Abstract
Cancer stem cells are responsible for tumorigenesis, progression, recurrence and metastasis. Intestinal stem cells (ISCs) are regarded as the origin of intestinal neoplasia. Inflammation also serves an important role in intestinal neoplasia. To explore the molecular mechanisms underlying the inflammation-mediated induction of intestinal tumorigenesis, the present study investigated the function of tumor necrosis factor (TNF)-α in the malignant transformation of ISCs. NCM460 spheroid (NCM460s) cells with higher expression of stem cell genes, such as Oct4, Nanog, Sox2 and Lgr5, and with a higher ratio of CD133+, were obtained from NCM460 cells in serum-free medium. TNF-α accelerated cell proliferation, migration and invasion, induced chemotherapy resistance and the epithelial-mesenchymal transition. NF-κB and Wnt/β-catenin pathways were activated in TNF-α-induced inflammatory responses, leading to the nuclear translocation of p65 and β-catenin, as well as promoter activity of NF-κB and TCF/LEF transcription factors. It was further demonstrated that TNF-α-induced activation of the NF-κB and Wnt/β-catenin signaling pathways, as well as the upregulation of proinflammatory cytokines, were significantly suppressed by p65-knockdown. Notably, PDTC, an inhibitor of NF-κB signaling, reversed TNF-α-induced activation of the NF-κB and Wnt/β-catenin pathways. A similar role was observed for IWP-2, an inhibitor of Wnt/β-catenin signaling. Collectively, these results demonstrated that the NF-κB and Wnt/β-catenin pathways were activated to promote TNF-α-induced malignant transformation of ISCs, in which these two pathways cross-regulated each other.
Keywords: TNF-α, NF-κB pathway, Wnt/β-catenin pathway, malignant transformation, intestinal stem cells
Introduction
Cancer is a major public health problem worldwide and colorectal cancer is one of the leading causes of cancer-associated mortality (1). In spite of the considerable progress in cancer therapeutics, tumor relapse and metastasis remain a major clinical challenge (2). Numerous studies have suggested that there is a rare subpopulation of poorly-differentiated cancer cells, cancer stem cells (CSCs), that are responsible for tumorigenesis, progression, recurrence and metastasis (3,4). It has been demonstrated that CSCs possess self-renewal properties, tumor initiation capability, a high proliferation rate and differentiation potential (5). CSC populations are associated with chemoradiotherapy resistance and relapse potential after successful treatment, leading to the unfavorable outcomes for patients (6).
It is well known that there are small populations of adult stem cells existing in various tissues, such as the lung, ovaries, intestines, skin and mammary gland (3,7,8), which have high proliferative capacity. Adult stem cells possess self-renewal abilities and multilineage differentiation potential to maintain tissue homeostasis and repair injured tissues (9,10). However, dysregulation in the mechanisms underlying proliferation and differentiation initiates the malignant transformation of adult stem cells leading to tumorigenesis (11). Previous studies have demonstrated that intestinal stem cells (ISCs) are the origin of intestinal neoplasia (8,12,13). Thus, it was hypothesized that ISCs are the origin of intestinal CSCs, sustaining tumorigenesis and progression. Resolving the molecular mechanisms underpinning the malignant transformation of ISCs to intestinal CSCs may help identify novel targets for colorectal cancer treatment.
Accumulating evidence suggests that inflammation, particularly chronic inflammation, serves an important role in intestinal neoplasia (14–17). Chronic inflammation has been revealed to promote the hyperactivation of signaling pathways involved in the regulation of ISCs, including Wnt/β-catenin, PI3K/AKT/mTOR, NF-κB, STAT3 and Notch (14,15,18). Then, ISCs undergo genomic alteration and aggressive proliferation, which eventually transforms normal stem cells into intestinal CSCs to initiate intestinal tumorigenesis (15). Recent studies have demonstrated that the crosstalk between the NF-κB and Wnt/β-catenin signaling pathways may regulate the progression of colorectal cancer in inflammatory responses (19,20). Therefore, it is necessary to elucidate the molecular mechanisms underlying the malignant transformation of ISCs in inflammatory responses.
The present study focused on the impact of proinflammatory cytokine tumor necrosis factor (TNF)-α on human ISCs. The results indicated that TNF-α induced the activation of the NF-κB and Wnt/β-catenin pathways to promote the malignant transformation of ISCs, such as increasing proliferation, colony formation, chemotherapeutic resistance, migration and invasion. It was further demonstrated that these two signaling pathways cross-regulated each other in TNF-α-induced malignant transformation of ISCs.
Materials and methods
Cell culture
The human normal colon epithelial cell line NCM460 was purchased from Ginio Biotechnology Corporation. Cells were cultured in DMEM-High Glucose medium (Gibco; Thermo Fisher Scientific, Inc.), supplemented with 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin-streptomycin at 37°C and 5% CO2 in a humidified atmosphere. For the sphere culture, single NCM460 cells were transferred in serum-free DMEM/F12 medium (Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10 ng/ml bFGF (PeproTech, Inc.), 20 ng/ml EGF (PeproTech, Inc.), 5 mg/ml insulin (MCE), 0.4% BSA (Beijing Solarbio Science & Technology Co., Ltd.) and 2% B27 Supplements (Gibco; Thermo Fisher Scientific, Inc.).
NCM460 spheroid (NCM460s) cells were collected using natural sedimentation at 37°C for 5 min. NCM460s cells were enzymatically dissociated, resuspended, and then seeded at 2×104 cells per well in serum-free medium (SFM) in 6-well ultra-low attachment culture dishes (Corning, Inc.). Cells were treated with 0–100 ng/ml TNF-α (PeproTech, Inc.) for various durations (12, 24, 48 and 72 h) at 37°C to induce an inflammatory response.
Differentiation assay
To evaluate the differentiation ability of NCM460s cells from SFM, the 50 NCM460 spheres with >100 µm diameter were collected and re-cultured for 48 h on a collagen-coated 35-mm dish in DMEM-High Glucose medium (Gibco; Thermo Fisher Scientific, Inc.), supplemented with 10% fetal bovine serum (FBS) (Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin-streptomycin at 37°C and 5% CO2 in a humidified atmosphere.
Antibodies and reagents
Specific primary antibodies to IKKβ (product no. 8943), phospho-IKKα/β (Ser176/180; cat. no. 2697), IκBα (cat. no. 9242), phospho-IκBα (Ser32/36; cat. no. 9246), NF-κB p65 (cat. no. 8242), phospho-NF-κB p65 (Ser536; cat. no. 3033), TNF-α (cat. no. 8184), APC (cat. no. 2504), GSK-3β (cat. no. 12456), phospho-GSK-3β (Ser9; cat. no. 9323), β-catenin (cat. no. 8480), phospho-β-catenin (Ser33/37/Thr41; cat. no. 9561), c-Myc (cat. no. 13987), cyclin D1 (cat. no. 2978), E-cadherin (cat. no. 3195), N-cadherin (cat. no. 13116), vimentin (cat. no. 5741), Snail (cat. no. 3879) and Nanog (cat. no. 3580) were obtained from Cell Signaling Technology, Inc. Antibodies to Lgr5 (cat. no. ab75732), Oct4 (cat. no. ab137427) and Sox2 (cat. no. ab97959) were obtained from Abcam. PE Mouse Anti-Human CD133 antibody (cat. no. 566593), PE Mouse IgG1, κ Isotype Control (cat. no. 554680) and 7-AAD (cat. no. 559925) were obtained from BD Biosciences. The NF-κB inhibitor pyrrolidine dithiocarbamate (PDTC; cat. no. M4005) and Wnt inhibitor IWP-2 (cat. no. M2237) were purchased from Abmole (Abmole Bioscience, Inc.). Lipofectamine 3000 transfection reagent was obtained from Invitrogen; Thermo Fisher Scientific, Inc.
