Abstract
Background
Trends in acute myocardial infarction (AMI) incidence rates for diverse races/ethnicities are largely unknown, presenting barriers to understanding the role of race/ethnicity in AMI occurrence.
Methods and Results
We identified AMI hospitalizations for Kaiser Permanente Southern California members, aged ≥35 years, during 2000 to 2014 using discharge diagnostic codes. We excluded hospitalizations with missing race/ethnicity information. We calculated annual incidence rates (age and sex standardized to the 2010 US census population) for AMI, ST‐segment–elevation myocardial infarction, and non–ST‐segment–elevation myocardial infarction by race/ethnicity (Hispanic and non‐Hispanic racial groups: Asian or Pacific Islander, black, and white). Using Poisson regression, we estimated annual percentage change in AMI, non–ST‐segment–elevation myocardial infarction, and ST‐segment–elevation myocardial infarction incidence by race/ethnicity and AMI incidence rate ratios between race/ethnicity pairs, adjusting for age and sex. We included 18 630 776 person‐years of observation and identified 44 142 AMI hospitalizations. During 2000 to 2014, declines in AMI, non–ST‐segment–elevation myocardial infarction, and ST‐segment–elevation myocardial infarction were 48.7%, 34.2%, and 69.8%, respectively. Age‐ and sex‐standardized AMI hospitalization rates/100 000 person‐years declined for Hispanics (from 307 to 162), Asians or Pacific Islanders (from 271 to 158), blacks (from 347 to 199), and whites (from 376 to 189). Annual percentage changes ranged from −2.99% to −4.75%, except for blacks, whose annual percentage change was −5.32% during 2000 to 2009 and −1.03% during 2010 to 2014.
Conclusions
During 2000 to 2014, AMI, non–ST‐segment–elevation myocardial infarction, and ST‐segment–elevation myocardial infarction hospitalization incidence rates declined substantially for each race/ethnic group. Despite narrowing rates among races/ethnicities, differences persist. Understanding these differences can help identify unmet needs in AMI prevention and management to guide targeted interventions.
Keywords: acute myocardial infarction, cardiovascular disease, incidence rates, race/ethnicity, trends
Subject Categories: Epidemiology, Myocardial Infarction, Race and Ethnicity
Clinical Perspective
What Is New?
Declines in acute myocardial infarction, non–ST‐segment–elevation myocardial infarction, and ST‐segment–elevation myocardial infarction hospitalization incidence rates were observed across all race/ethnic groups during 2000 to 2014; however, declines plateaued among blacks, but not other race/ethnic groups, beginning in 2010.
Acute myocardial infarction, non–ST‐segment–elevation myocardial infarction, and ST‐segment–elevation myocardial infarction incidence rates for Hispanics and Asians or Pacific Islanders were lower than rates for whites during the study period, but by 2014 Asians or Pacific Islanders were no longer the group with the lowest incidence of acute myocardial infarction and ST‐segment–elevation myocardial infarction.
What Are the Clinical Implications?
Improvements in the prevention and treatment of cardiovascular risk factors likely had a considerable influence on the declining incidence of acute myocardial infarction in this population; however, despite narrowing rates between race/ethnic groups, differences persisted, suggesting that further efforts are needed to identify inequities in unmet needs in primary prevention.
Acute myocardial infarction (AMI) is a common and potentially fatal presentation of cardiovascular disease (CVD). In the United States, an estimated 605 000 incident AMIs and 200 000 recurrent AMIs occur each year.1 Studies of community‐based cohorts and Medicare beneficiaries from the 1970s through 2010 observed >20% declines in AMI hospitalizations, but reported smaller declines for blacks, compared with whites.2, 3 Most studies have focused on differences between blacks and whites, leaving gaps in our understanding of AMI trends for other races/ethnicities.
Population sizes for some races/ethnicities, including Asians and Hispanics, are growing rapidly in the United States; whereas the non‐Hispanic white population is projected to decrease by 16 million during 2014 to 2060.4 The US Census Bureau estimated that >50% of the US population will belong to a race/ethnic minority group by 2044.4 Limited knowledge of trends in AMI incidence for Asians or Pacific Islanders (APIs) and Hispanics presents challenges to understanding the contribution of race/ethnicity in the cause of AMI occurrence and the need for planning culturally appropriate strategies for AMI prevention and management (eg, inclusion of some aspect of a group's cultural values in the strategy). We examined trends in incidence of AMI hospitalizations by race/ethnicity during 2000 to 2014 for the membership of Kaiser Permanente Southern California (KPSC), a large, integrated healthcare delivery system.
Methods
Anonymized data that support the findings of this study are made available from the corresponding author on reasonable request from qualified researchers with documented evidence of training in human subjects protections.
Study Population
KPSC currently exceeds 4.6 million members and represents a unique setting to observe AMI trends across race/ethnic groups. KPSC members are representative of the insured population within the service area, comprising 10 southern California counties.5 KPSC members’ receipt of outpatient, inpatient, laboratory, and pharmacy services is tracked in the electronic health record system. Services performed outside of KPSC hospitals and medical offices are tracked through billing claims submitted to KPSC. In this study, we included people aged ≥35 years with ≥4 years of continuous membership and race/ethnicity information available.
