Abstract
Many governments have instructed the population to wear simple mouth-and-nose covers or surgical face masks to protect themselves from droplet infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in public. However, the basic protection mechanisms and benefits of these masks remain controversial. Therefore, the aim of this work is to show from a fluid physics point of view under which circumstances these masks can protect against droplet infection. First of all, we show that the masks protect people in the surrounding area quite well, since the flow resistance of the face masks effectively prevents the spread of exhaled air, e.g. when breathing, speaking, singing, coughing and sneezing. Secondly, we provide visual evidence that typical household materials used by the population to make masks do not provide highly efficient protection against respirable particles and droplets with a diameter of 0.3–2 μm as they pass through the materials largely unfiltered. According to our tests, only vacuum cleaner bags with fine dust filters show a comparable or even better filtering effect than commercial particle filtering FFP2/N95/KN95 half masks. Thirdly, we show that even simple mouth-and-nose covers made of good filter material cannot reliably protect against droplet infection in contaminated ambient air, since most of the air flows through gaps at the edge of the masks. Only a close-fitting, particle-filtering respirator offers good self-protection against droplet infection. Nevertheless, wearing simple homemade or surgical face masks in public is highly recommended if no particle filtrating respiratory mask is available. Firstly, because they protect against habitual contact of the face with the hands and thus serve as self-protection against contact infection. Secondly, because the flow resistance of the masks ensures that the air remains close to the head when breathing, speaking, singing, coughing and sneezing, thus protecting other people if they have sufficient distance from each other. However, if the distance rules cannot be observed and the risk of inhalation-based infection becomes high because many people in the vicinity are infectious and the air exchange rate is small, improved filtration efficiency masks are needed, to take full advantage of the three fundamental protective mechanisms these masks provide.
Highlights
-
•
A simple mouth-and-nose cover or a surgical mask is able to effectively limit the spread of air and aerosol.
-
•
Wearing a mask is very useful to contain a pandemic by protecting people in the vicinity from droplet infection.
-
•
A mouth-and-nose cover or a surgical mask does not fit tightly enough on the face to protect against droplet infection.
-
•
Only a particle-filtering half-mask that fits tightly offers protection against droplet infection.
-
•
Common household materials, however, do not have a sufficient filter effect to protect against droplet infection.
1. Introduction
At present, humanity is threatened by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. The risk of severe infection with the virus depends heavily on physical factors of the infected persons and the quality of the medical system. According to a recent study the estimated infection fatality ratio (IFR), averaged over all age-groups including those who don't have symptoms, is between 0.2% and 1.6% with an average of 0.66% (Verity et al., 2020). These numbers look small, and the fatality risk may seem acceptable, and therefore the danger is often marginalized. This is surprising considering that the Apollo crew, the space shuttle astronauts and the Allied soldiers during the 2003 Iraq war took a deadly risk of this magnitude. Only very few people take such risks voluntarily and with full consciousness. For comparison, the lethal risk of a fatal accident with a commercial aircraft was 1:7700000 in 2008 and even such a small risk is not taken by some people. Considering that the IFR of the seasonal flu is about 0.04–0.1% (Centers for Disease, 2010) or even much lower (Wong et al., 2013) the mortality rate of SARS-CoV-2 appears to be significantly higher than for influenza flu. Although the numbers for SARS-CoV-2 are quite preliminary and the estimates may drop over time (Verity et al., 2020, Faust & del Rio, 2020) it is quite clear that the strategy of herd immunization of the population is not an option, as the number of victims would be far too high. Great hopes for coping with the pandemic currently rest on the development of a vaccine. Unfortunately, it is completely uncertain when an effective and well-tolerated vaccine will be generally available to contain the pandemic. Drugs such as Chloroquine, Remdesivir, Lopinavir and Ritonavir are also considered to be great sources of hope in the fight against the coronavirus disease 2019 (COVID-19) (Grein at al., 2020). However, even if one of the drugs should prove to be effective, there is no guarantee that the drug can be made available to the world population in sufficient quantities. In addition, it is possible that, despite the use of drugs, going through a severe course of disease can lead to lifelong neuropsychiatric sequelae (Troyer, Kohn, & Hong, 2020; Zandifar & Badrfam, 2020) or cause other diseases (Ackermann et al., 2020; Varga et al., 2020).
Containing the pandemic is therefore the only viable way to quench the spread of the virus. But containing the pandemic is a difficult task as about 44% of SARS-CoV-2 infections are caused by people with a presymptomatic and asymptomatic course of infection (He et al., 2020). Therefore, due to the absence of symptoms, many people do not know that they are infected and are spreading the virus and these people make it very difficult to trace the transmission chains. Furthermore, about 10% of infected people are responsible for 80% of infections (Kupferschmidt, 2020; Lloyd-Smith et al., 2005). People who have many social contacts at work or in their private lives and who do not protect themselves and others sufficiently by observing the rules of distance and hygiene, or who consider the risk of the virus to be low, appear to be a serious problem in the actual pandemic. For these reasons, the government must act at various levels to avert great harm to the population. The effectiveness of the containment strategy depends on:
-
1.
How societies are able to protect themselves personally against infection through hygiene, social distance and technical aids such as protective masks, glasses, gloves.
-
2.
How well the infrastructure is in place to identify the infection chains and effectively contain the spread, e.g. through mobile data collection, isolation or a lockdown.
-
3.
How well the seriously ill can be treated in hospitals.
In view of these prospects, it seems necessary for the time being to prevent the spread of the virus and to treat those infected as well as possible. In order to ensure the latter, the capacities of the health system must not be overloaded. But it is clear that this condition means that the pandemic will last for years without a vaccine1 . To not overload the medical systems, governments are pursuing the concept of containment by means of a lockdown because it proved successful in St. Louis during the Spanish Flu of 1918. This approach is quite effective when the population obeys the rules, but the impact on the state, economy and society is devastating when the lockdown lasts longer than a few weeks. Therefore, this concept is not a viable way to contain the pandemic in the long term. Consequently, it is necessary to fight the infection where it occurs.
Understanding the transmission pathways is the key to finding effective measures to block the infection and to reliably protect healthcare workers and the population. Contact infection were initially assumed to be the main transmission route of SARS-CoV-2. Today, hygiene measures and the avoidance of shaking hands effectively prevent this path of infection. Droplet infection is currently assumed to be the main transmission route over short distances (Wang et al., 2020). Since this path of infection is via the air, the rules of distance are effective (Soper, 1919 and Wells et al., 1936). But it is also known that SARS-CoV-2 can remain infectious in aerosols for more than 3 h, at least under laboratory conditions at high humidity (van Doremalen et al., 2020 and Pyankov et al., 2018). It is therefore conceivable that infections can also occur under special conditions over long distances, provided that the local virus concentration reaches the minimum infection dose due to poor air exchange in rooms.
