ABSTRACT
Tic disorders (TD) is a neurodevelopmental disorder that is often first recognized in children and adolescents and is characterized mainly by motor and phonic tics. Drug treatment of TD has been criticized because of serious side effects, and TD treatment emphasizes behavioral psychotherapy. This study reviewed the most common behavioral psychotherapy for TD: habit reversal training (HRT). We examined the contents, variation, curative effects, and premonitory urge control of HRT and other behavioral psychotherapies. The findings suggest that current understanding of HRT is insufficient and further studies are needed. First, studies of online guidance training are needed to implement technology that can help more patients. Second, the future integration of HRT and other technologies is important. Third, imaging techniques could be used to further explore the brain mechanisms underlying HRT. Research on HRT for TD in China is insufficient. We call on more Chinese researchers to study, investigate, and develop technology to promote the development of behavioral psychotherapy for TD in China.
Keywords: Tic disorders, Habit reversal training, Comprehensive behavioral intervention for tics, Premonitory urges
1. Introduction
Tic disorders (TD) is a neurodevelopmental disorder that is often first recognized in children and adolescents and is characterized mainly by motor and/or phonic tics. TD is generally divided into three categories: transient TD, persistent (chronic) motor or vocal TD, and Tourette syndrome (TS). 1 Some studies have estimated that about 60%–80% of children with TD experience symptoms that can last until the age of 16 years, and about 23% of adolescents experience moderate and severe tics, which seriously affect social functioning. 2 At present, TD treatments mainly include both drug therapies (e.g., aripiprazole and tiapride hydrochloride) 3 and non‐drug therapies (e.g., habit reversal training [HRT] and transcranial magnetic stimulation). 4 Our previous studies on drug therapy for TD have shown that the efficacy of aripiprazole is stable. 5 However, owing to the chronic nature of TD, pharmacological treatment is often long‐term and has been criticized for its side effects, such as somnolence, weight gain, and extrapyramidal syndrome. 6
Therefore, non‐drug treatment of TD has increasingly attracted attention. Non‐drug therapy mainly comprises psychological and behavioral interventions and neuromodulation techniques (e.g., transcranial magnetic stimulation, transcranial direct current stimulation, and deep brain stimulation). Of these therapies, behavioral psychotherapy has been gradually recognized as safe and effective. 7 Currently, there are several kinds of psychological and behavioral interventions for TD. The most common is HRT, which forms the basis of the comprehensive behavioral intervention for tics (CBIT). 8 Psychosocial and behavioral interventions for TD have been recommended in Europe and Canada as a first‐line TD treatment. 9 , 10 The latest guideline from the American Academy of Neurology also suggests HRT as a first‐line treatment of TD. 11 As they worry about medication side effects, many parents of children with TD are willing to try HRT.
Drug therapy remains the dominant treatment of TD in China; only a few institutions offer behavioral psychotherapy for TD, and it is usually non‐standard. This review focused on the following aspects of HRT: 1) an introduction to HRT; 2) variation in HRT; 3) the curative effect of HRT; 4) the key to HRT: premonitory urge control; 5) other behavioral psychotherapies. Finally, we provide a brief overview of the limitations and future development of this method.
2. Overview of HRT
2.1. Content of HRT
HRT is the main behavioral psychotherapeutic approach for TD. HRT consists of three basic steps, two stages, and twelve sessions. 12
Three basic steps: (1) awareness training: guiding children to notice premonitory urges (the sensation before a tic occurs); (2) competing response training: identifying competing responses for each tic; for example, breathing could be selected as a competing response for vocal tics, and breathing through the nose for sniffing tics; (3) intensive training: selecting a family member to assist the child to complete the competing response intensive exercise (Figure 1).
Figure 1.