Member Demographics
Age, sex, race/ethnicity, and health plan enrollment status were obtained from electronic membership records. Races/ethnicities were categorized into mutually exclusive groups, including Hispanic (regardless of race) and the following non‐Hispanic racial groups: API, black, white, and a group consisting of Native American/Alaskan Native, multiple, or other (multiple/other) races.
Identification of AMI Hospitalizations
We identified hospitalizations during January 1, 1996, to December 31, 2014, with a principal discharge diagnosis of AMI using previously validated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) codes 410.xx (excluding 410.x2) from hospital discharge records and inpatient claims.6, 7 An incident AMI hospitalization was defined as the first documented hospitalization during 2000 to 2014 for people with no history of AMI hospitalization during the previous 4 years. Each person identified to have an incident AMI hospitalization had at least 4 years of observation before the incident AMI hospitalization. Similarly, ICD‐9‐CM codes were used to identify the incidence of ST‐segment–elevation myocardial infarction (STEMI) hospitalizations (410.0–410.6 and 410.8) and non–ST‐segment–elevation myocardial infarction (NSTEMI) hospitalizations (410.7 and 410.9). In AMI analyses, myocardial infarction could be STEMI or NSTEMI. STEMI or NSTEMI analyses included the first event of the corresponding type.
Statistical Analysis
Demographic characteristics of people hospitalized with incident AMI were summarized overall and by race/ethnic groups (Table 1). To improve visibility of Table 1, demographic characteristics were summarized in three 5‐year periods: 2000 to 2004, 2005 to 2009, and 2010 to 2014.
Table 1.
Characteristics of People Hospitalized for AMI by Race/Ethnicity and Year, Kaiser Permanente Southern California, 2000 to 2014
| Characteristics | Overall | Hispanica | Asian or Pacific Islandera | Blacka | Whitea | Multiple/Othera |
|---|---|---|---|---|---|---|
| Years 2000–2004 | ||||||
| N (%) | 15 159 (100.0) | 2526 (16.7) | 870 (5.7) | 1811 (11.9) | 9882 (65.2) | 70 (0.5) |
| Age, mean±SD, y | 68.6±12.6 | 64.3±12.5 | 65.2±11.9 | 66.5±12.0 | 70.4±12.3 | 64.0±13.4 |
| Age group, y, % | ||||||
| 35–54 | 16.0 | 25.0 | 23.1 | 18.9 | 12.5 | 25.7 |
| 55–74 | 49.8 | 53.4 | 55.2 | 54.7 | 47.5 | 52.9 |
| ≥75 | 34.2 | 21.5 | 21.7 | 26.3 | 40.0 | 21.4 |
| Sex, % | ||||||
| Women | 36.7 | 31.3 | 27.9 | 44.5 | 37.4 | 30.0 |
| Men | 63.3 | 68.7 | 72.1 | 55.5 | 62.6 | 70.0 |
| Years 2005–2009 | ||||||
| N (%) | 14 527 (100.0) | 2959 (20.4) | 1021 (7.0) | 1597 (11.0) | 8844 (60.9) | 106 (0.7) |
| Age, mean±SD, y | 69.0±12.8 | 65.4±12.7 | 66.3±12.0 | 67.8±12.6 | 70.7±12.6 | 68.0±12.7 |
| Age group, y, % | ||||||
| 35–54 | 15.4 | 22.7 | 17.4 | 16.8 | 12.4 | 17.9 |
| 55–74 | 49.3 | 51.7 | 58.3 | 51.7 | 47.1 | 48.1 |
| ≥75 | 35.3 | 25.6 | 24.3 | 31.4 | 40.5 | 34.0 |
| Sex, % | ||||||
| Women | 37.0 | 33.7 | 27.9 | 48.7 | 37.1 | 32.1 |
| Men | 63.0 | 66.3 | 72.1 | 51.3 | 62.9 | 67.9 |
| Years 2010–2014 | ||||||
| N (%) | 14 456 (100.0) | 3339 (23.1) | 1211 (8.4) | 1696 (11.7) | 8097 (56.0) | 113 (0.8) |
| Age, mean±SD, y | 70.0±13.0 | 66.3±13.2 | 67.1±12.7 | 68.9±12.7 | 72.3±12.5 | 65.2±13.2 |
| Age group, y, % | ||||||
| 35–54 | 13.8 | 21.6 | 18.3 | 14.6 | 9.5 | 23.0 |
| 55–74 | 48.0 | 49.8 | 52.9 | 51.1 | 45.9 | 47.8 |
| ≥75 | 38.2 | 28.6 | 28.7 | 34.3 | 44.5 | 29.2 |
| Sex, % | ||||||
| Women | 38.5 | 36.1 | 30.5 | 50.1 | 38.3 | 33.6 |
| Men | 61.5 | 63.9 | 69.5 | 49.9 | 61.7 | 66.4 |
Percentages might not add up to 100% because of rounding to the nearest tenth of a percentage. AMI indicates acute myocardial infarction.
People were categorized as Hispanic (regardless of race) or as one of the following non‐Hispanic race groups: Asian or Pacific Islander, black, white, or multiple/other.