A significant proportion of the aerosol exhaled by humans has a diameter of less than 10 μm (Johnson et al., 2011) when breathing, speaking, singing and coughing. It is also known that the size and number of droplets increases with the volume of the voice (Asadi et al., 2019; Loudon & Roberts, 1968) and it is known that upper respiratory tract diseases increase the production of aerosol particles (Lee et al., 2019). Water droplets of this size evaporate within a few seconds at normal humidity (Liu et al. 2019 and Rensink, 2004). Droplets with a diameter of 10 μm for instance are evaporated after about 1 s at 50% relative humidity and larger droplets sink quickly to the ground and evaporate (Marin et al., 2016, 2019; Rossi et al., 2019). If the viruses are released as “naked” viruses together with the salt after the droplets have evaporated, the spatial concentration decreases rapidly over time, as the viruses no longer move in a correlated manner but quickly separate due to the chaotic turbulent flow motion. The viral load thus decreases rapidly in time and space, making infections over long distances or long periods of time increasingly unlikely. For this reason it is most important to understand the transmission of the virus over short distances.
Hygiene regulations and social distancing are very effective in blocking short distance infections. During the lockdown, the distance rules can usually be adhered to, but what happens when the actual lockdown is over and the people meet again in confined spaces? Then additional effective and efficient protection is essential to stabilise infection rates. Since the viruses are spread by contact and droplet infection, technical devices are required that effectively intervene in the chain of infection and effectively block infection. An effective protection is the respiratory mask as known since 100 years (Soper, 1919). The SARS outbreak in Hong Kong suggested that the use of simple face masks may have contributed to an overall reduction in the incidence of viral respiratory infections (Leung et al., 2003; Lo et al., 2005). Another study has shown that even a simple surgical mask can effectively reduce SARS infection (Seto et al., 2003). These results are supported by recent articles Leung et al., 2020b, Howard et al., 2020, Chu et al., 2020 and Zhang, Lib, Zhang, Wang, & Molina, 2020).
It was surprizing that for months, WHO, the CDC and many public health professionals in Europe advised against wearing face masks unless someone has COVID-19 or cares for someone who has COVID-19 (Feng et al., 2020; Leung et al., 2020a). This recommendation was based on three allegations. First, it was said that there is no scientific evidence that face masks can protect against droplet/aerosol infections. Second, it was argued that the population will not be able to wear the masks properly. Third, the statement that people will feel safe when wearing masks and then become careless and take risks was frequently made. At the same time, these experts have stressed that health professionals urgently need face masks to protect themselves effectively. This contradiction has created uncertainty among the population and called into question the credibility of the experts. It is a fact that particle filtration masks are recognized as legal occupational safety equipment and that the wearing of these masks in contaminated areas is required by labor law. There is therefore no doubt that these masks, when used correctly, provide effective protection within the specification range. The effectiveness of simple mouth-and-nose covers and surgical masks is less well accepted. The International Council of Nurses (ICN) estimates that, on average, 7% of all confirmed cases of COVID-19 are among healthcare workers (ICN, 2020). This illustrates that surgical masks may not provide the reliable protection against droplet infection, as anticipated. It is therefore very important to distinguish clearly between the different mask types when talking about their protective function. Unfortunately, this was not done sufficiently by the virologists and politically responsible persons in the initial phase of the pandemic. Also the second argument is questionable. Why should the people of Western societies not be able to protect themselves as many people in East Asian countries have long been doing? Many people in East Asian countries have already recognized through numerous pandemics that proper masks work effectively. It does not seem right to regard the Western population as unteachable or even incapable. The third argument is also false, because the opposite is true according to scientific studies (Prather, Wang, & Schooley, 2020; Scott et al., 2007 and Ruedl et al., 2012). If people protect themselves personally, they have dealt with the danger and therefore they benefit from the protection of the safety device and from the less risky behaviour due to insight. The reason why these facts were not appreciated by the experts is due to the attempt to prevent competition for protective masks between medical personnel and the public.
In the meantime, the general perception of the protective effect of face masks has become generally accepted. In the USA, the CDC has changed its guidelines and recommended that the public wear fabric face masks. In other countries, too, it is now recommended to protect themselves with suitable masks. However, it is recommended by governments and professionals to wear only simple mouth-and-nose covers that can be manufactured by the people themselves or surgical masks to avoid distribution battles with medical staff for certified and comfortable particle filtration masks. But the big question is, how effectively these homemade mouth-and-nose covers and surgical masks can protect against droplet infection. The answer is highly relevant to guide public behaviour (Leung et al., 2020). One study suggests that a surgical face mask and masks made of dense cotton fabrics apparently cannot effectively prevent the spread of SARS-CoV-2 into the environment through the coughing of patients with COVID-19 (Bae et al., 2020; Klompas, Morris, Sinclair, Pearson, & Shenoy, 2020). Another study suggests that any mask, no matter how efficiently it filters or how well it is sealed, has minimal effect unless used in conjunction with other preventive measures such as isolation of infected cases, immunization, good respiratory etiquette and regular hand hygiene (Kwok et al., 2015). These findings contradict the results in (Leung et al., 2003; Lo et al., 2005; Seto et al., 2003). Due to the contradiction, it is understandable that experts in the media have expressed the opinion that there is no scientific evidence for the effectiveness of masks and therefore the wearing of masks in public was not recommended for a long time. The fallacy of politicians and virologists, however, was to generalize the results obtained with simple mouth-and-nose covers to all masks without differentiation.
In order to clarify whether or to what extent these masks offer effective protection against droplet infection and to understand why research results differ on this simple scientific question, we have carried out these tests. First, we analyse the flow blockage caused by surgical masks when coughing, as this is essential for the protection of others and because coughing is a typical symptom of COVID-19. Second, we qualify the effectiveness of different filter materials and masks to determine the protection ability against droplets. Finally, we prove the effect of gap flows at the edge of surgical and particle filtrating respiratory masks. In contrast to the medical studies cited, we apply engineering research methods of fluid mechanics. The use of this research approach has several reasons: Firstly, the detachment of droplets in the lungs and throat and their convective transport through the mouth into the atmosphere until inhalation as well as the deposit and evaporation of droplets is a purely fluid mechanical process. Secondly, the effective blocking of the flow with suitable masks is a research subject of fluid mechanics. Thirdly, the filtering of particles from an air stream with the aid of suitable materials is also a purely fluid mechanical problem as well as the gap flow. Finally, this approach also has the advantage that the results are reproducible in a statistical sense, since the boundary conditions are well defined. We are not studying whether an infection really occurs in a special case, but whether an infection is physically possible in general.
