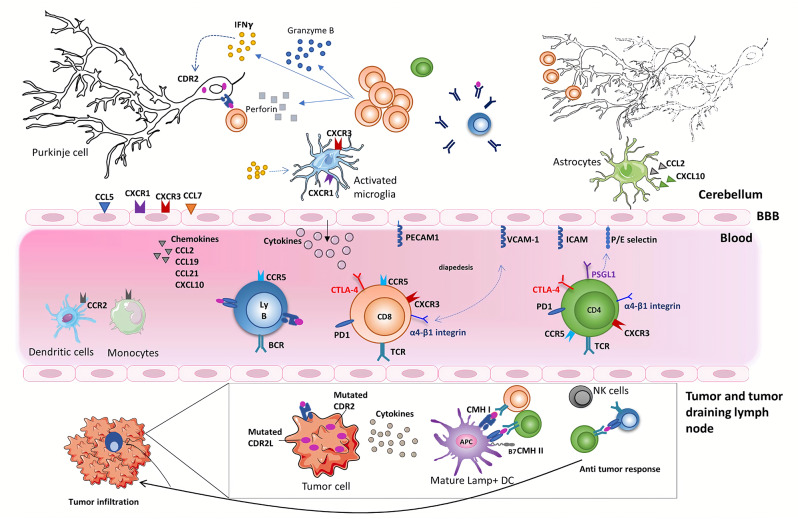
Figure 1.
Onconeural antigens such as CDR2 and CDR2L, mutated or not, can be the target of an anti-tumor immune response. Moderate to profound immune infiltrates are found in the primary tumor or metastases of anti-Yo PCD-associated tumors. These infiltrates sometimes form tertiary lymphoid structures. Priming of onconeural antigen-specific CD4 T cells may occur in the tumor-draining lymph nodes or the tumor itself following presentation by local DCs. Differentiation and recruitment of tumor antigen-specific cytotoxic CD8 T-cell likely contribute to the partial tumor control described in patients with PCD. B cells and plasma cells are also found in the tumor. The onconeural antigen-specific T cells reach the CNS after crossing the blood-brain barrier, through a multistep process involving selectins, integrins, and chemokine receptors. The preferential infiltration of the cerebellum in PCD patients could relate to presentation of the onconeural antigens by local APCs and/or to regional peculiarities. In the cerebellum of PCD patients, the inflammatory infiltrates are mostly composed of CD8 T cells, macrophages, and activated microglia. Purkinje neurons are naturally expressing onconeural antigen, such as CDR2 and CDR2L, and up-regulate their expression of MHC class I molecules during an inflammatory process providing the opportunity for CD8 T cells to recognize antigens presented by these neurons. Local CD8 T cells exhibit an activated phenotype with granzyme B- and perforin-containing cytolytic granules. They also secrete locally IFNγ, which has a number of disease-enhancing properties and, thus, is likely a key part of PCD pathogenesis. In particular, IFNγ increases the expression of MHC class I molecules on Purkinje neurons enhances VCAM1 expression on brain endothelial cells and elicits secretion of CXCL10, a ligand of CXCR3 expressed on Th1 cells and activated CD8 T cells. Although antibodies against intracellular onconeural antigens do not appear pathogenic in vivo, they could promote antigen presentation to pathogenic T cells.