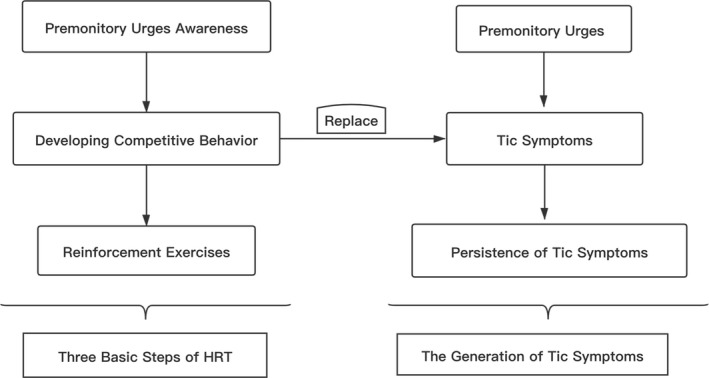
Three basic steps of habit reversal therapy
Two stages: stage one comprises sessions 1–8. These contain four main parts: tic awareness training, competing response training, relaxation training, and intensive training. The second stage is mainly a review and consolidation stage.
Twelve sessions: the first session introduces the basic process, familiarizes patients with reversal training, and introduces the methods and procedures. Sessions 2–6 occur weekly and develop different competitive behaviors for different tic symptoms. Sessions 7 and 8 occur every 2 weeks and mainly review and consolidate the contents of sessions 2–6. Sessions 9–12 occur every 4 weeks, and consolidate and review the previous training.
2.2. Variations of HRT: CBIT
CBIT is a new comprehensive intervention method first proposed by Woods in 2008. 13 CBIT is a highly structured behavioral therapy. The standard therapy is to complete eight treatments in 10 weeks; treatments can be personalized according to the specific needs of patients. The method consists of three parts: the first part familiarizes patients with their own tic symptoms and premonitory urges; the second part teaches patients competing responses that can be used when premonitory urges or tic symptoms occur (similar to HRT); the third step consists of adjustment of daily activities, especially those that aggravate or induce tic symptoms (for example, tic symptoms are usually aggravated when children encounter stressful situations), thereby reducing the likelihood of tic symptoms. CBIT is based on HRT. It provides an analysis of and response to environmental stimuli that affect the occurrence of tic symptoms. CBIT is a type of tic symptom management strategy and can be regarded as a supplement and extension of HRT. In addition to training of awareness and competing responses, CBIT includes relaxation training and psychoeducational intervention for events and environmental factors that affect tic severity. Patients are required to actively participate in the whole treatment process. 12
Some researchers have suggested that CBIT should be regarded as a first‐line treatment option for children over 9 years of age with TD. 1 Although CBIT may be effective for young TD children, there is still a lack of evidence‐based medical support. Wilhelm et al 14 randomly divided 122 patients with moderate or higher TS or chronic tic disorder (CTD) into two groups: one group was treated with CBIT and the other group was treated with psychoeducation and supportive therapy (PST). After 10 weeks of intervention, the CBIT group showed a more obvious alleviation of tic symptoms than the PST group, and follow‐up after 6 months of intervention showed that CBIT remained effective in 80% of patients with tic symptoms, whereas PST remained effective for 25% of patients, suggesting that CBIT was superior to psychoeducation in reducing the severity of tics and had better long‐term efficacy. Rowe et al 15 conducted eight CBIT training sessions with 30 TD children and their parents; compared with baseline, children's tic severity and anxiety/depression levels reduced after treatment, and their self‐perceived cognitive ability improved.
In addition to reducing tic severity, CBIT can also improve the self‐esteem of patients with TS or CTD. Weingarden et al 16 randomly divided 122 patients over 16 years old with IQs >80 into CBIT and PST intervention groups. These included 88 patients with no clinical comorbidity and 34 patients with at least one of attention deficit/ hyperactivity disorder (ADHD), obsessive–compulsive disorder, mood disorder, or anxiety disorder. The baseline results showed that self‐esteem scores were significantly lower in the comorbidity group than in the simple TS or CTD groups, and self‐esteem scores were negatively correlated with the severity of comorbidity and depression, but had no association with tic severity. After 10 weeks of intervention, self‐esteem scores in the comorbidity group with CBIT intervention were significantly improved compared with baseline, whereas self‐esteem scores in the PST group showed no significant change. A randomized controlled study by Chang et al 17 showed that CBIT intervention significantly reduced tic severity in children with TS. TS is often accompanied by ADHD and neurocognitive impairment, but CBIT has no effect on neurocognitive function in children. Specht et al 18 showed that, as CBIT intervention emphasizes the influence of environmental factors on tic symptoms, it is therefore effective in managing or eliminating those environmental factors that affect tic occurrence. However, it does not substantially improve premonitory urges.