Flow cytometric analysis
For the detection of surface markers in colon cancer stem cells, cells (1×106 cells) were collected, incubated with human anti-CD133-PE antibodies (1:20 dilution; BD Biosciences) at room temperature in the dark for 30 min. Dead cells were excluded using 7-AAD staining (1:20 dilution; BD Biosciences) at room temperature for 10 min. Cells were analyzed using a flow cytometer (BD Biosciences), and the isotype IgG2b (1:20 dilution; BD Biosciences) was used as the control.
For the cell cycle analysis, cells were pipetted, washed twice with PBS and fixed in 70% ethanol at 4°C overnight. Cells were centrifuged at 4,000 rpm for 10 min, re-suspended and stained with PI (BD Biosciences) at 4°C for 30 min. Then, samples were also analyzed using a flow cytometer (BD Biosciences).
Cell Counting Kit-8 (CCK-8) assay
Cell viability was analyzed using a CCK-8 assay according to the manufacturer's instructions (Boshide). Cells were seeded into a 96-well plate at 5×103 cells/well with 100 µl culture medium which contained the various TNF-α concentrations (0, 0.01, 0.1, 1, 10, 50 and 100 ng/ml). Cell viability was quantified by the addition of 10 µl CCK-8 solution. After 2 h of incubation at 37°C, the absorption was analyzed at 450 nm using a Multiskan plate reader (Thermo Fisher Scientific, Inc.).
The chemotherapy sensitivity assay to 5-FU (Sigma-Aldrich; Merck KGaA) was also evaluated using CCK-8 assay kit as aforementioned.
Soft-agar sphere-formation assay
The 6-well plates were loaded with 2 ml 0.6% soft agarose. Then, 2 ml 0.375% soft agarose containing 1×104 cells were added on the lower agarose. After 2 weeks of incubation, the cell spheres were stained with 0.005% crystal violet at room temperature for 1 h. The number of spheres with >100 µm diameter in each well were counted using an inverted fluorescence microscope (magnification, ×100; Olympus Corp.) to analyze the sphere formation capacity.
Colony formation assay
Cells (1×103 cells) were plated in 35-mm culture dishes and cultured for 2 weeks. After staining with 0.1% crystal violet at room temperature for 30 min. The number of colonies with >1 mm diameter was counted using an inverted fluorescence microscope (magnification, ×40; Olympus Corp.) to analyze the colony formation capacity.
Cell migration and invasion assay
Cell migration and invasion assays were performed as previously described (21). In brief, cell suspensions containing 2×104 cells in 200 µl SFM were added into 24-well plates with 8.0-µm upper Transwell chambers (BD Biosciences) pre-coated without or with Matrigel (Sigma-Aldrich; Merck KGaA) for migration or invasion assays, respectively, and lower chambers were filled with 800 µl medium with 15% FBS. After a 24 h incubation, the migrating and invading cells were stained with 0.1% crystal violet solution at room temperature for 30 min and then counted in five random microscopic fields using an inverted fluorescence microscope (magnification, ×200; Olympus Corp.).
Reverse transcription-quantitative (RT-q) PCR
Total RNA was purified using TRIzol® reagent (Beyotime Institute of Biotechnology) according to a standard protocol (22). The concentration and quality of all the RNA samples were valuated using a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific, Inc.). Then, 1 µg of total RNA was used to synthesize cDNA for the subsequent reverse transcription with the Reverse Transcription kit (Takara Biotechnology, Co., Ltd.) according to the manufacturer's instructions. Quantitative PCR was performed using the SYBR Green PCR Master Mix kit (Takara Biotechnology, Co., Ltd.) on a qPCR detection system (Bio-Rad Laboratories, Inc.). The qPCR thermocycling conditions were as follows: Initial denaturation for 3 min at 95°C followed by 40 cycles of denaturation for 15 sec at 95°C, annealing for 30 sec at 60°C and extension for 30 sec at 72°C. The data were analyzed using the 2−ΔΔCq method (23) and reported as the fold-change in gene expression normalized to the expression of the endogenous control gene GAPDH. The sequences of primers used are listed in Table SI.
Western blot analysis
After appropriate treatments, cells were harvested and total cellular proteins were extracted for western blot analysis. In addition, the nuclear and cytoplasmic proteins were extracted using a Nuclear and Cytoplasmic Protein Extraction kit (Sangon Biotech Co., Ltd.) according to the manufacturer's instructions. Protein concentrations were measured using a BCA Protein Assay kit (Nanjing KeyGen Biotech Co., Ltd.). Proteins (30 µg/lane) were separated by gel electrophoresis on 8–10% SDS-PAGE and then transferred onto PVDF membranes (EMD Millipore). After blocking with 5% non-fat milk at room temperature for 2 h, the PVDF membranes were incubated with primary antibodies at 4°C overnight. Membranes were incubated with horseradish peroxidase-labelled secondary goat anti-rabbit antibody (1:10,000; ProteinTech Group, Inc.) for 2 h. Proteins were examined by enhanced chemiluminescence (ECL) detection kit (Nanjing KeyGen Biotech Co., Ltd.), and then the signals were visualized and analyzed using the ImageJ v5.2.1 Software (Bio-Rad Laboratories, Inc.).
Immunofluorescence staining
Expression levels of p65 and β-catenin were detected using immunofluorescence staining. Spheres were fixed in 4% paraformaldehyde at room temperature for 20 min, blocked in blocking buffer (PBS+2% BSA+0.3% Triton-100) at room temperature for 1 h, and incubated with primary antibodies against p65 and β-catenin (1:200, rabbit) at 4°C overnight. Cells were then treated at room temperature with FITC-conjugated secondary antibody (Boster Biological Technology) for 1 h and DAPI (Beyotime Institute of Biotechnology) for 30 min. Fluorescent signals were visualized using a Leica fluorescence microscope (magnification, ×200; Leica Microsystems GmbH).
Dual-luciferase reporter assay
The cells were co-transfected with a pGL4.32 vector (Promega Corporation) containing the NF-κB reporter construct or a pGL4.49 vector (Promega Corporation) containing the TCF/lymphoid enhancer-binding factor 1 (LEF) reporter construct linked to a firefly luciferase reporter plasmid, and with a pRL-TK Renilla luciferase reporter gene (Promega Corporation). The luciferase activities were measured using a Dual-Luciferase Reporter Assay system (Promega Corporation) and normalized as a relative ratio of luciferase to Renilla luciferase activities according to the manufacturer's protocol.