For each year during 2000 to 2014, we calculated age‐ and sex‐standardized incidence rates/100 000 person‐years separately for AMI, NSTEMI, and STEMI by race/ethnicity using direct adjustment to the 2010 US Census Bureau population distribution. Numerators were the number of incident AMI, NSTEMI, or STEMI hospitalizations within the year. Denominators for each year were the total number of person‐years for all KPSC members, including people without an AMI. Denominators excluded person‐time from those missing race/ethnicity information among people who were aged ≥35 years with ≥4 years of membership. Within each race/ethnic group, we calculated AMI incidence stratified by age group (35–54, 55–74, and ≥75 years) and sex. Poisson distribution was used to estimate SEs and 95% CIs. We used Poisson regression to estimate the annual percentage changes (APCs) during 2000 to 2014 for AMI, STEMI, and NSTEMI incidence rates by race/ethnicity, adjusting for age and sex. We assessed trends for race/ethnic groups by including interaction terms between year and race/ethnicity in the Poisson regression models. Linear trends were modeled for all races/ethnicities, unless there was evidence for nonlinearity. We investigated nonlinearity by fitting generalized additive models and testing the smoothing effect of year, adjusting for age and sex. If nonlinear trends were identified, we modeled trends using linear spline regression, which allowed testing the change of APCs from one period to another.8 We also calculated APCs stratified by age group and sex. To determine if differences existed in the percentage declines between race/ethnic groups, we compared the 95% CIs of the APCs. We also estimated the incidence rate ratios to compare the incidence rates for each race/ethnicity pair in 2000 and again in 2014 using Poisson regression.
Sensitivity analyses were conducted to assess whether AMI hospitalization trends differed using 1, 2, and 8 years of time in membership requirements, compared with a 4‐year requirement. All analyses were conducted using SAS, version 9.3 (SAS Institute, Cary, NC). The study protocol was reviewed and approved by the KPSC Institutional Review Board, and a waiver for written informed consent was obtained. KPSC ensured compliance with Health Insurance Portability and Accountability Act regulations.
Results
We included 18 630 776 person‐years of observation in the study, with the following race/ethnicity distribution: 5 720 814 (30.7%) person‐years for Hispanics, 1 835 454 (9.9%) person‐years for APIs, 2 212 507 (11.9%) person‐years for blacks, 8 596 768 (46.1%) person‐years for whites, and 265 233 (1.4%) person‐years for multiple/other race (Table S1). We identified 45 331 AMI hospitalizations. We excluded 1189 (2.6%) hospitalizations missing race/ethnicity information. Among the remaining 44 142 people with hospitalizations, mean age at AMI was 69.2 years, with an SD of 12.8 years; 27 633 (62.6%) were men; 8824 (20.0%) were Hispanic, 3102 (7.0%) were API, 5104 (11.6%) were black, 26 823 (60.8%) were white, and 289 (0.7%) were of multiple/other race. Table 1 and Tables S2 and S3 show demographic characteristics of people with incident AMI hospitalization by race/ethnicity or type of AMI (NSTEMI or STEMI), respectively.
AMI, NSTEMI, and STEMI Incidence Rates Standardized for Age and Sex
During 2000 to 2014, standardized AMI hospitalization incidence rates/100 000 person‐years declined for Hispanics (from 307 to 162), APIs (271 to 158), blacks (347 to 199), whites (376 to 189), and multiple/other races (232 to 99) (Figure 1 and Table S4). AMI rates, in descending order, were highest for whites, blacks, Hispanics, and APIs. Among women, black women had the highest AMI rates among women aged 35 to 74 years, and black and white women aged ≥75 years had similar rates (Figure 2 and Table S5). In contrast, white men had the highest AMI rates across all age groups among men (Figure 2 and Table S6). NSTEMI incidence rates declined for Hispanics (from 181 to 132), APIs (154 to 116), blacks (240 to 171), whites (234 to 150), and multiple/other races (108 to 99) (Figure 1 and Table S7). NSTEMI rates were similar for blacks and whites (although rates for blacks became consistently higher than rates for whites after 2009), and these rates were followed by rates for Hispanics and then APIs. STEMIs also declined for Hispanics (from 150 to 44), APIs (122 to 46), blacks (133 to 41), whites (175 to 54), and multiple/other races (146 to 12) (Figure 1 and Table S8). Whites had the highest STEMI rates throughout the study period. In 2008, AMI incidence rates for Hispanics, APIs, and blacks converged. Incidence rates for people of multiple/other races were variable because their numbers were limited; they are not included in Figures 1 and 2 to increase visibility. These numbers are provided in Tables S4 through S8.
Figure 1.
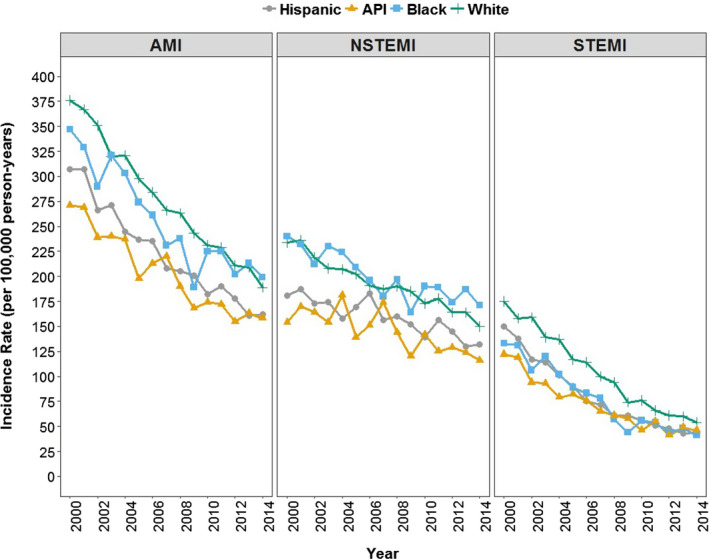
Overall incidence for acute myocardial infarction (AMI), non–ST‐segment–elevation myocardial infarction (NSTEMI), and ST‐segment–elevation myocardial infarction (STEMI) hospitalizations per 100 000 person‐years by race/ethnicity, standardized by age and sex, Kaiser Permanente Southern California, 2000 to 2014. Race/ethnic groups include Hispanic (regardless of race) and the following non‐Hispanic racial groups: Asian or Pacific Islander (API), black, and white.