The emergence of CBIT indicates that HRT needs further development and updating. Continuous application and evaluation of the method is needed to improve it. At the same time, we need to take into account the effect of cultural factors and age. Personalized treatment based on HRT may be developed in the future.
2.3. The efficacy of HRT
Several studies have confirmed that HRT can significantly reduce TD symptom severity. 4 , 19 , 20 A meta‐analysis of TD behavioral interventions showed that behavioral therapy yields medium to large effects. 21 Research on HRT has gradually increased over the past 5 years. Such research indicates that HRT is safe and effective, and also highlights problems with drug treatment. Moreover, HRT has been implemented in various ways. For example, online HRT has been used as a remote TD intervention that is cost‐effective for parents. 22 Group‐based HRT has been used for group therapy and has produced clinical improvements in symptoms. 23 Dutta et al 24 reviewed five randomized controlled studies on the treatment of TS and CTD in children and adults with HRT. The results showed that HRT significantly reduces tic severity in children and adults with TS and CTD. A study by Yates et al 25 randomly divided 33 CTD and TS children aged 9–13 years into a HRT group and a psychoeducation group. Tic severity was alleviated in both groups, and children’s quality of life improved; HRT was more effective in reducing motor tic symptoms than psychoeducation. A follow‐up study of 28 children after 12 months by Dabrowski et al 23 showed that HRT and psychoeducation improved children’s long‐term tic symptoms, quality of life, and school attendance rate; compared with the psychoeducation intervention group, the total tic score in the HRT group decreased more significantly. These studies have confirmed the stable efficacy of this method for both adults and children, and its ability to improve tic symptoms and social functioning.
HRT is becoming increasingly popular with families, and more parents are choosing behavioral psychotherapy as a TD treatment for their children and adolescents. Online guided HRT is a future development trend. Recent studies confirmed its effectiveness by showing that HRT based on the guidance of therapists and led by parents had a therapeutic effect of 1.12 and a response rate of 75%; the effect lasted more than 12 months after the intervention and was more acceptable to parents than other treatment types. 26 , 27
Finally, it should be pointed out that although there have been many studies on the efficacy of HRT, the method has some limitations. First, a single evaluation index of HRT’s curative effect tends to be used, the Yale Global Tic Severity Scale (YGTSS), but less attention has been paid to associated obsessive–compulsive symptoms, emotional and behavioral problems, and possible cognitive impairment. Premonitory urges have been particularly neglected. Second, curative effect evaluation uses simple statistical analysis (e.g., paired t‐tests or calculation of pre‐ and post‐intervention efficacy values), and experimental trols are not rigorous. Third, most studies focus on TD in adults; there is little evidence for the use of HRT in children and adolescents, particularly in China.
2.4. The key to HTR: Premonitory urges
The first step in HRT is the awareness exercise, and the object of awareness is the premonitory urge. What is a premonitory urge? A premonitory urge, also known as a sensory tic, is a special type of tic symptom, and is a sensation that occurs before the occurrence of tic symptoms. 28 Before the occurrence of a tic, there will be local or overall discomfort, such as “throat itching” before vocal tics and neck discomfort before shrugging shoulders. Tic symptoms occur to alleviate these sensations. 29 Premonitory urges are more common in patients with TS. As early as 1993, Leckman et al 30 reported that nearly 92% of TS children had premonitory urges. The most common locations of a premonitory urge are the head, neck, shoulder, and abdomen. Premonitory urges are more likely to occur before complex symptoms, and to occur less before simple symptoms such as blinking. This suggests that premonitory urges indicate more complex tic symptoms. At present, the most commonly used assessment of premonitory urge is the nine‐item Premonitory Urge for Tics Scale (PUTS) developed by Woods in 2005. 31 This has been widely used to assess premonitory urges.