Lentiviral transfection of spheroid cells
Lentiviral vectors bearing p65 short hairpin (sh)RNA and control non-targeting shRNA were synthesized by Shanghai GeneChem Co., Ltd. Cells were seeded in 6-well plates at a density of 3×105 cells/well and cultured at 37°C and 5% CO2 in a humidified atmosphere overnight. NCM460s cells were transfected with 100 nM p65 shRNA or control shRNA using Lipofectamine™ 3000 transfection reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. After 12 h of incubation, the medium was replaced with normal SFM under suspension conditions. After 5 days of transfection, the effect of p65 shRNA was examined using RT-qPCR and western blotting. Then, the transfected cells were passaged for further experiments.
Statistical analysis
All data were analyzed using SPSS v20.0 (IMB Corp.). The results were presented as the mean ± standard deviation from at least three independent experiments. Differences between two groups were analyzed using unpaired Student's t-tests. One-way ANOVA followed by Tukey's post hoc test was used to analyze differences in multiple groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Intestinal stem cells are enriched upon spheroidal culture in SFM
Human normal intestinal epithelial cells, NCM460 cells, formed spheres and the diameters increased gradually when cultured in SFM under suspension conditions (Fig. 1A). NCM460s cells could be passaged >30 times in SFM under suspension conditions, indicating that they possessed the self-renewal ability. Moreover, NCM460s cells could be induced to differentiate into epithelial-like cells when cultured in DMEM medium supplemented with 10% FBS (Fig. S1).
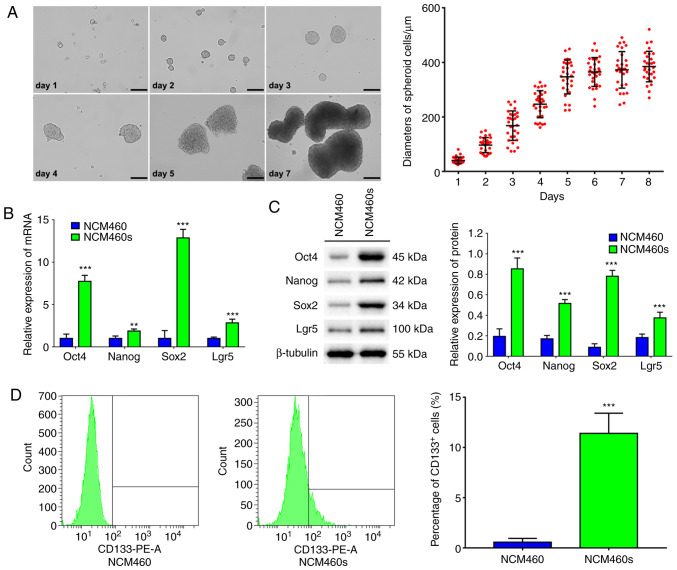
Figure 1.
Human normal intestinal epithelial cells NCM460s with the characteristics of stem cells are enriched upon spheroidal culture in SFM under suspension conditions. (A) NCM460s cells were directly generated from NCM460 adherent cells in SFM under suspension conditions. Scale bar, 100 µm. (B) Relative mRNA levels and (C) relative protein levels of stem cell genes Oct4, Nanog, Sox2 and Lgr5 in NCM460 cells and NCM460s cells were detected by RT-qPCR and western blotting. (D) Flow cytometric analysis revealed the proportion of CD133+ in NCM460 cells and NCM460s cells. **P<0.01, ***P<0.001 compared with NCM460 cells. SFM, serum-free medium. NCM460s, NCM460 spheroid.
In order to validate the stemness of NCM460s cells, the stem cell genes were analyzed using qPCR, western blotting and flow cytometric analysis. Results indicated that NCM460s cells exhibited higher mRNA and protein expression of stem cell genes such as Oct4, Nanog and Sox2 (24) and Lgr5, a marker gene of intestinal stem cells (13), compared with those in NCM460 adherent cells (Fig. 1B and C). Furthermore, flow cytometric analysis revealed that the ratio of CD133+ cells (one of the specific surface markers in colorectal CSCs) was <1% in NCM460 adherent cells, but reached 11.40% in NCM460s cells (Fig. 1D). These results indicated that serum-free suspension culture is an effective strategy to enrich NCM460s cells with stem cell characteristics from normal intestinal epithelial NCM460 cells.
TNF-α promotes the malignant transformation of NCM460s cells
When NCM460s cells were treated with 0–100 ng/ml TNF-α for various time-points (12, 24, 48 and 72 h), the viability of NCM460s cells was affected in a dose-dependent and time-dependent manner. Treatment with 1 ng/ml TNF-α for 24 h resulted in the maximum increase of the viability of NCM460s cells (Fig. S2). Therefore, all further experiments investigating malignant transformation were conducted for this duration.
To evaluate the impact of TNF-α on chemotherapy sensitivity, cells were exposed to 5-FU at various concentrations (0, 0.1, 1, 5, 10, 50 and 100 µg/ml) for 48 h. Then, the viabilities were analyzed at the indicated concentration of 5-FU using a CCK-8 assay. The results revealed that the survival rates of NCM460s cells were significantly increased at each concentration of 5-FU upon TNF-α treatment, suggesting that TNF-α increased chemotherapy resistance (Fig. 2A).
Figure 2.
TNF-α promotes the malignant transformation of human normal intestinal stem cells NCM460s. NCM460s cells were treated with 1 ng/ml TNF-α for 24 h, and then compared with NCM460 adherent cells. (A) TNF-α increased the survival rates of NCM460s cells in various concentrations of 5-FU by the CCK-8 assay. (B) TNF-α increased the capacity of colony formation of NCM460s cells in (a) colony formation assay and (b) soft agar assay. Scale bar, 100 µm. (C) TNF-α induced changes of the cell cycle distribution in NCM460s cells as revealed by flow cytometry. (D) TNF-α increased the (a) migratory and (b) invasive number of NCM460s cells in the Transwell assay. Scale bar, 50 µm. (E) TNF-α reduced the protein level of E-cadherin and increased the protein levels of N-cadherin, Vimentin and Snail as revealed by western blotting. (F) TNF-α induced an increased proportion of surface marker gene CD133+ in NCM460s cells as revealed by flow cytometry. *P<0.05, **P<0.01, ***P<0.001 compared with NCM460s cells without TNF-α stimulation. TNF, tumor necrosis factor; NCM460s, NCM460 spheroid; ns, not significant.
The effect of TNF-α on the proliferation ability of NCM460s cells was assessed using a colony formation and soft agar assay. The results revealed that TNF-α significantly increased the colony formation capacity of NCM460s cells (Fig. 2B). In order to explore the underlying mechanism associated with these phenotypic changes, the impact of TNF-α on NCM460s cell distribution in the cell cycle was investigated using flow cytometry. It was reported that TNF-α significantly reduced the proportion of cells in the G0-G1 phase and increased the proportion of cells in the S phase (Fig. 2C). These data revealed that TNF-α increased the proliferative capacity of NCM460s cells.
Since the epithelial-mesenchymal transition (EMT) is a key process in cancer metastasis, the impact of TNF-α on the migratory and invasive abilities of NCM460s cells was examined using Transwell assays. It was demonstrated that TNF-α significantly increased the capacities of migration and invasion of NCM460s cells (Fig. 2D). In addition, western blotting revealed that TNF-α decreased the expression of the epithelial marker E-cadherin, and concurrently increased the expression of mesenchymal markers, including N-cadherin, vimentin and transcription factor Snail, in NCM460s cells (Fig. 2E). These data revealed that TNF-α induced EMT to promote the migration and invasion capacities of NCM460s cells.