Figure 2.
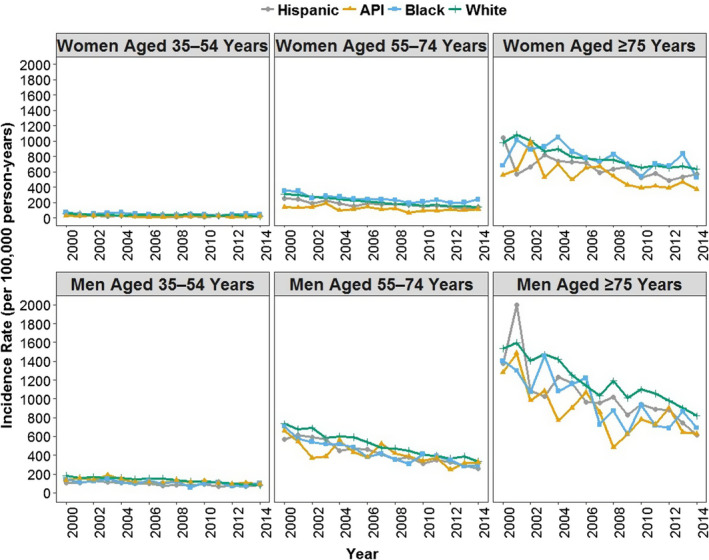
Overall acute myocardial infarction hospitalizations per 100 000 person‐years by race/ethnicity, age, and sex, Kaiser Permanente Southern California, 2000 to 2014. Race/ethnic groups include Hispanic (regardless of race) and the following non‐Hispanic racial groups: Asian or Pacific Islander (API), black, and white.
Trends in AMI, NSTEMI, and STEMI Incidence Rates
During 2000 to 2014, we observed a 48.7% (from 349 to 179) decrease in AMI incidence rates, standardized for age and sex, and an incidence decline for each race/ethnic group (Figure 1 and Table S4). Using Poisson regression, we estimated that during 2000 to 2014, the APC (95% CI) was −4.51% (−4.97% to −4.04%) for Hispanics, −4.11% (−4.90% to −3.32%) for APIs, −4.75% (−5.02% to −4.49%) for whites, and −2.99% (−5.65% to −0.26%) for multiple/other races (Table 2). The APCs across race/ethnic groups were similar, except for blacks. We identified nonlinear declines in AMI incidence among blacks, as indicated by generalized additive models (data not displayed). A linear spline model with one knot at year 2009 was fitted for blacks, and the APC (95% CI) was −5.31% (−6.31% to −4.30%) during 2000 to 2009; during 2010 to 2014, APC (95% CI) was −1.05% (−3.09% to 1.02%).
Table 2.
APC in Hospitalizations for AMI, NSTEMI, and STEMI, Adjusted by Age and Sex, by Race/Ethnicity, Kaiser Permanente Southern California, 2000 to 2014
| Event Type | Hispanica | Asian or Pacific Islandera | Black 2000–2009a, b | Black 2010–2014a, b | Whitea | Multiple/Othera |
|---|---|---|---|---|---|---|
| AMI | −4.51 (−4.97 to −4.04) | −4.11 (−4.90 to −3.32) | −5.31 (−6.31 to −4.30) | −1.05 (−3.09 to 1.02) | −4.75 (−5.02 to −4.49) | −2.99 (−5.65 to −0.26) |
| NSTEMI | −2.23 (−2.80 to −1.65) | −2.54 (−3.50 to −1.58) | −2.28 (−2.98 to −1.57) | −2.28 (−2.98 to −1.57) | −2.88 (−3.20 to −2.56) | −1.16 (−4.59 to −2.40) |
| STEMI | −8.60 (−9.34 to −7.86) | −7.42 (−8.70 to −6.12) | −8.84 (−9.90 to −7.77) | −8.84 (−9.90 to −7.77) | −8.53 (−8.95 to −8.10) | −8.41 (−12.55 to −4.08) |
AMI indicates acute myocardial infarction; APC, annual percentage change; NSTEMI, non‐STEMI; STEMI, ST‐segment–elevation myocardial infarction.
People were categorized as Hispanic (regardless of race) or as one of the following non‐Hispanic race groups: Asian or Pacific Islander, black, white, or multiple/other.
A linear spline model with one knot at year 2009 was fitted for the black people to account for nonlinearity in the decline in AMI incidence. This allowed for different estimations of the APC for 2000 to 2009 and 2010 to 2014. No statistically significant evidence of nonlinearity in the decline of hospitalized NSTEMI and STEMI incidence rates was observed.