We previously reported two special tic cases, both of which had tongue itching as the first symptom and often featured tongue biting to relieve the itching. 32 We have also encountered a large number of clinical cases that showed premonitory urges as the first symptoms. Moreover, we have found that premonitory urges appear more in children with TS, suggesting that they may be a pre‐symptom of tic symptoms, as well as an important index of the severity of tic symptoms. Our previous meta‐analysis further confirmed the association between premonitory urges and tic symptoms. 33
On the basis of the previous studies, we suggest that 1) premonitory urges are an indispensable component of the occurrence of tic symptoms; 2) premonitory urges form the basis or initial symptoms of tic symptoms; 3) premonitory urges indicate the severity of tic symptoms; 4) subsequent tic symptoms are needed to alleviate premonitory urges; and 5) premonitory urges can be regarded as recessive tics and tic symptoms as dominant tics, which complement each other.
2.5. Other behavioral treatments for TD
In recent years, many other psychological and behavioral interventions have emerged for TD (Table 1). Some of these methods are the application of existing psychological and behavioral techniques in TD treatment, and some have been developed based on HRT. Although the clinical efficacy of these techniques requires further verification, they provide more clinical options for TD behavioral psychotherapy, especially for children who fail to respond to HRT.
Table 1.
Psychological and behavioral interventions for tic disorders
| Psychological and behavioral intervention technique | Central principle |
|---|---|
| 78867023050500Massed negative practice (MNP) 34 | Allow the child actively repeat the target tics symptom, thus causing reaction inhibition or fatigue, and finally the extinction of the symptoms. |
| Self‐monitoring (SM) 35 | Let the patient record the frequency of tics, improve their self‐awareness of tic symptoms, so as to reduce tics. |
| Exposure with response prevention (ERP) 36 | Continuously expose the child to premonitory urges, break the positive strengthening cycle of premonitory urges and tics, gradually adapt the patient to this impulse, and reduce tics. |
| Cognitive behavioral therapy (CBT) 37 | Intervene in the negative cognition that causes tics symptoms, rather than the tic symptoms themselves. |
| 788670‐2590800078867021526500Assertiveness training (AT) 38 | Teach patients how to confidently face their tics symptoms, and make responses. |
| Biofeedback training (BT) 39 | A psychophysiological therapy based on inducing two different physiological states of sympathetic arousal and relaxation. |
| 78867023050500Contingency management (CM) 13 | Change behavior through stimulating control and positive reinforcement, which is widely used in the treatment of material dependence. |
| Relaxation therapy (RT) 40 | Relaxation training before the onset of tic symptoms (premonitory urge) to reduce the occurrence of tics symptoms. |
| Acceptance and commitment therapy (ACT) 41 | To accept rather than suppress the tic symptoms, and to reduce the occurrence of tics by adding relaxation training during tics. |
3. Limitations and future prospects
We can draw the following conclusions from the evidence discussed in this article:
There are two major steps to HRT: perceiving premonitory urges and developing competing responses to replace tic symptoms.
HRT is the most widely used treatment for TD. Its use is mostly evidence‐based, but there is little evidence from Chinese samples at present.
HRT should be further developed and updated to meet the treatment needs of individuals of different cultural backgrounds, ages, and genders, and the integration of other treatment techniques based on HRT is a future research direction.
Premonitory urges play an important role in HRT, and clarification of the relationship between premonitory urges and tic symptoms would be useful in further investigations of the possible mechanisms underlying HRT.
With the development of Internet technology, online guidance from therapists to parents may be an important future development.