To further characterize the malignant transformation of NCM460s cells, the effect of TNF-α on the proportion of CD133+ cells was investigated using flow cytometry. A significantly increased proportion of CD133+ cells was revealed, from 11.40% in NCM460s cells to 28.00% in the TNF-α-treated NCM460s cells, indicating that TNF-α induced the phenotypic change from NCM460s cells to CSCs (Fig. 2F). Collectively, these results indicated that TNF-α induced the malignant transformation of NCM460s cells.
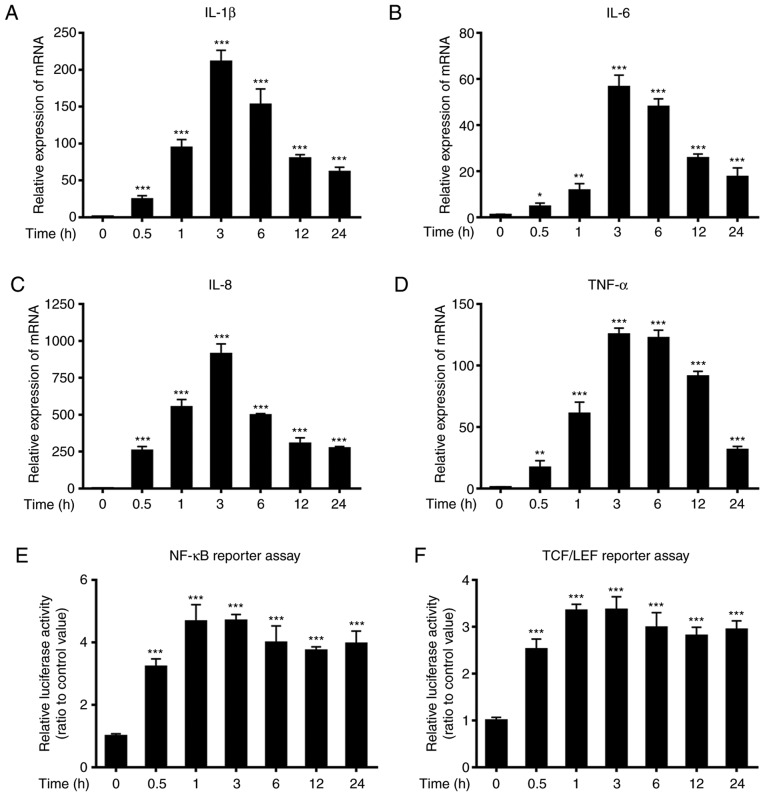
TNF-α induces inflammatory responses and initiates activation of the NF-κB and Wnt/β-catenin signaling pathways
When NCM460s cells were exposed to 1 ng/ml TNF-α for various time-points, the relative mRNA expression levels of the proinflammatory cytokines interleukin (IL)-1β, IL-6, IL-8 and TNF-α were significantly upregulated at 0.5 h after TNF-α stimulation compared with those of the untreated control, and reached peak levels ~3 h after stimulation (Fig. 3A-D). The promoter activities of the NF-κB and TCF/LEF transcription factors were also significantly increased at 0.5 h after TNF-α stimulation relative to those of the untreated control, and reached peak levels 1–3 h after stimulation (Fig. 3E-F).
Figure 3.
TNF-α induces inflammatory responses and the increased activities of responsive promoters in NF-κB and Wnt/β-catenin pathways. NCM460s cells were treated with 1 ng/ml TNF-α for various time-points ranging from 0 to 24 h. (A-D) The relative mRNA expression of the proinflammatory cytokines IL-1β, IL-6, IL-8 and TNF-α were examined by RT-qPCR, and all results were normalized to those in untreated cells. (E and F) Dual Luciferase reporter assays were conducted to analyze the effect of TNF-α to the NF-κB promoter activity and TCF/LEF promoter activity. *P<0.05, **P<0.01, ***P<0.001 compared with NCM460s cells without TNF-α stimulation. TNF, tumor necrosis factor; NCM460s, NCM460 spheroid; IL, interleukin.
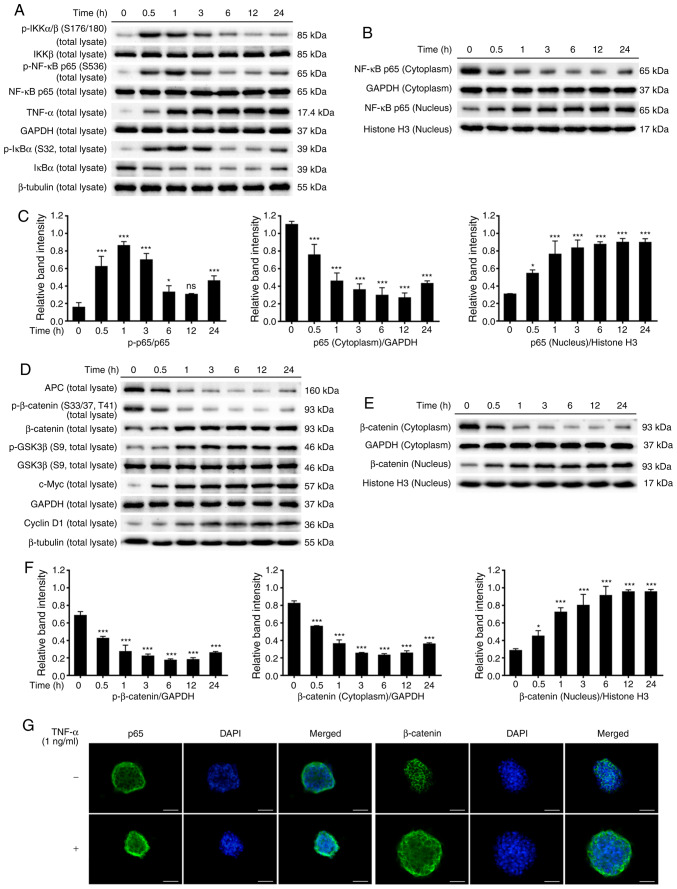
Phosphorylation of IκB kinase complex α/β (IKKα/β) was increased at 0.5 h after TNF-α stimulation relative to the untreated control. Moreover, the phosphorylation of IκBα was upregulated however, the protein levels of IκBα were downregulated at 0.5 h after stimulation relative to the untreated control, while TNF-α levels were increased. p65 is an essential subunit of the NF-κB complex and is key for the regulation of inflammatory responses. TNF-α increased the phosphorylation of p65 and induced the nuclear translocation of p65 (Fig. 4A-C).
Figure 4.
TNF-α induces the activation of the NF-κB and Wnt/β-catenin pathways. NCM460s cells were treated with 1 ng/ml TNF-α for various time-points ranging from 0 to 24 h. Western blotting was used to analyze the protein levels of the NF-κB and Wnt/β-catenin pathways in the total cell extracts and the nuclear/cytoplasmic extracts. (A and B) Representative blots of the NF-κB pathway. (C) The relative levels of p65 phosphorylation in the total cell extracts and p65 protein levels in the nuclear/cytoplasmic extracts. (D and E) Representative blots of the Wnt/β-catenin pathway. (F) The relative levels of β-catenin phosphorylation in the total cell extracts and β-catenin protein levels in the nuclear/cytoplasmic extracts. (G) NCM460s cells were exposed to 1 ng/ml TNF-α for 24 h, and immunofluorescence staining was used to detect the localization of p65 and β-catenin in NCM460s cells. The nuclei were stained with DAPI. Scale bar, 50 µm. *P<0.05, ***P<0.001 compared with NCM460s cells without TNF-α stimulation. TNF, tumor necrosis factor; NCM460s, NCM460 spheroid; ns, not significant.
