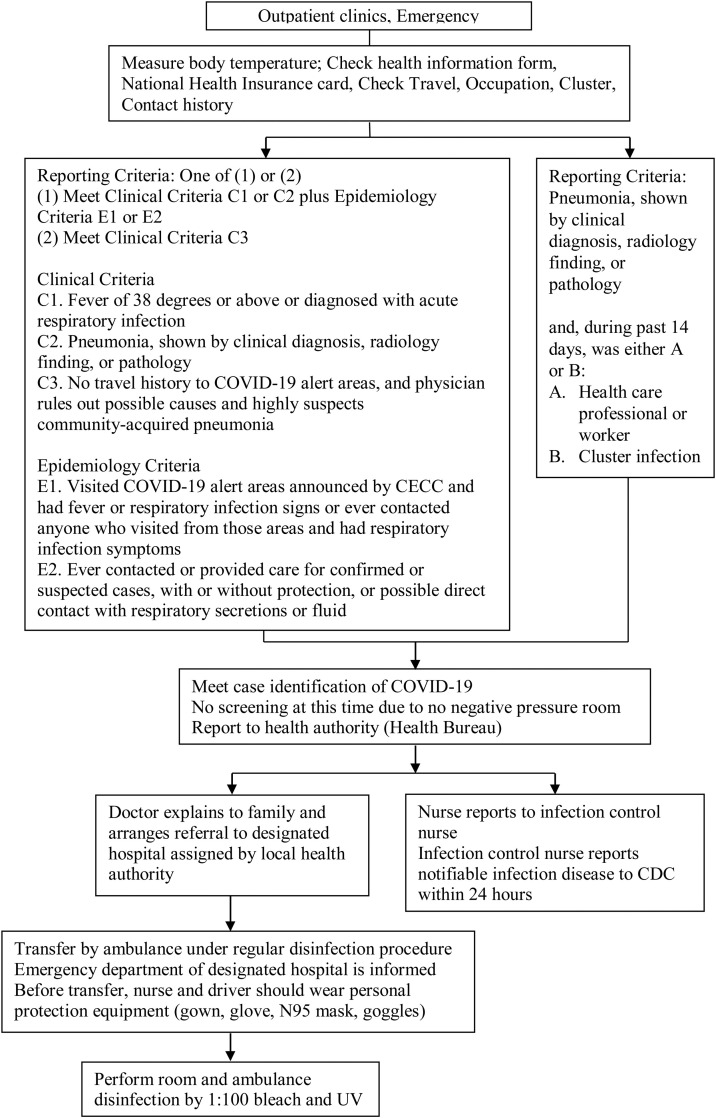
In Taiwan, for the purpose of patient safety, contingency plans according to vulnerability analyses of hospitals are required for hospital accreditation. The scope of contingency plans and standards of operations for infection outbreaks vary due to different pathogens and transmission rates and routes. In the case of COVID-19, because of its highly contagious nature, the extent of operations to prevent infection and reduce harm is enormous. For example, patients coming to the hospital are asked TOCC questions. Most hospitals in Taiwan adopt strict shunting strategies. Every person should be thoroughly classified with the consideration of the possibility of asymptomatic carriers. Every person, including patients as well as care assistants, family members, and staff, should measure their temperature before entrance to the hospital. People with fever are advised to visit designated hospitals. If COVID-19 is suspected in any patient, the medical team should follow a series of steps to report noticeable infectious diseases to the local authorities and CDCs and to arrange transfers appropriately and carefully (Fig. 2 ).
Fig. 2.
Shunting-- Transfer patient with suspected COVID-19 to designated hospital.
If there is a confirmed case in a psychiatric ward, other patients and staff must be quarantined and receive screening tests; however, this creates a shortage of manpower. Part of the contingency plan in our hospital is to encourage social distancing between staff, such as dividing staff into groups based on their serving ward, including offices and on-duty rooms, instead of their profession and utilizing apps for online meetings. By doing so, the routes of staff activities are staggered, thus preventing cross-infection and possibly quarantining together, as in the SARS era. Environmental rearrangement in the hospital is needed. For example, all members of each treatment team are required to provide services only in a single ward and to be separated from other treatment teams as much as possible. Consultant physicians from other general hospitals must wear personal protective equipment to perform history taking and physical examinations. Additionally, space rearrangement can help with surveillance and prevent nosocomial infection. In our hospital, a new patient is isolated in a single room with limited daily activities, such as eating and recreational training, in that room for 5 days and then transferred to another room without a locked door for the next 3 days with patient agreement after staff explanation. After completing 8 days of isolation, they are transferred to rooms without these limitations.