2. Materials and methods
In the first sets of the experiments, outlined in section 3.1, the flow field generated by coughing without and with a surgical mask is examined as coughing sets the air strongly in motion and because coughing is a typical symptom of COVID-19. To measure the flow field quantitatively in space and time we use Particle Image Velocimetry (PIV) (Raffel et al., 2018). For the measurements a 8 m long testing room with a cross section of 2 m × 2 m was seeded with DEHS (Di-Ethyl-Hexyl-Sebacate) tracer particles with a mean diameter of 1 μm (Kähler et al., 2002). DEHS was used as these droplets exist for several hours until they have evaporated. The tracer particles provided by a seeding generator (PIVTEC GmbH, Germany) were illuminated in a light-sheet generated with a frequency doubled Nd:YAG laser (SpitLight PIV 1000–15, InnoLas Laser GmbH, Germany). The light-sheet was oriented normal to the mouth opening and parallel to the symmetry axis of the body and the longitudinal axis of the room. The light scattered by the tracer particles were recorded with back illuminated scientific CMOS cameras (pco.edge 5.5, PCO AG, Germany) equipped with Zeiss Distagon T* lens with a focal length of 35 mm and 50 mm. The triggering of the system components was achieved with a programmable timing unit (PTU X, LaVision GmbH, Germany). The recorded series of images were evaluated with a commercial computer program (DaVis, LaVision GmbH, Germany). These quantitative PIV measurements allow to determine the area that can be contaminated due to the exhaled air, the velocity of the exhaled droplets and the turbulence properties of the flow.
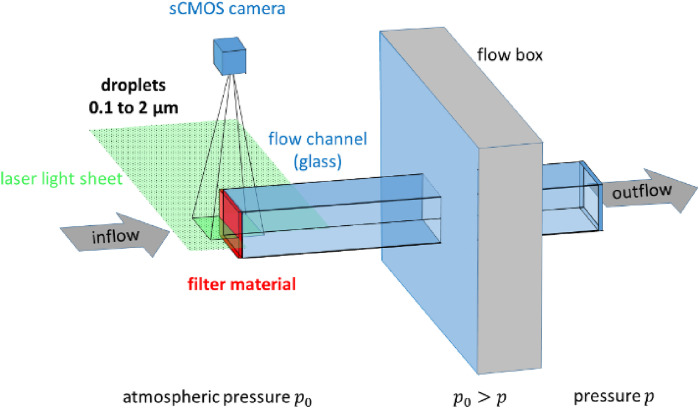
In the second set of experiments, discussed in section 3.2, common household materials currently used by the population and some medical staff to make simple masks at home were tested but also a surgical mask and a FFP3 mask to visualize their filtering properties. The tested materials are given in Table 1 . For the investigation, a test set-up was installed which largely fulfilled the officially prescribed test conditions in Europe (DIN EN 149, 2009). The materials were installed one after the other in a fixed position in front of the inlet of a rectangular flow channel with a cross-section of 0.1 m × 0.1 m, as shown in Fig. 1 . The material was held in place with a special clamping device that seals tightly to the duct to avoid leakage flows. To explore the filtering performance of the different materials the movement of small aerosol droplets passing through the media was observed visually in front of and behind the filter material with a digital camera. We only use droplets whose diameter is less than 2 μm, since the removal of the smallest droplets in an air stream is the greatest challenge in mask development. If these droplets can be effectively filtered out effectively, then all droplets larger than 2 μm can also be filtered. The droplets were generated from DEHS with an aerosol generator (AGF 2.0, Palas GmbH, Germany). DEHS was used again as these droplets are long lasting. Consequently, bias errors due to evaporation effects can be neglected. A Nd:YAG double-pulse laser (Evergreen 200, Quantel, France) was used to illuminate the droplets. The output beam was fanned out with a few lenses to form a 1 mm thin light-sheet. The light-sheet was located in the middle of the flow channel parallel to the flow direction as indicated in Fig. 1.
Table 1.
Tested filter materials.
| Material | Surgical face mask | Hygienic mask | Toilet paper | Paper towel | Coffee filter |
|---|---|---|---|---|---|
| Pressure drop at 60 l/min [mbar] | 0.2 | a | 0.3 | 0.3 | 1.8 |
| Pressure drop at 90 l/min [mbar] | 0.4 | a | 0.6 | 0.7 | 4.0 |
|
| |||||
|
Material |
Microfibre cloth |
Fleece |
Vacuum cleaner bag |
FFP3 mask with valve |
Halyard H600 |
| Pressure drop at 60 l/min [mbar] | 7.7 | 0.1 | 2.0 | b | 1.4 |
| Pressure drop at 90 l/min [mbar] | 17.2 | 0.2 | 4.5 | b | 3.1 |
Not measured.
Not available. Due to the valve and the resulting inhomogeneous flow field, the volume flow rate could not be determined with the method applied.
Fig. 1.
Schematic representation of the experimental setup.
The scattered light emitted by the illuminated aerosol in the light-sheet plane was recorded with a highly sensitive PCO edge 5.5 sCMOS camera equipped with a Zeiss Distagon T* lens with a focal length of 50 mm. The triggering of the system components and the data recording was realized again with the software DaVis from LaVision. The flow velocity was driven by the pressure difference between the atmosphere and the flow box. The flow rate through the filter material was adjusted approximately according to the DIN EN 149, 2009 test standard (90 L/min). The volume flow rate and the movement of the droplets through the filter material was measured optically with high spatial and temporal resolution using PIV. To calculate the volume flow rate the average flow velocity within the light-sheet plane in the flow channel was measured and it was assumed that this velocity is homogeneous over the cross section of the channel. This assumption is justified as the filtering materials are homogeneous and the inflow condition is constant across the filtering material. With the know size of the cross section the volume flow rate can be calculated. The pressure drops provided in Table 1 are calculated from the measured pressure drops and the volume flow rate. It is assumed that the pressure loss is proportional to the square of the volume flow rate. The pressure drop across the filter material was measured with a pressure transducer with an uncertainty of about 3 Pa (TESTO 480, Testo SE & Co. KG, Germany).