Conversely, TNF-α decreased the protein levels of APC, while increasing glycogen synthase kinase (GSK)3β phosphorylation at 0.5–1 h after stimulation. Phosphorylation of β-catenin was downregulated and the protein levels of total β-catenin were upregulated at 0.5 h after stimulation. The expression of β-catenin was markedly reduced in the cytoplasm but gradually increased in the nucleus. In addition, the expression of downstream Wnt target genes c-Myc and cyclin D1 were increased after TNF-α stimulation (Fig. 4D-F).
To further elucidate the molecular mechanisms by which TNF-α induced the activation of the NF-κB and Wnt/β-catenin pathways, immunofluorescence staining was used to observe the distribution of p65 and β-catenin in NCM460s cells. Exposure of NCM460s cells to TNF-α for 24 h reduced the expression of p65 and β-catenin in the cytoplasm but increased their expression in the nucleus, indicating that TNF-α induced the translocation of p65 and β-catenin from the cytoplasm to the nucleus (Fig. 4G). These findings demonstrated that the NF-κB and Wnt/β-catenin pathways were activated in TNF-α-induced inflammatory responses in NCM460s cells.
NF-κB and Wnt/β-catenin pathways cross-regulate each other in TNF-α-induced NCM460s cells
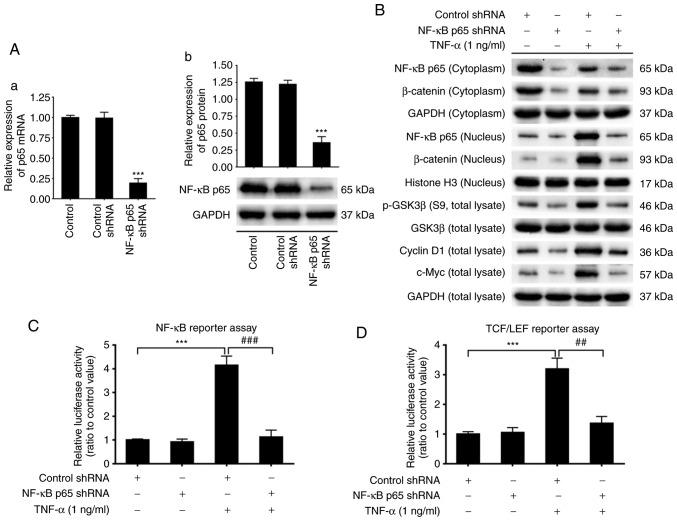
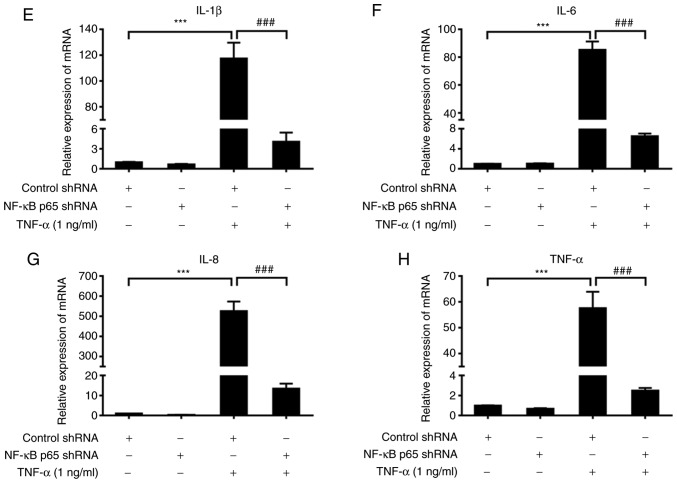
To elucidate the potential molecular mechanisms of TNF-α-induced malignant transformation in NCM460s cells, p65 shRNA was used to knockdown the activity of NF-κB signaling. The effect of p65 shRNA transfection on p65 expression was evaluated using qPCR and western blotting. The results revealed that the mRNA and protein levels of total p65 were considerably suppressed by p65 shRNA transfection (Fig. 5A), indicating that the p65 gene expression was successfully knocked down.
Figure 5.
Effects of p65 knockdown on the activities of NF-κB and Wnt/β-catenin signaling pathways and the expression of proinflammatory cytokines in TNF-α-induced NCM460s cells. NCM460s cells were transfected with control shRNA or p65 shRNA for 24 h, and treated with 1 ng/ml TNF-α for 3 h. (A) The effects of p65 knockdown on the (a) mRNA and (b) protein expression levels of p65 in NCM460s cells. (B) The effects of p65 knockdown on the activities of the NF-κB pathway and Wnt/β-catenin pathway in TNF-α-induced NCM460s cells. (C and D) The effects of p65 knockdown on the NF-κB promoter activity and TCF/LEF promoter activity. (E-H) The effects of p65 knockdown on the mRNA expression of proinflammatory cytokines (E) IL-1β, (F) IL-6, (G) IL-8 and (H) TNF-α in TNF-α-induced NCM460s cells. ***P<0.001 compared with control shRNA group; ##P<0.01 and ###P<0.001 compared with control shRNA + TNF-α. TNF, tumor necrosis factor; NCM460s, NCM460 spheroid; IL, interleukin.
Protein expression of p65 in the cytoplasm, which was downregulated by TNF-α, remained at a low level by p65 shRNA. Protein expression of p65 in the nucleus, which was upregulated by TNF-α, was also downregulated by p65 shRNA (Fig. 5B). These results indicated that p65 knockdown blocked the protein expression of total p65 and suppressed the nuclear translocation of p65, both of which were promoted by TNF-α treatment. NF-κB promoter activity, which was markedly increased by TNF-α, was also significantly downregulated to almost basal levels by p65 shRNA (Fig. 5C). Notably, TNF-α-induced activation of the Wnt/β-catenin pathway, including increased expression of GSK3β phosphorylation, protein levels of c-Myc and cyclin D1 and the translocation of β-catenin from the cytoplasm to the nucleus, were all suppressed by p65 shRNA (Fig. 5B). TCF/LEF promoter activity, which was significantly upregulated by TNF-α, was significantly suppressed to almost basal levels by p65 shRNA (Fig. 5D). Similarly, mRNA expression of proinflammatory cytokines IL-1β, IL-6, IL-8 and TNF-α, which were significantly increased by TNF-α, were also blocked by p65-knockdown (Fig. 5E-H).