There are several reasons why the psychological and behavioral intervention of TD is not yet well developed in China. First, there are few studies on HRT interventions in this area, and there is no evidence of its curative effect; second, although individual research centers have begun to apply psychological and behavioral interventions for TD, non‐standard implementation and low standardization are problems, indicating the necessity and urgency of research in this area; third, HRT has not been tailored to specific groups, and some of the terms in the operation manual to describe premonitory urges are difficult for patients to understand.
There are three main trends in the future development of HRT: first, further investigation of the online implementation process, evidence for a curative effect,and information about population suitability for HRT are needed; second, the integration of HRT and other methods, such as habit prevention exposure therapy, will be an important development for this method; third, there is currently little evidence of the brain mechanisms underlying HRT, and more research is particularly needed to clarify the role of premonitory urges in the training process. Finally, we call on more Chinese researchers to study, explore, and develop this method to promote the development of behavioral therapy for TD in China.
CONFLICT OF INTEREST
None.
Liu S, Li Y, Cui Y. Review of habit reversal training for tic disorders. Pediatr Invest. 2020;4:127–132. 10.1002/ped4.12190
Contributor Information
Ying Li, Email: liying@bch.com.cn.
Yonghua Cui, Email: cuiyonghua@bch.com.cn.
REFERENCES
- 1. Martino D, Pringsheim TM. Tourette syndrome and other chronic tic disorders: An update on clinical management. Expert Rev Neurother. 2018;18:125–137. [DOI] [PubMed] [Google Scholar]
- 2. Groth C, Mol Debes N, Rask CU, Lange T, Skov L. Course of tourette syndrome and comorbidities in a large prospective clinical study. J AM Acad Child Adolesc Psychiatry. 2017;56:304–312. [DOI] [PubMed] [Google Scholar]
- 3. Janik P, Szejko N. Aripiprazole in treatment of Gilles de la Tourette syndrome ‐ New therapeutic option. Neurol Neurochir Pol. 2018;52:84–87. [DOI] [PubMed] [Google Scholar]
- 4. Nissen JB, Kaergaard M, Laursen L, Parner E, Thomsen PH. Combined habit reversal training and exposure response prevention in a group setting compared to individual training: A randomized controlled clinical trial. Eur Child Adolesc Psychiatry. 2019;28:57–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cui YH, Zheng Y, Yang YP, Liu J, Li J. Effectiveness and tolerability of aripiprazole in children and adolescents with Tourette’s disorder: A pilot study in China. J Child Adolesc Psychopharmacol. 2010;20:291–298. [DOI] [PubMed] [Google Scholar]
- 6. Pandey S, Dash D. Progress in pharmacological and surgical management of tourette syndrome and other chronic tic disorders. Neurologist. 2019;24:93–108. [DOI] [PubMed] [Google Scholar]
- 7. Houghton DC, Capriotti MR, Scahill LD, Wilhelm S, Peterson AL, Walkup JT, et al. Investigating habituation to premonitory urges in behavior therapy for tic sisorders. Behav Ther. 2017;48:834–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Conelea CA, Wellen BCM. Tic treatment goes tech: A review of TicHelper.com. Cogn Behav Pract. 2017;24:374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Steeves T, McKinlay BD, Gorman D, Billinghurst L, Day L, Carroll A, et al. Canadian guidelines for the evidence‐based treatment of tic disorders: Behavioural therapy, deep brain stimulation, and transcranial magnetic stimulation. Can J Psychiatry. 2012;57:144–151. [DOI] [PubMed] [Google Scholar]
- 10. Verdellen C, van de Griendt J, Hartmann A, Murphy T, Group EG. European clinical guidelines for Tourette syndrome and other tic disorders. Part III: Behavioural and psychosocial interventions. Eur Child Adolesc Psychiatry. 2011;20:197–207. [DOI] [PubMed] [Google Scholar]