During 2000 to 2014, the relative decline in people hospitalized with NSTEMI was 34.2% (from 219 to 144), and the relative decline in people hospitalized with STEMI was 69.8% (159 to 48) (Figure 1 and Table S7 and S8). APCs (95% CIs) in NSTEMI incidence rates were −2.23% (−2.80% to −1.65%) for Hispanics, −2.54% (−3.50% to −1.58%) for APIs, −2.28% (−2.98% to −1.57%) for blacks, −2.88% (−3.20% to −2.56%) for whites, and −1.16% (−4.59% to 2.40%) for multiple/other races (Table 2). APCs (95% CIs) in STEMIs during this period were −8.60 (−9.34% to −7.86%) for Hispanics, −7.42% (−8.70% to −6.12%) for APIs, −8.84% (−9.90% to −7.77%) for blacks, −8.53% (−8.95% to −8.10%) for whites, and −8.41% (−12.55% to −4.08%) for multiple/other races (Table 2).
In sensitivity analyses, using 1, 2, or 8 years of time in membership did not change trends in AMI incidence, compared with a 4‐year membership requirement, although estimated rates were different (Figure S1).
Race/Ethnic Group Incidence Rate Ratios in 2000 and 2014
AMI incidence rates were significantly lower for blacks, APIs, and Hispanics than for whites in 2000 (P<0.001; Figure 3). In 2014, rates for APIs and Hispanics were still lower than rates for whites (P<0.0001); however, rates between blacks and whites were similar (P=0.93). AMI incidence rates for APIs and Hispanics were lower than AMI rates for blacks in 2000 and 2014 (P<0.0001). Compared with APIs, Hispanics had higher AMI incidence rates in 2000 (P=0.008), although AMI incidence rates were similar for both groups in 2014 (P=0.14).
Figure 3.
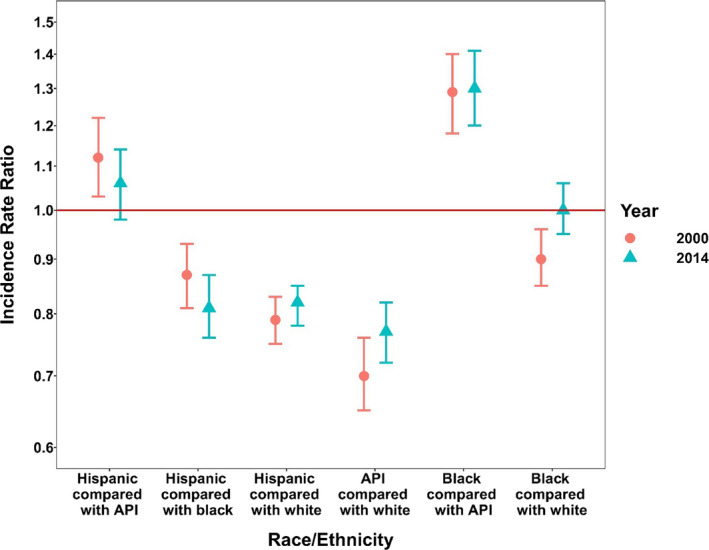
Incidence rate ratios for acute myocardial infarction for race/ethnicity pairs in 2000 and 2014, Kaiser Permanente Southern California. People were categorized as Hispanic (regardless of race) or as one of the following non‐Hispanic racial groups: Asian or Pacific Islander (API), black, or white.
Discussion
Among people aged ≥35 years, we observed considerable declines in the incidence of AMI hospitalizations during a 15‐year period (2000–2014) across all race/ethnic groups in a large, diverse, community‐based population. The decline of STEMI was approximately twice the decline of NSTEMI. Declines for most race/ethnic groups were similar, except for blacks, who experienced a steep decline in AMI rates during 2000 to 2009 that slowed during 2010 to 2014. Results indicate that although AMI incidence rates narrowed between races/ethnicities, particularly between black and white and between API and Hispanic groups, differences by race/ethnicity persist.
These results extend previous reports of substantial decreases in rates of AMI hospitalizations in the United States during the past 2 decades, which typically reported AMI declines of 24% to 30% corresponding to the first half of our study period (≈2000–2007).3, 7, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 We observed a relative decline in AMI of 48.7% over a study period that is nearly twice as long (2000–2014). In Kaiser Permanente Northern California, STEMI rates decreased steeply from 1999 to 2008, whereas NSTEMI rates increased from 1999 to 2004 and then decreased thereafter, which is consistent with our observation of steeper declines in STEMI compared with NSTEMI. A follow‐up study in Kaiser Permanente Northern California from 2008 to 2014 demonstrated that AMI rates continued to decrease, although declines were driven by NSTEMI rather than STEMI.18 In our study, we did not find statistically significant evidence of nonlinearity for the APCs in NSTEMI or STEMI rates over the study period. However, although the APCs are consistent across years, the magnitude of the rate decreases becomes smaller over time.