For the third set of experiments, analysed in section 3.3, simple flow visualizations using smoke were performed in order to demonstrate the effect of the gap around the mask edge. A person exhaled air seeded with tracer particles while wearing surgical and FFP2 masks.
3. Results
3.1. The effect of flow resistance (protection of others)
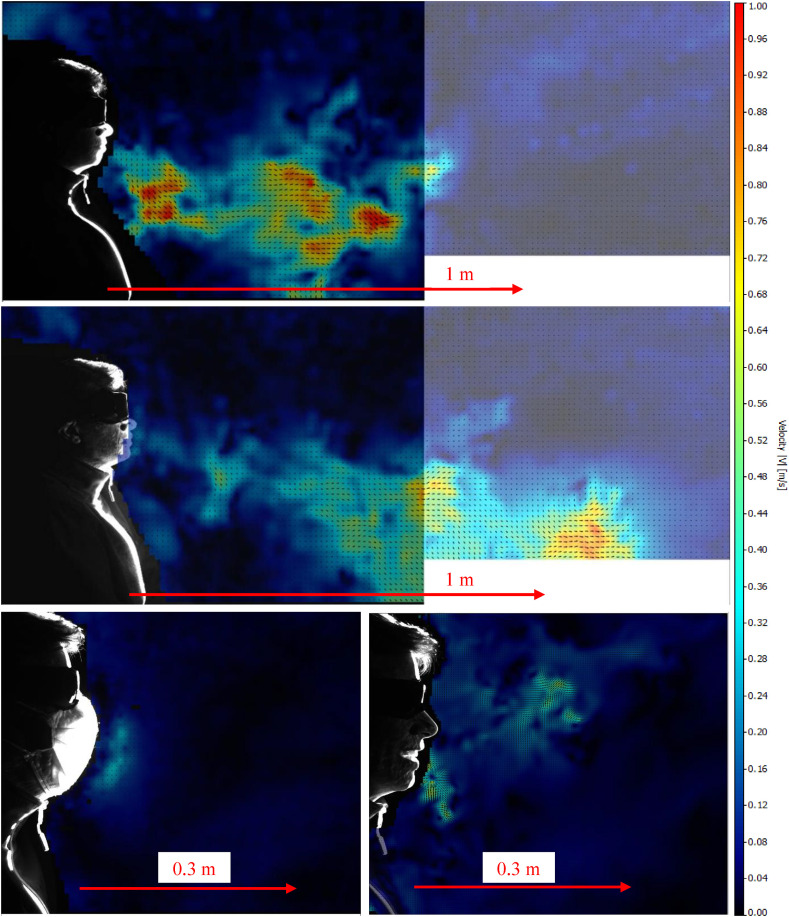
In the first series of experiments, one person performed a single severe cough while the PIV system was measuring the flow field data. The video in the supplementary material shows the temporal evolution of the process. The results displayed in this subsection show instantaneous velocity fields of various independent time-resolved flow field measurements. Color-coded is the magnitude of the local flow velocity and the vectors indicate the direction of the flow movement at a given time step. In areas where the flow movement remains close to zero over the whole recording time (blue color), no droplets can penetrate as only the flow can move the particles to other areas. Large droplets with a diameter of 1 mm or more, such as those produced when sneezing (Lok, 2016), can fly ballistic over long distances, and occasionally ballistic flying droplets are produced when certain sounds are spoken. But sneezing is not a typical COVID-10 symptom so that this will not we considered here. The small droplets that are normally produced when breathing, speaking, singing and coughing are immediately slowed down and then move with the flow velocity of the ambient air. It is therefore important to study the air set in motion by exhalation. Furthermore, the small droplets are particularly dangerous because they can be inhaled deep into the lungs.
Fig. 2 a shows that the spread of the exhaled air forms a cone like shape similar to a free turbulent jet (see video). The flow velocity is reaching values up to 1 m/s near the mouth, but due to the widening of the cone caused by the turbulent mixing and entrainment (Reuther & Kähler, 2020) the flow velocity decreases in streamwise direction. The widening of the area in motion reduces the viral load significantly with distance. A single strong cough sets the air in motion over a distance of less than 1.5 m in the experiments. Distances of more than 1.5 m can be considered safe according to these results, since no droplets can reach such large distances when accelerated by a single cough. However, if the cough lasts longer, greater distances can be achieved, as shown in Fig. 2b. For this reason, it is important to dynamically increase the distance to a person if the coughing stimulus is about to last longer.
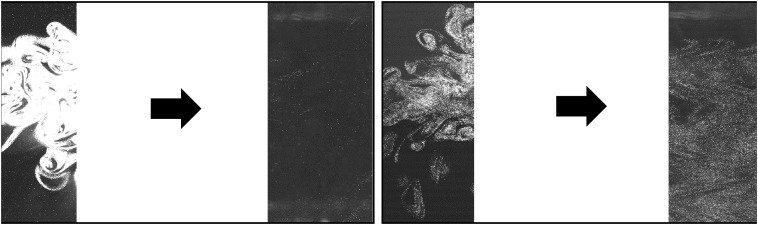
Fig. 2.
Instantaneous flow field when coughing over one breath without mask (a, top). Flow field when coughing over a longer periods of time without mask (b, middle). Flow field when coughing over one breath with mask (c, lower left) and instantaneous flow field when talking without mask (d, lower right). The first video in the supplementary material shows the animated sequences.
The results in Fig. 2c illustrate how the spread of the airflow from the mouth during coughing is very effectively inhibited by a surgical mask. Physically the mask ensures that the directional jet like air movement with high exit velocity from the mouth is converted into an undirected air movement with low velocity behind the mask. This is because the exhaled air increases the pressure inside the mask compared to the atmosphere outside, and the pressure difference creates a flow movement in all directions. This effect is of utmost importance for limiting the virus load in the environment. The results show that even a simple mouth-and-nose cover or a surgical mask can effectively protect other people in the vicinity because the mask prevents the droplets from spreading over a wide area. A simple mask with sufficient flow resistance therefore provides very effective protection for people in the surrounding area when infected and wearing the mask. Wearing a mask is therefore absolutely useful to protect others according to our quantitative measurements.
