Abstract
A number of important principles in effective risk communication established in the late 20th century can provide important scientific insight into patient response to the risks posed by coronavirus disease 2019 (COVID-19). Early risk communication scholars found acceptability of risk was shaped by 2 key components: hazard and outrage. The number of people who are exposed, infected, and fall ill can be considered the hazard. How the public and patients and respond to messages regarding risk mitigation relates to outrage. Social and cultural factors, immediacy, uncertainty, familiarity, personal control, scientific uncertainty, and trust in institutions and media all shape perception and response to risk mesaging. Outrage factors influence the ever-changing public understanding of COVID-19 risk. In concert, hazard and outrage along with cultural and economic context shape adherence to, and overall acceptance of, personal mitigation strategies including wearing facemasks and social distancing among the general public. The spread of misinformation on social media also provides both challenges and opportunities for clinicians. Social media offers an opportunity for experts to quickly convey true information about hazards, but offers others the opportunity to counter this with the spread of misinformation and exacerbate outrage. We propose strategies for infectious diseases clinicians to apply risk communication principles and frameworks to improve patient care and public message development in response to COVID-19.
Keywords: COVID-19, risk communication, social media
Public perception of risk in a pandemic is shaped by not only the true nature of the hazard but include various contextual outrage factors. Public perception of outrage affects adherence to mitigation strategies. Social media offers important opportunities for experts to respond quickly but can also present challenges for effective risk communication during a pandemic such as coronavirus disease 2019 (COVID-19).
As healthcare providers struggle to develop effective messaging to support patients’ understanding, how the public perceives and responds to risk messages is critically important. A number of important principles in effective risk communication established in response to environmental disasters and pollution events in the late 20th century can provide important scientific insight into patient response to the risks posed by coronavirus disease 2019 (COVID-19) [1–4]. These insights have shaped risk communication and principles of risk communication for decades. Risk communication, focused on communication of hazards to potentially exposed communities, evolved in large part in the context of public health and environmental disaster response [5, 6]. In more recent years, the scope of risk communication has expanded to include communication strategies to better address ongoing public health challenges, including global pandemics, and is referred to more specifically as crisis communication [6–9]. Here we discuss strategies for infectious diseases clinicians to apply these existing, early risk communication principles and frameworks to effectively support patients and the general public response to COVID-19.
Key to understanding and responding to the ongoing COVID-19 pandemic is that perceptions of risk are driven by 2 primary factors: hazard and outrage [2, 4]. In other words, what a particular audience perceives as acceptable or unacceptable risk includes both the nature of the hazard and degree of outrage. Among the many early leaders in risk communication, Peter Sandman, Vincent Covello, and Paul Slovic were among the first to offer psychometric insights to explain the importance of risk perception as being a combination of technical perceptions of hazard and outrage [1–3, 10]. Their investigations included careful psychometric studies of risk perception and factors that shaped the interactions between scientists and the general public. What they found was the actual threats to health were only one aspect of risk perception. Risk perception was also shaped by factors that altered acceptability of risk in the minds of different audiences, messages, and in different context. For example, despite clear evidence that wearing masks can reduce transmission of COVID-19, the acceptability of and adherence to wearing masks varies greatly. In the United States, mask wearing has become more of a political issue than a fact-based intervention, and thus the use of masks varies widely among populations. In other communities and countries, mask wearing is seen as a reasonable strategy, and masks are commonly used by the public [11]. The variation in acceptability and willingness for individuals to respond to expert opinions creates significant challenges for health education among patients [11]. Clinicians are scientists trained to respond to facts; however, research has shown the public and patients’ perceptions, concerns, and responses do not always conform only to science and reason [4]. Subsequently, the hazard and outrage framework was established as a way to demonstrate how risks are often perceived differently among technical experts including healthcare providers, epidemiologists and front-line workers, and the general public [3, 10]. From this the science of risk communication was established [6].