To further explore the molecular basis for the cross-regulation between the NF-κB and Wnt/β-catenin pathways in the TNF-α-induced malignant transformation of NCM460s cells, two inhibitors were used to examine the protein levels of signaling molecules associated with these two pathways. When NCM460s cells were incubated with PDTC, an inhibitor of NF-κB signaling, TNF-α-induced translocation of p65 from the cytoplasm to the nucleus was reversed in a dose-dependent manner. Notably, PDTC counteracted TNF-α-induced activation of the Wnt/β-catenin pathway in NCM460s cells, including the increased phosphorylation of GSK3β and β-catenin, as well as the increased protein levels of c-Myc and nuclear translocation of β-catenin (Fig. 6A). Furthermore, as an inhibitor of Wnt processing and secretion, IWP-2 prevented TNF-α-induced nuclear translocation of β-catenin in a dose-dependent manner. Notably, IWP-2 also counteracted TNF-α-induced activation of the NF-κB pathway in NCM460s cells, including increased phosphorylation of IKKα/β and IκBα, decreased protein levels of IκBα and nuclear translocation of p65 (Fig. 6B). Collectively, these results indicated that NF-κB and Wnt/β-catenin pathways cross-regulated each other in TNF-α-induced NCM460s cells.
Figure 6.
Effects of inhibitors of the NF-κB and Wnt/β-catenin pathways on their activities in TNF-α-induced NCM460s cells. NCM460s cells were respectively incubated with 1, 10, 100 µM of (A) PDTC or (B) IWP-2 without or with 1 ng/ml TNF-α for 3 h. Western blotting was used to analyze the protein expression of genes related with NF-κB and Wnt/β-catenin signaling in the total cell extracts and the nuclear/cytoplasmic extracts. TNF, tumor necrosis factor; NCM460s, NCM460 spheroid; PDTC, pyrrolidine dithiocarbamate; IKKα/β, IκB kinase complex α/β; GSK, glycogen synthase kinase.
Discussion
Stem cells are characterized by their self-renewal capacity and potential for multilineage differentiation. Normal stem cells serve a critical role in injury, disease and regular maintenance. Unfortunately, genetic alterations of tumor-initiating cells drive the acquisition of oncogenic mutations through the interactions with abnormal environmental elements (12,16). In most cases, one mutation is insufficient and at least four to five genetic mutations are required for tumor initiation (25). It is imperative that oncogenic mutations only accumulate in long-lived but quiescent stem cells rather than in differentiated cells, which are rapidly eliminated before the next mutation occurs (16,25). Notably, dysregulation in the mechanisms underlying proliferation and differentiation initiates the malignant transformation of normal stem cells, leading to tumorigenesis (11). CSCs are responsible for tumor initiation, progression, recurrence and metastasis, and can differentiate into all cell types in cancer tissues (3,4). The similar biological properties between normal stem cells and CSCs are the basis of a recent hypothesis that CSCs originate from normal stem cells. Furthermore, studies have demonstrated that ISCs are the origin of intestinal neoplasia (8,12,13). Barker et al (26) and Leung et al (27), reported that Lgr5-positive crypt base columnar cells, which are often located adjacent to Paneth cells, could generate all epithelial lineages, suggesting that Lgr5-positive crypt base columnar cells were stem cells of the normal small intestine and colon. Using mouse models, Lgr5-positive ISCs were identified as the origin cells of intestinal neoplasia and were found to accelerate tumor progression (13). Thus, ISCs are considered to be the origin of intestinal CSCs and sustain tumorigenesis and progression.
Recently, it was demonstrated that spheroid cells derived from cancer cell lines in SFM under suspension conditions had increased expression of stemness-associated genes (3,10,12,28). As one effective strategy to enrich rare CSCs, serum-free suspension culture has been widely used to isolate several types of CSCs, including breast (6), ovarian (11), colorectal (3,29) and lung cancer (30). A number of human colorectal cancer cell lines, including HT29, SW480, DLD-1 and HCT116, can form spheres under serum-free suspension culture conditions (27,28). In this present study, NCM460 cells formed spheres when cultured under SFM suspension conditions. NCM460s cells exhibited higher mRNA and protein expression compared with those in NCM460 adherent cells, such as stem cell genes Oct4, Nanog, Sox2 and Lgr5, a marker gene of intestinal stem cells. Furthermore, the proportion of CD133+ cells, a colorectal CSC-specific surface marker, was significantly increased in NCM460s cells compared with NCM460 adherent cells. Thus, serum-free suspension culture is a highly efficient method to enrich NCM460s cells with stem cell characteristics from the NCM460 normal intestinal epithelial cell line. In addition, other options such as intestinal stem cells or organoids, which is the limitation of the present study, but more convincing methods in the study on CSCs, will be the next-step directions and methods to reveal the cross-relationship of CSCs and tumorigenesis.
An increasing number of studies have demonstrated that chronic inflammation plays an important role in tumorigenesis and progression (14,20), especially in colorectal cancer (16). Several inflammatory cytokines are found in serum, stools and bowel mucosa of patients with inflammatory bowel disease (31). Among these cytokines, TNF-α is a potent inflammatory factor, which can activate NF-κB signaling, upregulate the expression of other cytokines, chemokines, growth factors and transcription factors and accelerate tumorigenesis (31,32). Expression of TNF-α is notably increased in various cancer types and is often correlated with poor patient prognosis, thus TNF-α is regarded as a critical pro-tumorigenic cytokine (16,32). NF-κB activation induces innate and adaptive immune responses that can influence the progression of cancer and inflammation (16). In line with these observations, the present study reported that TNF-α treatment promoted cell proliferation, migration and invasion, induced the EMT phenotype, increased chemotherapy resistance and the ratio of CD133+ cells in NCM460s cells, which are all characteristics of malignant transformation. Certainly, it would be preferable to study the effect of anti-TNF antibodies on the indices, which is a potential limitation of the present study.
Furthermore, it was determined that TNF-α increased the phosphorylation of IKK in NCM460s cells at 0.5 h after stimulation, resulting in the phosphorylation and degradation of IκBα and promoting the phosphorylation and nuclear translocation of p65. As a crucial event of NF-κB signaling, the transcriptional activity of the NF-κB p65 responsive promoter was also significantly increased and maintained this increase up to 24 h after stimulation. Subsequently, the expression of proinflammatory cytokines IL-1β, IL-6, IL-8 and TNF-α were increased after stimulation, thus establishing a positive feedback loop that further enhanced activation of the NF-κB pathway and induced the expression of proinflammatory cytokines. Moreover, it was demonstrated that, in NCM460s cells, TNF-α also initiated the sequential activation of Wnt/β-catenin signaling, which serves a critical role in tumorigenesis and progression (33). The protein levels of APC, a negative modulator of the Wnt/β-catenin pathway, were downregulated 0.5 h after stimulation, while GSK3β phosphorylation, another negative modulator, was upregulated. Then, the dephosphorylation, accumulation and nuclear translocation of β-catenin, a central mediator in the canonical Wnt/β-catenin cascade, was observed in TNF-α-induced NCM460s cells. The luciferase reporter assay revealed that TNF-α stimulation significantly increased the promoter activity of TCF/LEF transcription factors in NCM460s cells. Thus, the data revealed that TNF-α induced the activation of NF-κB and Wnt/β-catenin pathways in NCM460s cells.
