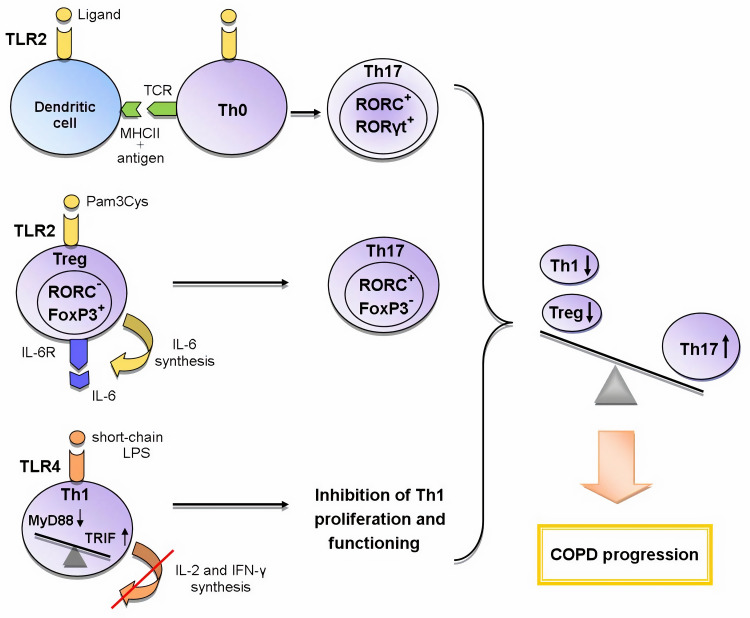
Figure 1.
The role of TLR2 and TLR4 in the formation of Th17 immune response in COPD.
Abbreviations: FoxP3 – forkhead box P3, IL-6 – interleukin-6, IL-6R – IL-6 receptor, MHCII – histocompatibility complex class II, MyD88 – myeloid differentiation primary response gene 88, RORα – retineic-acid-receptor-related orphan nuclear receptor α, RORC – retineic-acid-receptor-related orphan nuclear receptor C, RORγt – retineic-acid-receptor-related orphan nuclear receptor γ, TRIF – toll/interleukin-1 receptor-domain-containing adapter-inducing interferon-β, TCR – T cell receptor, Th0 – naive T helper cell, Th1 – T helper cell type 1, Th17 – T helper cell type 17, Treg – T regulatory cell, TLR – toll-like receptor
Legend: Recently three mechanisms of the influence of TLRs on the formation of T-helper immune response in COPD are proposed: 1) the activation of TLR2 signaling in dendritic cells during the presentation of antigen to Th0 cells enhances the expression of RORγt, RORC (Th17-associated transcription factors) and thus contributes to the differentiation of Th17 cells; 2) TLR2 signaling in Tregs initiates the synthesis of IL-6; IL-6, acting in an autocrine manner, inhibits the expression of FoxP3 responsible for the suppressive activity and initiates the expression of RORC in these cells; as a result, the polarization of Tregs towards Th17 cells occurs; 3) the switching from the TLR4/MyD88-dependent pathway to the TLR4/TRIF-dependent pathway in Th1 cells leads to a decrease in synthesis of IL-2 and IFN-γ and the inhibition of IL-2-mediated proliferation of these cells. Thus, the activation of these mechanisms causes an imbalance between T-helper subpopulations towards Th17 cells, which leads to COPD progression.