- 11. Pringsheim T, Holler‐Managan Y, Okun MS, Jankovic J, Piacentini J, Cavanna AE, et al. Comprehensive systematic review summary: Treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology. 2019;92:907–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGuire JF, Ricketts EJ, Piacentini J, Murphy TK, Storch EA, Lewin AB. Behavior therapy for tic disorders: An evidenced‐based review and new directions for treatment research. Curr Dev Disord Rep. 2015;2:309–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Franklin SA, Walther MR, Woods DW. Behavioral interventions for tic disorders. Psychiatr Clin North Am. 2010;33:641–655. [DOI] [PubMed] [Google Scholar]
- 14. Wilhelm S, Peterson AL, Piacentini J, Woods DW, Deckersbach T, Sukhodolsky DG, et al. Randomized trial of behavior therapy for adults with Tourette syndrome. Arch Gen Psychiatry. 2012;69:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rowe J, Yuen HK, Dure LS. Comprehensive behavioral intervention to improve occupational performance in children with Tourette disorder. Am J Occup Ther. 2013;67:194–200. [DOI] [PubMed] [Google Scholar]
- 16. Weingarden H, Scahill L, Hoeppner S, Peterson AL, Woods DW, Walkup JT, et al. Self‐esteem in adults with Tourette syndrome and chronic tic disorders: The roles of tic severity, treatment, and comorbidity. Compr Psychiatry. 2018;84:95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chang SW, McGuire JF, Walkup JT, Woods DW, Scahill L, Wilhelm S, et al. Neurocognitive correlates of treatment response in children with Tourette’s Disorder. Psychiatry Res. 2018;261:464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Specht MW, Woods DW, Nicotra CM, Kelly LM, Ricketts EJ, Conelea CA, et al. Effects of tic suppression: Ability to suppress, rebound, negative reinforcement, and habituation to the premonitory urge. Behav Res Ther. 2013;51:24–30. [DOI] [PubMed] [Google Scholar]
- 19. Seragni G, Chiappedi M, Bettinardi B, Zibordi F, Colombo T, Reina C, et al. Habit reversal training in children and adolescents with chronic tic disorders: An Italian randomized, single‐blind pilot study. Minerva Pediatr. 2018;70:5–11. [DOI] [PubMed] [Google Scholar]
- 20. Viefhaus P, Feldhausen M, Gortz‐Dorten A, Volk H, Dopfner M, Woitecki K. Efficacy of habit reversal training in children with chronic tic disorders: A within‐subject analysis. Behav Modif. 2020;44:114–136. [DOI] [PubMed] [Google Scholar]
- 21. McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, et al. A meta‐analysis of behavior therapy for Tourette syndrome. J Psychiatr Res. 2014;50:106–112. [DOI] [PubMed] [Google Scholar]
- 22. Jakubovski E, Reichert C, Karch A, Buddensiek N, Breuer D, Muller‐Vahl K. The ONLINE‐TICS study protocol: A randomized observer‐blind clinical trial to demonstrate the efficacy and safety of internet‐delivered behavioral treatment for adults with chronic tic disorders. Front Psychiatry. 2016;7:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dabrowski J, King J, Edwards K, Yates R, Heyman I, Zimmerman‐Brenner S, et al. The long‐term effects of group‐based psychological interventions for children with Tourette syndrome: A randomized controlled trial. Behav Ther. 2018;49:331–343. [DOI] [PubMed] [Google Scholar]
- 24. Dutta N, Cavanna AE. The effectiveness of habit reversal therapy in the treatment of Tourette syndrome and other chronic tic disorders: A systematic review. Funct Neurol. 2013;28:7–12. [PMC free article] [PubMed] [Google Scholar]
- 25. Yates R, Edwards K, King J, Luzon O, Evangeli M, Stark D, et al. Habit reversal training and educational group treatments for children with tourette syndrome: A preliminary randomised controlled trial. Behav Res Ther. 2016;80:43–50. [DOI] [PubMed] [Google Scholar]