It has been demonstrated that activation of the Wnt/β-catenin and NF-κB pathways upregulates the expression of individual target genes through independent cascades during tumorigenesis, modulating cell proliferation, cell survival, apoptosis, metastasis and differentiation (14). In addition to these shared functions, NF-κB signaling is more crucial for inflammation and immune responses, whereas the Wnt/β-catenin pathway is mainly responsible for development and tissue regeneration (16). However, studies have suggested that these two pathways cross-regulate each other, extending their functions for each individual pathway. NF-κB signaling influences the activity of Wnt/β-catenin pathway, and the Wnt/β-catenin pathway also regulates inflammatory responses via interaction with NF-κB signaling (19,34).
Schwitalla et al (35), revealed that NF-κB signaling played a crucial role in the expression of Wnt/β-catenin and the intestinal epithelial cell-specific ablation of p65 suppressed the expansion of crypt stem cells. Furthermore, upregulated NF-κB signaling promoted the activation of the Wnt/β-catenin pathway and induced dedifferentiation of non-stem cells that acquired tumor-initiating capacity. Jang et al (34), revealed that Wnt/β-catenin signaling modulated the NF-κB pathway in TNF-α-induced inflammatory responses. In addition, NF-κB signaling can activate the expression of mesenchymal markers N-cadherin, vimentin, Slug and Snail, which downregulates the expression of adhesion protein E-cadherin, leading to EMT (16). Furthermore, nuclear β-catenin established a TCF/LEF/β-catenin complex via the interaction with TCF/LEF transcription factors, which also induces the EMT phenotype (33,36). Concurrently, the TCF/LEF/β-catenin complex has been revealed to promote the expression of downstream Wnt target genes c-Myc and cyclin D1 in TNF-α-induced NCM460s cells (19). Other studies have revealed that NF-κB activation upregulates the expression of various cell cycle proteins, especially the Wnt signaling target gene cyclin D1 (35,37,38). Crosstalk between Wnt/β-catenin and NF-κB signaling has been revealed to play a crucial role in inflammation-induced tumorigenesis (19).
Notably, the present study also revealed that there was a crosstalk between NF-κB and Wnt/β-catenin signaling in TNF-α-induced inflammatory responses. The nuclear protein levels of NF-κB p65 and the transcriptional activity of NF-κB p65 responsive promoter, which were markedly increased by TNF-α, were both blocked by p65-knockdown. Then, mRNA expression levels of proinflammatory cytokines IL-1β, IL-6, IL-8 and TNF-α, which were significantly upregulated by TNF-α, were also reduced to almost basal levels by p65-knockdown in TNF-α-treated NCM460s cells. GSK3β phosphorylation and nuclear protein levels of β-catenin were reduced by p65-knockdown in TNF-α-treated NCM460s cells. Subsequently, TCF/LEF promoter activity and expression of Wnt target genes c-Myc and cyclin D1 were also suppressed by p65 knockdown. Furthermore, PDTC, an inhibitor of NF-κB signaling, reversed the activation of the NF-κB pathway in a dose-dependent manner in TNF-α-treated NCM460s cells and counteracted TNF-α-induced activation of the Wnt/β-catenin pathway. The same effect on the NF-κB pathway was found following Wnt/β-catenin inhibitor IWP-2 application to TNF-α-treated NCM460s cells. Therefore, these results indicated that NF-κB and Wnt/β-catenin signaling cross-regulate each other in TNF-α-induced malignant transformation of ISCs.
The present study demonstrated that serum-free suspension culture is an effective strategy to enrich spheroid cells with stem cell characteristics in normal intestinal epithelial cell lines. The NF-κB and Wnt/β-catenin signaling pathways were activated to promote the malignant transformation of ISCs in TNF-α-induced inflammatory responses, in which these two pathways cross-regulated each other. These findings may aid our understanding of the underlying molecular mechanisms in intestinal tumorigenesis and progression, and provide new insight to develop more specific and effective treatments against inflammation-associated cancer types.
Supplementary Material
Acknowledgements
The authors greatly appreciate and thank the colleagues at the Key Laboratory of Fertility Preservation and Maintenance, Ministry of Education, of Ningxia Medical University.
Glossary
Abbreviations
- CSCs
cancer stem cells
- ISCs
intestinal stem cells
- SFM
serum-free medium
- EMT
epithelial-mesenchymal transition
Funding
The present study was supported by the National Natural Science Foundation of China (grant no. 31660336) and West China first-class Disciplines Basic Medical Sciences at Ningxia Medical University (grant no. NXYLXK2017B07).
Availability of data and materials
All data used during this study are available from the corresponding authors upon reasonable request. Supplementary files related to this article can be found in the online version.
Authors' contributions
XZ and LD were responsible for the acquisition and analysis of all the experimental data, as well as the writing of the paper. LM, XL and FX participated in the study design. DZ and HZ were involved in the data interpretation and the final revision of the manuscript. All authors read and approved the manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Chen W, Sun K, Zheng R, Zeng H, Zhang S, Xia C, Yang Z, Li H, Zou X, He J. Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018;30:1–12. doi: 10.21147/j.issn.1000-9604.2018.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olejniczak A, Szarynska M, Kmiec Z. In vitro characterization of spheres derived from colorectal cancer cell lines. Int J Oncol. 2018;52:599–612. doi: 10.3892/ijo.2017.4206. [DOI] [PubMed] [Google Scholar]
- 4.Zhao H, Yan C, Hu Y, Mu L, Huang K, Li Q, Li X, Tao D, Qin J. Sphere-forming assay vs. organoid culture: Determining long-term stemness and the chemoresistant capacity of primary colorectal cancer cells. Int J Oncol. 2019;54:893–904. doi: 10.3892/ijo.2019.4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah S, Pocard M, Mirshahi M. Targeting the differentiation of gastric cancer cells (KATOIII) downregulates epithelial-mesenchymal and cancer stem cell markers. Oncol Rep. 2019;42:670–678. doi: 10.3892/or.2019.7198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu R, Gires O, Zhu L, Liu J, Li J, Yang H, Ju G, Huang J, Ge W, Chen Y, et al. TSPAN8 promotes cancer cell stemness via activation of sonic Hedgehog signaling. Nat Commun. 2019;10:2863. doi: 10.1038/s41467-019-10739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Celia-Terrassa T, Liu DD, Choudhury A, Hang X, Wei Y, Zamalloa J, Alfaro-Aco R, Chakrabarti R, Jiang YZ, Koh BI, et al. Normal and cancerous mammary stem cells evade interferon-induced constraint through the miR-199a-LCOR axis. Nat Cell Biol. 2017;19:711–723. doi: 10.1038/ncb3533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cable J, Fuchs E, Weissman I, Jasper H, Glass D, Rando TA, Blau H, Debnath S, Oliva A, Park S, et al. Adult stem cells and regenerative medicine-a symposium report. Ann N Y Acad Sci. 2019;1462:27–36. doi: 10.1111/nyas.14243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ji R, Zhang X, Qian H, Gu H, Sun Z, Mao F, Yan Y, Chen J, Liang Z, Xu W. miR-374 mediates the malignant transformation of gastric cancer-associated mesenchymal stem cells in an experimental rat model. Oncol Rep. 2017;38:1473–1481. doi: 10.3892/or.2017.5831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pastrana E, Silva-Vargas V, Doetsch F. Eyes wide open: A critical review of sphere-formation as an assay for stem cells. Cell Stem Cell. 2011;8:486–498. doi: 10.1016/j.stem.