Fig. 2d shows the spread of exhaled air when speaking. It can be clearly seen that a greater spread of the exhaled air appears than when coughing with a mask. Consequently, wearing a mask during normal face-to-face conversations and of course also when talking on the smartphone in a human environment is extremely useful to stop the transmission of the SARS-CoV-2 infection via droplets. It must also be taken into account that persons with a presymptomatic or asymptomatic course of infection will infect other persons most likely during face-to-face conversations. A mask will therefore make an effective contribution to suppressing this significant path of infection.
3.2. The effect of aerosol filtration (self protection)
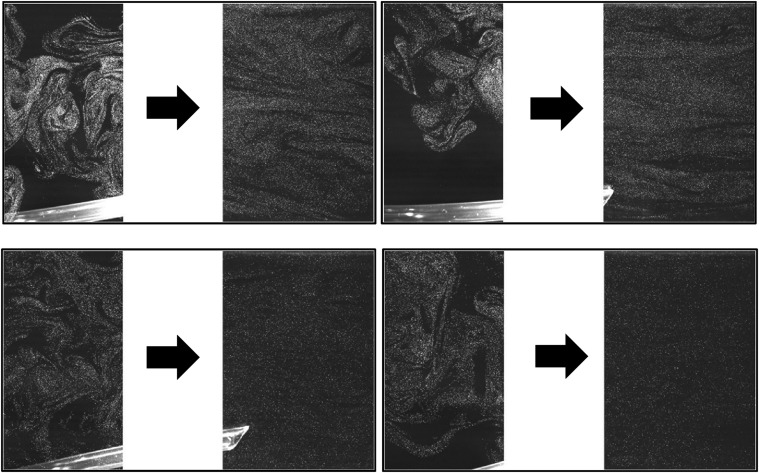
In this section we want to find out if the material of simple mouth-and-nose covers, surgical masks and FFP3 masks can protect the user from droplet infection, if the surrounding air is contaminated with SARS-CoV-2. In this case, the mask material must have good filtering properties to stop small droplets that typically occur when speaking, singing and coughing. Since large droplets are easily filtered out by simple materials, we focus on small droplets in the range between 0.3 and 2 μm because they are produced in large fractions when speaking, singing and coughing and they can penetrate deep into the lungs. The droplets were distributed approx. 400 mm in front of the filter materials. In order to make the motion of the droplets and the filtering ability of the materials clearly visible an inhomogeneous droplet distribution was generated. The flow direction is from left to right and the flow state of the incoming air is laminar. If the intensity of the scattered light emanating from the droplets is large in front of the filter material (left image) and close to zero behind the filter material (right image), the droplets are almost completely filtered out through the material. If, on the other hand, no significant reduction in intensity can be detected behind the filter material, the filter effect is negligible. The area of the filter mount and the channel edges are not shown in the following images, since no relevant flow and droplet information is visible in these areas. The results presented are qualitative, but intended to be this way to provide readers with visual evidence of the particle penetration through different candidate filter media. A better impression of the filter efficiency is obtained by viewing the second video in the supplementary material.
The comparison of the two pictures in Fig. 3 (left) shows that almost all droplets pass the tested surgical face mask unhindered. Consequently, this mask does not provide serious self protection against droplet infection. Only a mixing of the droplet distribution takes place due to the porosity of the filter material. It is fatal that medical personnel are often so poorly protected by these masks. But it is also fatal for patients if clinical staff with a presymptomatic or asymptomatic course of infection uses these masks.
Fig. 3.
Effectiveness of particle filtering with the filter material of a surgical face masks (left) and a hygienic mask (right). The arrow indicates the flow direction and filter position. The second video in the supplementary material shows the animated sequences.
Even worse than the surgical face masks is the hygiene mask, see Fig. 3 (right). This mask is designed for catching larger objects such as hair and spook, but tiny droplets, such as those produced when talking, singing and coughing, cannot be filtered out of the air stream by the hygiene mask. It should also be noted that the flow resistance of the hygiene mask is so low that even the protective mechanism described in subsection 3.1 does not function effectively. Fig. 4 reveals the effectiveness of particle filtering with toilet paper with 4 layers, paper towel, coffee filters, and microfibre cloth which also offer no serious protection against droplets in this size range. Only very large droplets are retained by these materials and therefore these materials are suitable for their intended use, but not as filter material for small droplets. It is therefore strongly discouraged to make masks from these materials with the aim of protecting oneself from infection.
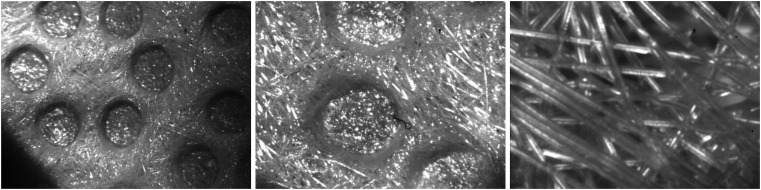
Fig. 4.
Effectiveness of particle filtration. Toilet paper (upper left), paper towel (upper right), coffee filter (lower left), microfibre cloth (lower right). The second video in the supplementary material shows the animated sequences.
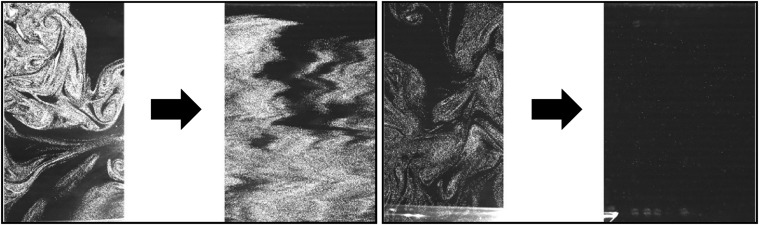
Furthermore, a very strong fleece was tested, which serves as a protective coating on ironing boards. The material is 4 mm thick, completely opaque and has a pressure drop of about 35 Pa. However, a filter effect is not visible, as indicated in Fig. 5 (left). The droplet clouds flow almost unfiltered through the fleece. Even several layers of a dense fabric do not have a proper filtering effect on the considered droplet sizes, which escape mainly when breathing, speaking, singing and coughing.
Fig. 5.
Effectiveness of particle filtration of a fleece (left) and vacuum cleaner bag with fine dust filter (right). The second video in the supplementary material shows the animated sequences.