6. Conclusion
Psychiatric hospitals play an important role in supporting patients with mental illness by relieving symptoms and improving functioning in a physically and psychologically safe environment. By learning from previous experiences of SARS and previous studies, psychiatric hospitals can provide safe strategies to prevent patients and staff from infection before and during an epidemic or biological disaster. Even if there is no epidemic, psychiatric hospitals should provide relevant and sufficient pro-service and in-service education and training on infection control, establish regular surveillance of hand hygiene habits, and provide opportunities for vaccination for patients and staff if possible.
During epidemics, psychiatric hospitals should safeguard patients and staff based on the harm reduction concept. These strategies call for rapid responses and actions, including making contingency plans available, reserving adequate support of disinfection equipment, implementing the classification and shunting of patients, and dividing office breaks and manpower to prevent cross-infection. These efforts may minimize the impact and damage of both nosocomial and community-acquired infections and thus may avoid longer-term rehabilitation for the entire hospital.
Financial disclosure
None.
Declaration of Competing Interest
None.
Acknowledgments
The authors appreciate the assistance of the staff at the Kaohsiung Municipal Kai-Syuan Psychiatric Hospital.
References
- Almeida R.C.D., Pedroso R.P. Nosocomial infection in long-term care facilities. A survey in a brazilian psychiatric hospital. Rev. Do Inst. Med. Trop. São Paulo. 1999;41(6):365–370. doi: 10.1590/s0036-46651999000600006. [DOI] [PubMed] [Google Scholar]
- Association for Professionals in Infection Control and Epidemiology . 2020. Infection Prevention and You: Behavioral Health.https://professionals.site.apic.org/settings-of-care/behavioral-health/ Retrieved from. [Google Scholar]
- Banerjee D., Nair V.S. Handling the COVID-19 pandemic: proposing a community based toolkit for psycho-social management and preparedness. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S.-Y. 2020. Strategies of Infection Control for Emergency Deaprtment Facing COVID-19. [Internet]. [updated 2020 March 23; cited 2020 April 12]. https://www.cdc.gov.tw/File/Get/EbADzIybz7nAbc5W7AguLA. [Google Scholar]
- Chen K.-T., Twu S.-J., Chang H.-L., Wu Y.-C., Chen C.-T., Lin T.-H., Su I.-J. SARS in Taiwan: an overview and lessons learned. Int. J. Infect. Dis. 2005;9(2):77–85. doi: 10.1016/j.ijid.2004.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedoriw L.M., Meijer B. Infection prevention strategies in inpatient psychiatric units using patient acuity and motivation. Am. J. Infect. Control. 2013;41(6):S48. doi: 10.1016/j.ajic.2013.03.101. [DOI] [Google Scholar]
- Fukuta Y., Muder R.R. Infections in psychiatric facilities, with an emphasis on outbreaks. Infect. Control Hosp. Epidemiol. 2013;34(1):80–88. doi: 10.1086/668774. [DOI] [PubMed] [Google Scholar]
- Gan N., Thomas N., Culver D. CNN World; 2020. Over 1,700 Frontline Medics Infected With Coronavirus in China, Presenting New Crisis for the Government.https://edition.cnn.com/2020/02/13/asia/coronavirus-health-care-workers-infected-intl-hnk/index.html Retrieved from. [Google Scholar]
- Gaspard P., Mosnier A., Gunther D., Lochert C., Larocca S., Minery P., Talon D. Influenza outbreaks management in a French psychiatric hospital from 2004 to 2012. Gen. Hosp. Psychiatry. 2014;36(1):46–52. doi: 10.1016/j.genhosppsych.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Hiremath P., Suhas Kowshik C.S., Manjunath M., Shettar M. COVID 19: impact of lock-down on mental health and tips to overcome. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavoor A.R. COVID-19 in people with mental illness: challenges and vulnerabilities. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M., Chen C., Yeh C., King C. Severe acute respiratory syndrome-taiwan, 2003. JAMA. 2003;289(22):2930. doi: 10.1001/jama.289.22.2930. [DOI] [PubMed] [Google Scholar]