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li SC, Lee KL, Luo J, Zhong JF, Loudon WG. Convergence of normal stem cell and cancer stem cell developmental stage: Implication for differential therapies. World J Stem Cells. 2011;3:83–88. doi: 10.4252/wjsc.v3.i9.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drost J, van Jaarsveld RH, Ponsioen B, Zimberlin C, van Boxtel R, Buijs A, Sachs N, Overmeer RM, Offerhaus GJ, Begthel H, et al. Sequential cancer mutations in cultured human intestinal stem cells. Nature. 2015;521:43–47. doi: 10.1038/nature14415. [DOI] [PubMed] [Google Scholar]
- 13.Barker N, Ridgway RA, van Es JH, van de Wetering M, Begthel H, van den Born M, Danenberg E, Clarke AR, Sansom OJ, Clevers H. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457:608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 14.Shigdar S, Li Y, Bhattacharya S, O'Connor M, Pu C, Lin J, Wang T, Xiang D, Kong L, Wei MQ, et al. Inflammation and cancer stem cells. Cancer Lett. 2014;345:271–278. doi: 10.1016/j.canlet.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Tang F, Wang Y, Hemmings BA, Rüegg C, Xue G. PKB/Akt-dependent regulation of inflammation in cancer. Semin Cancer Biol. 2018;48:62–69. doi: 10.1016/j.semcancer.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Taniguchi K, Karin M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat Rev Immunol. 2018;18:309–324. doi: 10.1038/nri.2017.142. [DOI] [PubMed] [Google Scholar]
- 17.Zanotto-Filho A, Rajamanickam S, Loranc E, Masamsetti VP, Gorthi A, Romero JC, Tonapi S, Goncalves RM, Reddick RL, Benavides R, et al. Sorafenib improves alkylating therapy by blocking induced inflammation, invasion and angiogenesis in breast cancer cells. Cancer Lett. 2018;425:101–115. doi: 10.1016/j.canlet.2018.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bloemendaal AL, Buchs NC, George BD, Guy RJ. Intestinal stem cells and intestinal homeostasis in health and in inflammation: A review. Surgery. 2016;159:1237–1248. doi: 10.1016/j.surg.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Ma B, Hottiger MO. Crosstalk between Wnt/β-catenin and NF-κB signaling pathway during inflammation. Front Immunol. 2016;7:378. doi: 10.3389/fimmu.2016.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kakiuchi N, Yoshida K, Uchino M, Kihara T, Akaki K, Inoue Y, Kawada K, Nagayama S, Yokoyama A, Yamamoto S, et al. Frequent mutations that converge on the NFKBIZ pathway in ulcerative colitis. Nature. 2020;577:1–6. doi: 10.1038/s41586-019-1856-1. [DOI] [PubMed] [Google Scholar]
- 21.Kong FF, Li D, Yang H, Ma J, Pan X, Liu HX, Huo JN, Ma XX. Preliminary identification of endometrial cancer stem cells in vitro and in vivo. Biochem Biophys Res Commun. 2017;490:506–513. doi: 10.1016/j.bbrc.2017.06.070. [DOI] [PubMed] [Google Scholar]
- 22.Zhai Y, Wei R, Sha S, Lin C, Wang H, Jiang X, Liu G. Effect of NELL1 on lung cancer stemlike cell differentiation. Oncol Rep. 2019;41:1817–1826. doi: 10.3892/or.2019.6954. [DOI] [PubMed] [Google Scholar]
- 23.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Yun CW, Han YS, Kim S, Jeong D, Kwon HY, Kim H, Baek MJ, Lee SH. Melatonin and 5-fluorouracil co-suppress colon cancer stem cells by regulating cellular prion protein-Oct4 axis. J Pineal Res. 2018;65:e12519. doi: 10.1111/jpi.12519. [DOI] [PubMed] [Google Scholar]
- 25.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 27.Leung C, Tan SH, Barker N. Recent advances in Lgr5(+) stem cell research. Trends Cell Biol. 2018;28:380–391. doi: 10.1016/j.tcb.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 28.Arab-Bafrani Z, Shahbazi-Gahrouei D, Abbasian M, Saberi A, Fesharaki M, Hejazi SH, Manshaee S. Culturing in serum-free culture medium on collagen type-I-coated plate increases expression of CD133 and retains original phenotype of HT-29 cancer stem cell. Adv Biomed Res. 2016;5:59. doi: 10.4103/2277-9175.179181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leng Z, Tao K, Xia Q, Tan J, Yue Z, Chen J, Xi H, Li J, Zheng H. Kruppel-like factor 4 acts as an oncogene in colon cancer stem cell-enriched spheroid cells. PLoS One. 2013;8:e56082. doi: 10.1371/journal.pone.0056082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu F, Li C, Zheng X, Zhang H, Shen Y, Zhou L, Yang X, Han B, Zhang X. Lung adenocarcinoma resistance to therapy with EGFR-tyrosine kinase inhibitors is related to increased expression of cancer stem cell markers SOX2, OCT4 and NANOG. Oncol Rep. 2020;43:727–735. doi: 10.3892/or.2019.7454. [DOI] [PubMed] [Google Scholar]
- 31.Chen X, Liu R, Liu X, Xu C, Wang X. Protective role of Coxsackie-adenovirus receptor in the pathogenesis of inflammatory bowel diseases. Biomed Res Int. 2018;2018:7207268. doi: 10.1155/2018/7207268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Balkwill F. Tumour necrosis factor and cancer. Nat Rev Cancer. 2009;9:361–371. doi: 10.1038/nrc2628. [DOI] [PubMed] [Google Scholar]
- 33.Kretzschmar K, Clevers H. Wnt/β-catenin signaling in adult mammalian epithelial stem cells. Dev Biol. 2017;428:273–282. doi: 10.1016/j.ydbio.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 34.Jang J, Jung Y, Chae S, Chung SI, Kim SM, Yoon Y. WNT/β-catenin pathway modulates the TNF-α-induced inflammatory response in bronchial epithelial cells. Biochem Biophys Res Commun. 2017;484:442–449. doi: 10.1016/j.bbrc.2017.01.156. [DOI] [PubMed] [Google Scholar]
- 35.Schwitalla S, Fingerle AA, Cammareri P, Nebelsiek T, Goktuna SI, Ziegler PK, Canli O, Heijmans J, Huels DJ, Moreaux G, et al. Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell. 2013;152:25–38. doi: 10.1016/j.cell.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 36.Teo JL, Kahn M. The Wnt signaling pathway in cellular proliferation and differentiation: A tale of two coactivators. Adv Drug Deliv Rev. 2010;62:1149–1155. doi: 10.1016/j.addr.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Ledoux AC, Perkins ND. NF-κB and the cell cycle. Biochem Soc Trans. 2014;42:76–81. doi: 10.1042/BST20130156. [DOI] [PubMed] [Google Scholar]
- 38.Liu X, Chen H, Hou Y, Ma X, Ye M, Huang R, Hu B, Cao H, Xu L, Liu M, et al. Adaptive EGF expression sensitizes pancreatic cancer cells to ionizing radiation through activation of the cyclin D1/P53/PARP pathway. Int J Oncol. 2019;54:1466–1480. doi: 10.3892/ijo.2019.4719. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used during this study are available from the corresponding authors upon reasonable request. Supplementary files related to this article can be found in the online version.