Good results could only be achieved with the material of a vacuum cleaner bag with fine dust filter properties, see Fig. 5 (right). Despite the small droplets used in these tests, almost all droplets are reliably filtered out. Consequently, also no larger droplets will be able to pass through the material. According to the manufacturer SWIRL, the material filters 99.9% of fine dust down to 0.3 μm diameter. This vacuum cleaner bag with fine dust filter therefore has better filtering properties than all tested materials and masks and even an FFP2 protective mask has poorer filtering properties, as it only has to filter out 94% of the fine dust down to 0.6 μm to meet the specifications (Uvex, 2020). The material of vacuum cleaner bags with fine dust protection is therefore very well suited as a self-protecting mask if only the filter effect is considered. However, because vacuum cleaner bags are not certified clinical products, they may contain unhealthy ingredients that kill bacteria and harmful fibers that may leak from the bag material. It is therefore uncertain whether this material is suitable in practice as a material for a respirator mask.
Fig. 6 (left) illustrates the filtering capabilities of an FFP3 mask under the test conditions. Nearly all droplets are filtered out as expected. Therefore, this mask type is very well suited to protect people from an infection by means of aerosols even when the environment is strongly contaminated with infectious droplets. Recently, some hospitals in the USA make use of Halyard H600 material to protect their employers from aerosol infection. The test result of the material is displayed in Fig. 6 (right). It is clearly visible that the filtering capacity of the material is not sufficient to protect people from infection by aerosols if the environment is contaminated with the SARS-CoV-2. Fig. 7 shows with different resolution microscopic images of the Halyard H600 material. It is composed to fibers but the density might not be sufficient to filter the particles used in our investigation. There are also tiny holes in the pockets visible, which could be the reason why the aerosol passes through the material, as the flow resistance at the holes is low compared to the other parts of the material.
Fig. 6.
Effectiveness of a FFP3 mask (left) and Halyard H600 material (right). The second video in the supplementary material shows the animated sequences.
Fig. 7.
Microscopic images of the Halyard H600 material with different resolution.
The flow tests clearly show that apart from the vacuum cleaner bag and the FFP3 mask, the filter effect of the tested materials is not sufficient to protect against droplet infection reliably if the environment is contaminated with SARS-CoV-2. Even masks routinely used by medical staff in hospitals and doctor's offices have almost no significant filtering effect on the droplet sizes typically produced when breathing, speaking, singing and coughing. The results are therefore in good agreement with the results from (Leung et al., 2020 and Davies et al., 2013 and Kwok et al., 2015. But why has wearing these masks been shown to provide effective protection against infection with the virus in the SARS epidemic, as shown in (Leung et al., 2003, Lo et al., 2005 and Seto et al., 2003)? Because a mask is important not only because of its filtering ability, but to limit the droplet propagation as discussed in section 3.1. So in combination with distances these mask can protect if only a few people are infected in the surrounding. The results in (Bae et al., 2020; Leung et al., 2020) are correct, but they do not consider the full performance of masks, but only a partial aspect. Therefore, the conclusions in the articles are not universal. The findings in (Leung et al., 2003; Lo et al., 2005; Seto et al., 2003) are understandable when the full performance of masks in blocking infections is considered.
Unfortunately, wearing a simple mouth-and-nose cover may be less comfortable than wearing a particle filtering face mask. In effect, this can promote a smear infection. Since all these transmissions of infection are possible in daily life, wearing a comfortable mask is essential to block human-to-human transmission by smear and droplet infection. To ensure the best possible protection, a particle filtering mask should be used if the number of infected persons in the environment and the viral load in the room is unknown. At present, social distancing practices and universal masking seem to be the best methods of containing viral pandemic without stricter lockdown policies and without vaccines.
Some recent studies show that even the simple materials we have tested have some filtering ability (Davies et al., 2013; Drewnick, 2020; Konda et al., 2020 and van der Sande et al., 2008), We do not question these results, although the pressure drops in one study is anomalously low (see supporting information in Konda et al., 2020), but we state explicitly that a material that does not have an adequate filtering ability equivalent to an FFP2/N95/KN95 mask cannot be recommended as a filter material for self-protection against droplet infection. Statistically speaking, every loss of performance leads to an increase in the number of infected people and thus to an increase in the number of death. It is therefore very dangerous to recommend materials with some filtering properties as possible materials for self-protection masks. But there is another important aspect that will be discussed next.
3.3. The effect of gap flows on the mask performance
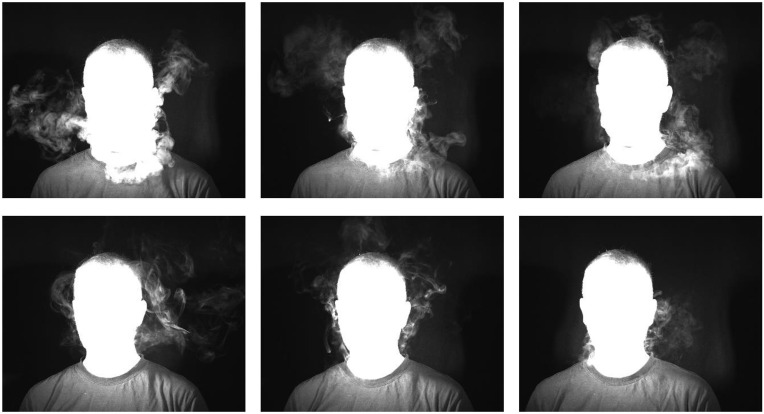
According to the previous section one might argue that a mouth-and-nose cover or surgical mask made of a good filter material would provide good protection against infection when infected people are in the vicinity or the room is contaminated with viruses. But that will not usually be the case. Air takes the path of least resistance. As these masks do not seal tightly enough with the face, droplets can flow unhindered past the edge of the mask when inhaled and exhaled and reach the lungs or the environment. If the mask does not fit properly, this will even be the rule. This is illustrated in Fig. 8 were a person is exhaling air during an easy exhalation without physical exertion (left), strong breathing during physical exertion (middle) and when coughing (right). The first video in the supplementary material shows the animated sequences.
Fig. 8.
Exhalation of air during light exhalation without physical exertion (left), heavy breathing comparable to physical exertion (middle) and when coughing (right). Top row: Surgical mask. Lower row: Very simple FFP2 mask without exhalation valve. The first video in the supplementary material shows the animated sequences.
4. Summary and conclusion
The analysis shows that it is very important do differentiate between mouth-and-nose cover, surgical mask and particle filtering respirator mask because they differ substantial in their fundamental protection properties. Face masks can offer three fundamental different kind of protection:
-
1.
They effectively prevents a smear infection, as the wearers of the masks no longer perform their habitual grip on the face and thus no longer bring the virus from the hand into the mouth or nose (Howard et al., 2020).
-
2.