- Li P.-H., Wang S.-Y., Tan J.-Y., Lee L.-H., Yang C.-I. Infection preventionists’ challenges in psychiatric clinical settings. Am. J. Infect. Control. 2019;47(2):123–127. doi: 10.1016/j.ajic.2018.08.010. [DOI] [PubMed] [Google Scholar]
- Loving P., Porter S., Stuifbergen A., Houfek J., Collins P. Surveillance of nosocomial infection in private psychiatric hospitals: an exploratory study. Am. J. Infect. Control. 1992;20(3):149–155. doi: 10.1016/s0196-6553(05)80182-8. http://er.lib.ncku.edu.tw:2048/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=1636936&lang=zh-tw&site=eds-live Retrieved from. [DOI] [PubMed] [Google Scholar]
- Mada P.K., Saldana D., Castano G., Malus M., Adley S. Influenza outbreaks with a focus on closed psychiatric units: a review article. Global J. Infect. Diseases Clin. Res. 2018;4(1):001–003. [Google Scholar]
- McDonald L.C., Simor A.E., Su I.-J., Maloney S., Ofner M., Chen K.-T., Jernigan D.B. SARS in healthcare facilities, Toronto and Taiwan. Emerg. Infect. Dis. 2004;10(5):777. doi: 10.3201/eid1005.030791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piai-Morais T.H., Fortaleza C.M.C.B., Figueiredo R.Md. Good practices for infection prevention and control at a psychiatric hospital in Brazil. Issues Ment. Health Nurs. 2015;36(7):513–517. doi: 10.3109/01612840.2015.1007539. [DOI] [PubMed] [Google Scholar]
- Santos de Aguiar V., Jr., de Oliveira A.M., Almeida de Araújo L.C. Hygiene and mental health: body care in the clinical intervention in a CAPSI. Revista de Pesquisa: Cuidado e Fundamental. 2015;7(2):2582–2590. doi: 10.9789/2175-5361.2015.v7i2.2582-2590. [DOI] [Google Scholar]
- Shih G., Horton A., Iati M. Coronavirus deaths climb as China corrals sick in quarantine facilities in outbreak epicenter. Washington Post. 2020 https://www.washingtonpost.com/world/asia_pacific/coronavirus-china-updates/2020/02/09/eb9e683c-4aa4-11ea-8a1f-de1597be6cbc_story.html Retrieved from. [Google Scholar]
- Song S.-y. 7 coronavirus deaths at psychiatric ward reveal grim reality. Korea Biomed. Rev. 2020 http://www.koreabiomed.com/news/articleView.html?idxno=7512 Retrieved from. [Google Scholar]
- Taiwan Centers of Disease Control . Taipei Taiwan Centers of Disease Control; 2013. A Decade After SARS : Lessons Learned and Preparedness. [updated 2013; cited 6 March12] Available from: https://www.cdc.gov.tw/File/Get/48woWqOSydNvXDjnQQjn6A. [Google Scholar]
- Taiwan Centers of Disease Control . Taipei Taiwan Centers of Disease Control; 2019. Standards and Audit Procedure of Hospital Infection Control- 2019 Version. [updated 2013; cited 6 March12]. Available from: https://www.cdc.gov.tw/File/Get/ZsHC1EXftPYtz0VZ6TG7nQ. [Google Scholar]
- Taiwan Joint of Commision . Joint Commision of Taiwa; Taiwan: 2019. Accreditation Standards and Measures of Psychiatric Hospitals Taipei. [2019 edition][Internet]. Taipei: Taiwan Joint of Commision. https://www.jct.org.tw/lp-1166-1.html. [Google Scholar]
- Tandon R. The COVID-19 pandemic, personal reflections on editorial responsibility. Asian J. Psychiatr. 2020;50 doi: 10.1016/j.ajp.2020.102100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thibaut B., Dewa L.H., Ramtale S.C., D’Lima D., Adam S., Ashrafian H., Archer S. Patient safety in inpatient mental health settings: a systematic review. BMJ Open. 2019;9(12):e030230. doi: 10.1136/bmjopen-2019-030230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva: 2003. SARS: Status of the Outbreak and Lessons for the Immediate Future. [updated 2003; cited 2020 March 6]. Available from: https://www.who.int/csr/media/sars_wha.pdf?ua=1. [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Outbreak Situation.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Retrieved from. [Google Scholar]