Declines in AMI rates have been attributed to improvements in CVD awareness, treatment, and risk factor management.7 Although not analyzed in our study, efforts to improve and standardize long‐term and preventive care at KPSC likely contributed to declines in incident AMI hospitalizations.19 KPSC has prioritized hypertension control and increased the use of statins for primary prevention.20, 21
Our study provides evidence to expand the limited literature assessing AMI hospitalization incidence rates for Hispanics and APIs in the United States. During 2000 to 2014, we observed similar declines in AMI, NSTEMI, and STEMI hospitalization incidence rates for Hispanics, APIs, and whites, indicating that these groups might have experienced similar benefits from improvements in CVD awareness and care. Our results also reveal that AMI, NSTEMI, and STEMI incidence rates for Hispanics and APIs were lower than rates for whites during the study period. Although not directly comparable to our more contemporary study, results from the Corpus Christi Heart Project reported that Mexican people who resided in one Texas community had higher AMI incidence rates than their white counterparts during 1988 to 1992.22 For APIs, CVD incidence data are severely lacking in the United States; however, studies report that compared with other races/ethnicities, APIs have lower prevalence of coronary heart disease and stroke and a higher prevalence of ideal cardiovascular health metrics.1 Although we observed AMI rates for APIs as the lowest among all race/ethnic groups in 2000, AMI rates for APIs and Hispanics converged by the end of the study period. In addition, NSTEMI rates also converged for APIs, Hispanics, and blacks. Our results provide new data indicating that by 2014, APIs in our study population were no longer the group with the lowest incidence of AMI and STEMI. However, our API and Hispanic categories aggregate multiple race/ethnic groups and might not reflect the experience of more granular groups (eg, Asian Indians, Filipinos, and Puerto Ricans) whose CVD prevalence has been reported to vary.23, 24
Although incident AMI hospitalization rates remain lower for APIs and Hispanics, compared with whites, the absolute burden (number of people hospitalized) of AMI hospitalization incidence for Hispanics and APIs increased over the study period. In contrast, the absolute burden of AMI hospitalizations for whites declined. The absolute burden for APIs and Hispanics increased, despite decreasing incidence rates. This observation is likely attributable to the rapid growth in population size for the underlying API and Hispanic populations and the slower growth for the white population, outweighing lower incidence rates for APIs and Hispanics, compared with whites. The AMI burden for APIs and Hispanics will likely continue to grow according to population size increases.
Studies of Medicare beneficiaries,15, 16 the ARIC (Atherosclerosis Risk in Communities) study,12 and an analysis of an all‐payer administrative database of hospitalizations in the United States11 examined race/ethnic differences in incidence and recurrent AMI hospitalization rates and observed smaller declines for blacks than whites. In our study, we observed similar annual declines in incidence rates during 2000 to 2009 for blacks and whites. However, the decline for blacks plateaued during 2010 to 2014, whereas the decline for whites during 2010 to 2014 continued according to the trajectory observed during 2000 to 2009.
Although slower declines in AMI hospitalizations among blacks might be attributable to less effective improvements in primary prevention of CVD for blacks than in primary prevention for whites, alternative explanations raise the possibility that slower declines might represent improvements in access and quality of care for blacks. This might occur if more blacks with AMIs survive long enough to be hospitalized.15 Hospitalized AMIs do not capture nonhospitalized AMIs, including out‐of‐hospital deaths. Blacks have a higher burden of CVD and its risk factors,25 more barriers to symptom recognition,26 and reduced access to heart disease treatment and health care compared with whites.25, 27 Therefore, blacks might be less likely than whites to be hospitalized for AMI and more likely to experience out‐of‐hospital AMI deaths. Reports of higher hospitalization rates and nonhospitalized first AMI or fatal coronary heart disease for blacks, compared with whites, support this hypothesis.28, 29
Among Medicare enrollees in Kaiser Permanente health plans in the western United States, differences in control of cardiovascular and diabetes mellitus risk factors between blacks and whites have decreased, with control becoming similar by 2011.30 Moreover, in our study, the higher rates of AMI incidence for whites compared with blacks were driven by STEMIs, which are more severe and deadlier than NSTEMIs. Although NSTEMI rates were similar for blacks and whites in 2000, NSTEMI rates were higher for blacks than whites starting in 2010. These observations are consistent with the possibility that blacks experienced a shift from out‐of‐hospital STEMI deaths to hospitalized STEMIs and a shift from STEMIs to NSTEMIs. Therefore, a plateauing decline in hospitalized AMIs during later study years for blacks might reflect reductions in healthcare access barriers and disease severity, increases in cardioprotective medications, or improved treatment of CVD risk factors for blacks.
Our findings require considerations. All people in our study had healthcare coverage through membership in an integrated, managed healthcare organization and might be healthier than the general population. In addition, the study population might have had better access to care than the general population and further benefited from increasingly standardized approaches to CVD prevention and management (eg, improved hypertension control).19, 20 Our results might not be generalizable to populations with less access to care; however, our study provides a unique opportunity to increase knowledge about the contribution of race/ethnicity to AMI cause in a setting where all people have healthcare coverage. Although people from all race/ethnic groups in this study have the same theoretical access to healthcare coverage because they are all insured with KPSC, we demonstrate that differences in AMI incidence rates persist. These differences might reflect genetic and other biological predispositions for AMI risk or barriers to healthcare use experienced by different race/ethnic groups.15, 31
Our study is limited by not capturing out‐of‐hospital fatal AMIs, which might indicate more severe disease or barriers to accessing care quickly. Other studies have observed greater declines in out‐of‐hospital fatal AMI than hospitalized AMI.9 Thus, declines in combined fatal out‐of‐hospital AMI and hospitalized AMI are likely to be steeper than the decline in hospitalized AMI alone. We did not account for secular changes in diagnostic sensitivity that might arise from increasing use of biomarkers (eg, serum troponin). Trends might be more dramatic than observed in this study because incidence during earlier years might be biased downward. Moreover, we could not assess AMI history before KPSC membership, which might have led to misclassification of some recurrent AMIs as first AMIs. However, because we included a 4‐year time in membership requirement, we were able to use a look‐back period of 4 years to reduce potential misclassification. Results from sensitivity analyses illustrated that varying the length of continuous membership time (1, 2, 4, and 8 years) did not change the trend of hospitalized AMI incidence rates during the study period. Moreover, most recurrent AMIs occur within the first year, with risk of recurrent AMI decreasing sharply after the second year.32
In summary, we observed substantial declines in incidence of hospitalized AMI across all race/ethnic groups during 2000 to 2014 (declines plateaued among blacks beginning in 2010) among a community‐based southern California population, likely caused in part by ongoing efforts to improve primary prevention and chronic disease care. Our results provide valuable insights into how AMI risk differs by race/ethnicity and can guide long‐term goals of KPSC and other healthcare communities to reduce AMI rates, potentially through identifying unmet needs in primary prevention for targeted interventions. Determining AMI risk for diverse populations will become increasingly important as the distribution of race/ethnicity shifts with the growth of race/ethnic minority populations.