The flow resistance of the mask greatly limits the spread of viruses in the room. This significantly reduces the risk of infection in the vicinity of an infected person (protection of third parties).
-
3.
The inhalation of droplets containing viruses can be prevented by using a tight-fitting mask with particle filtering properties (self-protection).
The first fundamental protection mechanism can be reached by all face masks if they fit well and sit comfortably. If not, the user will touch the face even more than usual to correct the fit of the mask. As this can increase the risk of smear infection, a good fit of the mask is very important. The first and second fundamental protection mechanisms are fulfilled by all masks that have sufficient flow resistance. If the mask is worn and a candle can easily be blown out despite the mask, the mask does not fulfil this function and should not be used. All three fundamental protection mechanisms can be only achieved with FFP2/N95/KN95 or better particle filtering respirator mask.
Typical materials currently used by the public to build masks reduce the risk of smear infection and effectively prevent the widespread spread of viruses in the environment. Therefore, the use of these mouth-and-nose covers and surgical masks are very important to prevent smear infection and droplet infection to others if the distance is not too close. As these masks do not have a significant particle-filtering protective effect against droplets that are typically produced when breathing, speaking, singing, coughing and sneezing they should not be used if the environment is contaminated, like in hospitals, even when the distance rules are followed. To achieve effective self-protection in a virus-contaminated environment, masks with particle filtering properties (FFP2/N95/KN95) are absolutely necessary from our point of view. If a large number of infected persons are present and distance rules cannot be achieved, a very good particle filtration mask (FFP3 or better) is strongly recommended.
If these general rules are followed and all people use suitable particle-filtering respirators correctly, the transmission of viruses via droplets/aerosols can be effectively prevented. Otherwise, these types of masks would never have received certification, nor would they be a core component of the personal protective equipment in hospitals and other environments. Therefore, proper face masks can save lives while maintaining social life and securing the economy and the state.
But universal masking alone is not enough for two reasons: First, many people are not very good at following rules consistently. Therefore, it is advisable to observe the rules of hygiene and distance and to be careful even when wearing a mask. In the event of a car accident, the occupants are also protected by various devices (bumpers, crumple zone, safety belts, airbags, head and legroom, autonomous assistance systems, …). Second, some people are extremely bad at following rules, either because they do not want to or because they simply cannot. These people can become super spreaders. Therefore, the early detection of sources of infection and their isolation remains important beside universal masking and the rules of hygiene and distance.
Acknowledgement
The authors would like to thank Stefan Ostmann for conducting the mask experiments presented in Section 3.3 and Amirabas Bakhtiari for taking the microscopic images in Fig. 7.
Footnotes
It is clear that it is not enough to have a well tolerated and effective vaccine in large quantities. The vaccine must also be accepted and used by the world population.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaerosci.2020.105617.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., Vanstapel A., Werlein C., Stark H., Tzankov A., Li W.W., Li V.W. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. New England Journal of Medicine. 2020 doi: 10.1056/NEJMoa2015432. May 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi S., Wexler A.S., Cappa C.D., Barreda S., Bouvier N.M., Ristenpart W.D. Aerosol emission and super emission during human speech increase with voice loudness. Nature Scientiftic Reports. 2019;9:2348. doi: 10.1038/s41598-019-38808-z. https://www.nature.com/articles/s41598-019-38808-z.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae S., Kim M.-C., Kim J.Y., Cha H.-H., Lim J.S., Jung J., Kim M.-J., Oh D.K., Lee M.-K., Choi S.-H., Sung M., Hong S.-B., Chung J.-W., Kim S.-H. Effectiveness of surgical and cotton masks in blocking SARS-CoV-2: A controlled comparison in 4 patients. Annals of Internal Medicine. 2020 doi: 10.7326/M20-1342. published online on April 6. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Centers for Disease C, Prevention Estimates of deaths associated with seasonal influenza ––– United States, 1976–2007. MMWR Morb Mortal Wkly Rep. 2010;59(33):1057–1062. [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. The Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. published online on June 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A., Thompson K.-A., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: Would they protect in an influenza pandemic? Disaster Medicine and Public Health Preparedness. 2013;7:413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DIN EN 149 Respiratory protective devices – filtering half masks to protect against particles – requirements, testing, marking. German version EN. 2009;149 2001+A1, Beuth Verlag GmbH, 10772 Berlin. [Google Scholar]
- Doremalen van N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnick F. Abscheideeffizienz von Mund-Nasen-Schutz Masken, selbstgenähten Gesichtsmasken und potentiellen Maskenmaterialien. 2020. https://www.mpic.de/4646696/filtermasken_zusammenfassung_08_04_2020_v3_final.pdf called on May 28.