- 26. Andrén P, Aspvall K, Fernández de la Cruz L, Wiktor P, Romano S, Andersson E, et al. Therapist‐guided and parent‐guided internet‐delivered behaviour therapy for paediatric Tourette’s disorder: A pilot randomised controlled trial with long‐term follow‐up. BMJ Open. 2019;9:e024685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hall CL, Davies EB, Andrén P, Murphy T, Bennett S, Brown BJ, et al. Investigating a therapist‐guided, parent‐assisted remote digital behavioural intervention for tics in children and adolescents‐‘Online Remote Behavioural Intervention for Tics’ (ORBIT) trial: Protocol of an internal pilot study and single‐blind randomised controlled trial. BMJ Open. 2019;9:e027583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McGuire JF, McBride N, Piacentini J, Johnco C, Lewin AB, Murphy TK, et al. The premonitory urge revisited: An individualized premonitory urge for tics scale. J Psychiatr Res. 2016;83:176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cavanna AE, Black KJ, Hallett M, Voon V. Neurobiology of the premonitory urge in Tourette's syndrome: Pathophysiology and treatment implications. J Neuropsychiatry Clin Neurosci. 2017;29:95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leckman JF, Walker DE, Cohen DJ. Premonitory urges in Tourette’s syndrome. Am J Psychiatry. 1993;150:98–102. [DOI] [PubMed] [Google Scholar]
- 31. Woods DW, Piacentini J, Himle MB, Chang S. Premonitory urge for Tics Scale (PUTS): Initial psychometric results and examination of the premonitory urge phenomenon in youths with Tic disorders. J Dev Behav Pediatr. 2005;26:397–403. [DOI] [PubMed] [Google Scholar]
- 32. Li Y, Zhang JS, Wen F, Lu XY, Yan CM, Wang F, et al. Premonitory urges located in the tongue for tic disorder: Two case reports and review of literature. World J Clin Cases. 2019;7:1508–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li Y, Wang F, Liu J, Wen F, Yan C, Zhang J, et al. The correlation between the severity of premonitory urges and tic symptoms: A meta‐analysis. J Child Adolesc Psychopharmacol. 2019;29:652–658. [DOI] [PubMed] [Google Scholar]
- 34. Storms L. Massed negative practice as a behavioral treatment for Gilles de la Tourette’s syndrome. Am J Psychother. 1985;39:277–281. [DOI] [PubMed] [Google Scholar]
- 35. Himle MB, Woods DW, Piacentini JC, Walkup JT. Brief review of habit reversal training for Tourette syndrome. J Child Neurol. 2006;21:719–725. [DOI] [PubMed] [Google Scholar]
- 36. Verdellen CW, Keijsers GP, Cath DC, Hoogduin CA. Exposure with response prevention versus habit reversal in Tourettes’s syndrome: A controlled study. Behav Res Ther. 2004;42:501–511. [DOI] [PubMed] [Google Scholar]
- 37. Morand‐Beaulieu S, O’Connor KP, Sauvé G, Blanchet PJ, Lavoie ME. Cognitive‐behavioral therapy induces sensorimotor and specific electrocortical changes in chronic tic and Tourette’s disorder. Neuropsychologia. 2015;79:310–321. [DOI] [PubMed] [Google Scholar]
- 38. Mansdorf IJ. Assertiveness training in the treatment of a child’s tics. J Behav Ther Exp Psychiatry. 1986;17:29–32. [DOI] [PubMed] [Google Scholar]
- 39. Nagai Y, Cavanna A, Critchley HD. Influence of sympathetic autonomic arousal on tics: Implications for a therapeutic behavioral intervention for Tourette syndrome. J Psychosom Res. 2009;67:599–605. [DOI] [PubMed] [Google Scholar]
- 40. Bergin A, Waranch HR, Brown J, Carson K, Singer HS. Relaxation therapy in Tourette syndrome: A pilot study. Pediatr Neurol. 1998;18:136–142. [DOI] [PubMed] [Google Scholar]
- 41. Franklin ME, Best SH, Wilson MA, Loew B, Compton SN. Habit reversal training and acceptance and commitment therapy for Tourette syndrome: A pilot project. J Dev Phys Disabil. 2011;23:49–60. [Google Scholar]