Sources of Funding
This work was supported by the Southern California Permanente Medical Group.
Disclosures
Dr Chi completed this work while employed at the Centers for Disease Control and Prevention and Kaiser Permanente Southern California. She is currently employed by Genentech, Inc. Dr Reading completed this work while employed at Kaiser Permanente Southern California. She is currently employed by Amgen, Inc. Dr Reynolds has received research funding through her institution from Amgen, Inc, and Regeneron Pharmaceuticals, Inc. The remaining authors have no disclosures to report.
Supporting information
Table S1. Person‐Years Contributed by Each Race/Ethnic Group by Year, Kaiser Permanente Southern California, 2000–2014
Table S2. Characteristics of Persons Hospitalized for Non‐ST‐Segment Elevation Myocardial Infarction by Race/Ethnicity and Year, Kaiser Permanente Southern California, 2000–2014*
Table S3. Characteristics of Persons Hospitalized for ST‐Segment Elevation Myocardial Infarction by Race/Ethnicity and Year, Kaiser Permanente Southern California, 2000–2014*
Table S4. Crude and Age‐ and Sex‐standardized Incidence Rates of Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014
Table S5. Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years Among Women by Race/Ethnicity, Age Group, and Sex, Kaiser Permanente Southern California, 2000–2014
Table S6. Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years Among Men by Race/Ethnicity, Age Group, and Sex, Kaiser Permanente Southern California, 2000–2014
Table S7. Crude and Standardized Age‐ and Sex‐standardized Incidence of Non‐ST‐Segment Elevation Myocardial Infarction (NSTEMI) Hospitalizations per 100 000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014
Table S8. Crude and Age‐ and Sex‐standardized Incidence of ST‐Segment Elevation Myocardial Infarction (STEMI) Hospitalizations per 100,000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014
Acknowledgments
The authors thank the patients of Kaiser Permanente for helping to improve care through the use of information collected through our electronic health record systems. The authors thank Byron Robinson, PhD, for helpful insights and comments that greatly improved the article. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
(J Am Heart Assoc. 2020;9:e013542 DOI: 10.1161/JAHA.119.013542.)
Preliminary findings were previously presented at the Epidemic Intelligence Service Conference, April 24 to 27, 2017, in Atlanta, GA; and at the Council of State and Territorial Epidemiologists Conference, June 4 to 8, 2017, in Boise, ID.
References
- 1. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després J‐P, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Heart Turner MB. Disease and stroke statistics—2016 update. Circulation. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 3. Chen J, Normand S‐LT, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee‐for‐service beneficiaries. Circulation. 2010;121:1322–1328. [DOI] [PubMed] [Google Scholar]
- 4. Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Washington, DC: US Census Bureau ; 2014. [Google Scholar]
- 5. Koebnick C, Langer‐Gould AM, Gould MK, Chao CR, Iyer RL, Smith N, Chen W, Jacobsen SJ. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau Data. Perm J. 2012;16:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCormick N, Lacaille D, Bhole V, Avina‐Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One. 2014;9:e92286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reynolds K, Go AS, Leong TK, Boudreau DM, Cassidy‐Bushrow AE, Fortmann SP, Goldberg RJ, Gurwitz JH, Magid DJ, Margolis KL, McNeal CJ, Newton KM, Novotny R, Quesenberry CP, Rosamond WD, Smith DH, VanWormer JJ, Vupputuri S, Waring SC, Williams MS, Sidney S. Trends in incidence of hospitalized acute myocardial infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130:317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hechter RC, Qian L, Yan S, Luo Y, Krishnarajah G, Tseng H‐F. Impact of the change of copay policy in Medicare Part D on zoster vaccine uptake among Medicare beneficiaries in a managed care organization. BMC Health Serv Res. 2017;17:503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gerber Y, Weston SA, Jiang R, Roger VL. The changing epidemiology of myocardial infarction in Olmsted County, Minnesota, 1995–2012. Am J Med. 2015;128:144–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 11. Talbott EO, Rager JR, Brink LL, Benson SM, Bilonick RA, Wu WC, Han Y‐Y. Trends in acute myocardial infarction hospitalization rates for US States in the CDC tracking network. PLoS One. 2013;8:e64457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty‐two‐year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang OJ, Wang Y, Chen J, Krumholz HM. Recent trends in hospitalization for acute myocardial infarction. Am J Cardiol. 2012;109:1589–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sacks NC, Ash AS, Ghosh K, Rosen AK, Wong JB, Rosen AB. Trends in acute myocardial infarction hospitalizations: are we seeing the whole picture? Am Heart J. 2015;170:1211–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sacks NC, Ash AS, Ghosh K, Rosen AK, Wong JB, Cutler DM, Rosen AB. Recent national trends in acute myocardial infarction hospitalizations in Medicare: shrinking declines and growing disparities. Epidemiology. 2015;26:e46. [DOI] [PubMed] [Google Scholar]
