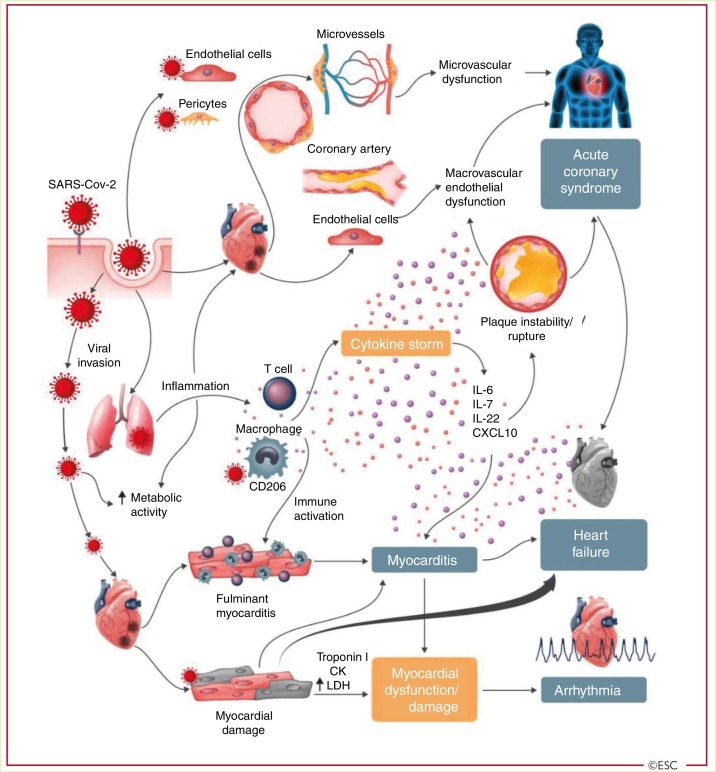
Figure 1.
Cardiovascular involvement in COVID-19 – key manifestations and hypothetical mechanisms. SARS-CoV-2 anchors on trans-membrane angiotensin-converting enzyme-2 to enter the host cells including type-2 pneumocytes, macrophages, endothelial cells, pericytes and cardiac myocytes leading to inflammation and multi- organ failure. Infection of endothelial cells or pericytes is of particular importance because this could lead to severe microvascular and macrovascular dysfunction. In addition, immune over-reactivity can potentially destabilize atherosclerotic plaques and explain the development of acute coronary syndromes. Infection of the respiratory tract, particularly type-2 pneumocytes, by SARS-CoV-2 is manifested by the progression of systemic inflammation and immune cell over-reaction leading to “cytokine storm”, resulting in increased levels of cytokines such as IL-6, IL-7, IL-22 and CXCL10. Subsequently, it is possible that activated T cell and macrophages may infiltrate infected myocardium resulting in the development of fulminant myocarditis and sever cardiac damage. This process may be further intensified by a cytokine storm. Similarly, the viral invasion my case cardiac myocyte damage directly leading to myocardial dysfunction and contribute to the development of arrhythmias.6 Reproduced from the original work “ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic” https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance.7 Permission obtained from © The European Society of Cardiology 2020. All rights reserved.