- Faust J.S., del Rio C. Assessment of deaths from COVID-19 and from seasonal influenza. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.2306. Published online May 14. [DOI] [PubMed] [Google Scholar]
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. The Lancet Respiratory Medicine. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grein J., Ohmagari N., Shin D., Diaz G., Asperges E., Castagna A., Oda R. Compassionate use of Remdesivir for patients with severe COVID-19. New England Journal of Medicine. 2020;382:2327–2336. doi: 10.1056/NEJMoa2007016. Published on April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X., Lau E.H.Y., Wu P., Deng X., Wang J., Hao X., Chung Lau Y., Wong J.Y., Guan Y., Tan X., Mo X., Chen Y., Liao B., Chen W., Hu F., Zhang Q., Zhong M., Wu Y., Zhao L.…Leung G.M. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nature Medicine. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- Howard J., Huang A., Li Z., Tufekci Z., Zdimal V., van der Westhuizen H., von Delft A., Price A., Fridman L., Tang L., Tang V., Watson G.L., Bax C.E., Shaikh R., Questier F., Hernandez D., Chu L.F., Ramirez C.M., Rimoin A.W. Face masks against COVID-19: An evidence review. Preprints. 2020. www.preprints.org not peer reviewed, Published on April 12. [DOI] [PMC free article] [PubMed]
- International Council of Nurses (ICN) 2020. https://www.icn.ch/news/more-600-nurses-die-covid-19-worldwide Called on June 10. [PubMed]
- Johnson G.R., Morawska L., Ristovski Z.D., Hargreaves M., Mengersen K., Chao C., Wan M.-P., Li Y., Xie X., Katoshevski D., Corbett S. Modality of human exposed aerosol size distributions. Journal of Aerosol Science. 2011;42:839–851. doi: 10.1016/j.jaerosci.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kähler C.J., Sammler B., Kompenhans J. Generation and control of tracer particles for optical flow investigations in air. Experiments in Fluids. 2002;33:736–742. [Google Scholar]
- Klompas M., Morris C.A., Sinclair J., Pearson M., Shenoy E.S. Universal masking in hospitals in the Covid-19 era. New England Journal of Medicine. 2020;382:e63. doi: 10.1056/NEJMp2006372. [DOI] [PubMed] [Google Scholar]
- Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K. Why do some COVID-19 patients infect many others, whereas most don't spread the virus at all? Science. 2020 doi: 10.1126/science.abc8931. May 19. [DOI] [Google Scholar]
- Kwok Y.L.A., Gralton J., McLaws M.-L. Face touching: A frequent habit that has implications for hand hygiene. American Journal of Infection Control. 2015;43:112–114. doi: 10.1016/j.ajic.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Yoo D., Ryu S., Ham S., Lee K., Yeo M., Min K., Yoon C. Quantity, size distribution, and characteristics of cough generated aerosol produced by patients with an upper respiratory tract infection. Aerosol and Air Quality Research. 2019;19:840–853. [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.-H., McDevitt J.J., Hau B.J.P., Yen H.-L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.-H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung C.C., Lam T.H., Cheng K.K. Mass masking in the COVID-19 epidemic: People need guidance. The Lancet. 2020;395:945. doi: 10.1016/S0140-6736(20)30520-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung G.M., Lam T.H., Ho L.M., Ho S.-Y., Chan B.H.Y., Wong I.O.L., Hedley A.J. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. Journal of Epidemiology & Community Health. 2003;57:857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu F., Qian H., Zheng X., Song J., Cao G., Liu Z. Evaporation and dispersion of exhaled droplets in stratified environment. IOP Conference Series: Materials Science and Engineering. 2019;609 [Google Scholar]
- Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Super spreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lok C. Where sneezes go. Nature. 2016;534:24–26. doi: 10.1038/534024a. [DOI] [PubMed] [Google Scholar]
- Lo J.Y., Tsang T.H., Leung Y.H., Yeung E.Y.H., Wu T., Lim W.W.L. Respiratory infections during SARS outbreak, Hong Kong, 2003. Emerging Infectious Diseases. 2005;11:1738–1741. doi: 10.3201/eid1111.050729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loudon R.G., Roberts R.M. Singing and the dissemination of tuberculosis. American Review of Respiratory Disease. 1968;98:297–300. doi: 10.1164/arrd.1968.98.2.297. https://www.atsjournals.org/doi/abs/10.1164/arrd.1968.98.2.297 [DOI] [PubMed] [Google Scholar]
- Marin A., Karpitschka S., Noguera-Marín D., Cabrerizo-Vílchez M.A., Rossi M. Solutal Marangoni flow as the cause of ring stains from drying salty colloidal drops. Physical Review Fluids. 2019;4 [Google Scholar]
- Marin A., Liepelt R., Rossi M., Kähler C.J. Surfactant-driven flow transitions in evaporating droplets. Soft Matter. 2016;12:1593–1600. doi: 10.1039/c5sm02354h. [DOI] [PubMed] [Google Scholar]
- Prather K.A., Wang C.C., Schooley R.T. Reducing transmission of SARS-CoV-2. Science. 2020 doi: 10.1126/science.abc6197. [DOI] [PubMed] [Google Scholar]
- Pyankov O.V., Bodnev S.A., Pyankova O.G., Agranovski I.E. Survival of aerosolized coronavirus in the ambient air. Journal of Aerosol Science. 2018;115:158–163. doi: 10.1016/j.jaerosci.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffel M., Willert C.E., Scarano F., Kähler C.J., Wereley S.T., Kompenhans J. Springer International Publishing AG; 2018. Particle image Velocimetry. [Google Scholar]
- Rensink D. Dissertation; Erlangen, Germany: 2004. Verdunstung akustisch levitierter schwingender Tropfen aus homogenen und heterogenen Medien. [Google Scholar]
- Reuther N., Kähler C.J. Effect of the intermittency dynamics on single and multipoint statistics of turbulent boundary layers. Journal of Fluid Mechanics. 2020;897 doi: 10.1017/jfm.2020.384. Published online by Cambridge University Press: 10 June 2020. [DOI] [Google Scholar]
- Rossi M., Marin A., Kähler C.J. Interfacial flows in sessile evaporating droplets of mineral water. Physical Review E. 2019;100 doi: 10.1103/PhysRevE.100.033103. [DOI] [PubMed] [Google Scholar]
- Ruedl G., Kopp M., Burtscher M. Does risk compensation undo the protection of Ski Helmet use? Epidemiology. 2012;23:936–937. doi: 10.1097/EDE.0b013e31826d2403. [DOI] [PubMed] [Google Scholar]
- Sande van der M., Teunis P., Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PloS One. 2008;3 doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott M.D., Buller D.B., Andersen P.A., Walkosz B.J., Voeks J.H., Dignan M.B., Cutter G.R. Testing the risk compensation hypothesis for safety helmets in alpine skiing and snowboarding. Injury Prevention. 2007;13:173–177. doi: 10.1136/ip.2006.014142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto W.H., Tsang D., Yung R.W., Ching T.Y., Ng T.K., Ho M., Ho L.M., Peiris J.S.M. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) The Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soper G.A. The lessons of the pandemic. Science. 1919;49:501–506. doi: 10.1126/science.49.1274.501. [DOI] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior, and Immunity. 2020;87:34–39. doi: 10.1016/j.bbi.2020.04.027. Published on April 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uvex (2020). https://www.uvex-safety.com/de/wissen/normen-und-richtlinien/atemschutzmasken/die-bedeutung-der-ffp-schutzklassen, called on May 20, 2020.
- Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: A model-based analysis. The Lancet. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Journal of the American Medical Association. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells W.F., Wells M.W. Journal A. M. A.; Cambridge: 1936. Air-bone infection; pp. 1698–1703. [Google Scholar]
- Wong J., Kelly H., Ip D.K., Wu J., Leung F., Cowling B. Case fatality risk of influenza A (H1N1pdm09): A systematic review. Epidemiology. 2013;24(6):830–841. doi: 10.1097/EDE.0b013e3182a67448. Issn print: 1044–3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. COVID-19: Considering the prevalence of schizophrenia in the coming decades. Psychiatry Research. 2020;288:112982. doi: 10.1016/j.psychres.2020.112982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Lib Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. PNAS. 2020 doi: 10.1073/pnas.2009637117. First published June 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.