- 16. Singh JA, Lu X, Ibrahim S, Cram P. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 2014;12:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Krumholz HM, Normand S‐LT, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130:966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Solomon MD, Leong TK, Rana JS, Xu Y, Go AS. Community‐based trends in acute myocardial infarction from 2008 to 2014. J Am Coll Cardiol. 2016;68:666–668. [DOI] [PubMed] [Google Scholar]
- 19. Kanter MH, Lindsay G, Bellows J, Chase A. Complete care at Kaiser Permanente: transforming chronic and preventive care. Jt Comm J Qual Patient Saf. 2013;39:484–494. [DOI] [PubMed] [Google Scholar]
- 20. Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systemic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol. 2014;30:544–552. [DOI] [PubMed] [Google Scholar]
- 21. Harrison TN, Scott RD, Cheetham TC, Chang S‐C, Hsu J‐WY, Wei R, Ling Grant DS, Boklage SH, Romo‐LeTourneau V, Reynolds K. Trends in statin use 2009–2015 in a large integrated health system: pre‐ and post‐2013 ACC/AHA guideline on treatment of blood cholesterol. Cardiovasc Drugs Ther. 2018;32:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goff DC, Nichaman MZ, Chan W, Ramsey DJ, Labarthe DR, Ortiz C. Greater incidence of hospitalized myocardial infarction among Mexican Americans than non‐Hispanic whites: the Corpus Christi Heart Project, 1988–1992. Circulation. 1997;95:1433–1440. [DOI] [PubMed] [Google Scholar]
- 23. Palaniappan LP, Araneta MRG, Assimes TL, Barrett‐Connor EL, Carnethon MR, Criqui MH, Fung GL, Narayan KMV, Patel H, Taylor‐Piliae RE, Wilson PWF, Wong ND; American Heart Association Council on Epidemiology and Prevention, American Heart Association Council on Peripheral Vascular Disease, American Heart Association Council on Nutrition, Physical Activity, and Metabolism, American Heart Association Council on Clinical Cardiology, American Heart Association Council on Cardiovascular Nursing, Council on Cardiovascular Nursing . Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation. 2010;122:1242–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Daviglus ML, Talavera GA, Avilés‐Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil‐Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Leigh JA, Alvarez M, Rodriguez CJ. Ethnic minorities and coronary heart disease: an update and future directions. Curr Atheroscler Rep. 2016;18:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Swanoski MT, Lutfiyya MN, Amaro ML, Akers MF, Huot KL. Knowledge of heart attack and stroke symptomology: a cross‐sectional comparison of rural and non‐rural US adults. BMC Public Health. 2012;12:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shippee TP, Ferraro KF, Thorpe RJ. Racial disparity in access to cardiac intensive care over 20 years. Ethn Health. 2011;16:145–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, Lewis CE, Gamboa C, Cushman M, Howard V, Howard G; REGARDS Investigators . Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare Advantage plans. N Engl J Med. 2014;371:2288–2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lanza GA. Ethnic variations in acute coronary syndromes. Heart. 2004;90:595–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gulliksson M, Wedel H, Köster M, Svärdsudd K. Hazard function and secular trends in the risk of recurrent acute myocardial infarction: 30 years of follow‐up of more than 775,000 incidents. Circ Cardiovasc Qual Outcomes. 2009;2:178–185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Person‐Years Contributed by Each Race/Ethnic Group by Year, Kaiser Permanente Southern California, 2000–2014
Table S2. Characteristics of Persons Hospitalized for Non‐ST‐Segment Elevation Myocardial Infarction by Race/Ethnicity and Year, Kaiser Permanente Southern California, 2000–2014*
Table S3. Characteristics of Persons Hospitalized for ST‐Segment Elevation Myocardial Infarction by Race/Ethnicity and Year, Kaiser Permanente Southern California, 2000–2014*
Table S4. Crude and Age‐ and Sex‐standardized Incidence Rates of Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014
Table S5. Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years Among Women by Race/Ethnicity, Age Group, and Sex, Kaiser Permanente Southern California, 2000–2014
Table S6. Acute Myocardial Infarction Hospitalizations per 100 000 Person‐Years Among Men by Race/Ethnicity, Age Group, and Sex, Kaiser Permanente Southern California, 2000–2014
Table S7. Crude and Standardized Age‐ and Sex‐standardized Incidence of Non‐ST‐Segment Elevation Myocardial Infarction (NSTEMI) Hospitalizations per 100 000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014
Table S8. Crude and Age‐ and Sex‐standardized Incidence of ST‐Segment Elevation Myocardial Infarction (STEMI) Hospitalizations per 100,000 Person‐Years by Race/Ethnicity, Kaiser Permanente Southern California, 2000–2014