Technical experts define risk based on quantitative hazard information regarding the burden, etiology, and spread. Most often, even when factual information about a hazard is provided, the public perception of risk from an unknown and emerging hazard such as COVID-19 leads to a more emotional response or outrage. Outrage, in turn, shapes acceptability and adherence to risk mitigation strategies such as social distancing and wearing of face masks [1, 3, 10]. Therefore, outrage factors shaping public risk perceptions are important for clinicians to understand, because they will determine how and why the general public will react and respond to messages [4]. In other words, scientists are often perplexed by public perceptions and acceptance of misinformation; however, what a particular audience perceives as acceptable or unacceptable risk includes both the nature of the hazard and degree of outrage.
It is well established that carefully planned crisis communication can play a critically important role in prevention and mitigation of pandemics over time by reducing anxiety and fear, supporting public adherence to mitigation strategies, reducing burden, and increasing the effectiveness of medical interventions [6]. Most infectious diseases clinicians, epidemiologists, and scientists do not receive formal training in risk communication despite their critically important role as experts well versed in understanding the scientific and technical aspects of risk. A number of case studies have shown that when communication is led by credible scientists, the public’s response to the risk and (and as a result, the containment of the outbreak) is often more successful than if communication is led solely by individuals who are not subject matter experts [6]. As such, it is important for infectious diseases clinicians to be well prepared to lead risk communication during crises, in this case, the COVID-19 pandemic.
Alhough news outlets have always played an important role in informing and shaping public perception of risk, social media has rapidly become a major driver of what the public understands and responds to. Experts can use social media in crisis response by rapidly spreading hazard information and helping inform the public and patients on actions they can take to mitigate risk [7]. At the very same time, social media can rapidly spread misinformation across large portions of the public. Public outrage driven by social media must be considered by experts to understand and deploy effective communication strategies aimed at mitigating and control of risks overtime [7–9]. Although these larger social forces are difficult to control, the hazard plus outrage framework can help clinicians and public health experts remain trusted sources in the fight against COVID-19.
Hazard and Outrage Factors Impacting Public Perceptions of Risks and Mitigation Strategies
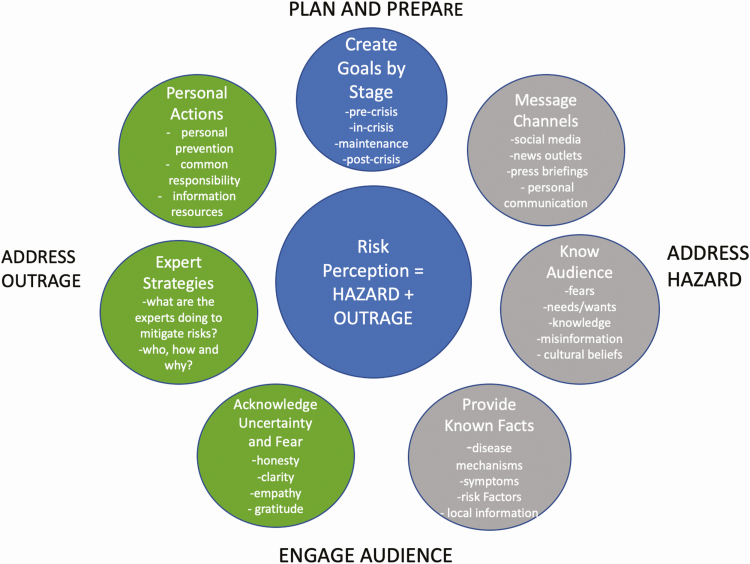
The unfolding scale and intensity of the COVID-19 pandemic makes clear that engagement with and by the public is essential for effective risk reduction, mitigation, and ultimate control [8, 12]. Figure 1 outlines a framework and set of guidelines that builds on past crisis and risk communication strategies that can support clinicians in their response to COVID-19 adapted from early hazard + outrage frameworks that also takes into account new understanding of the cultural and social media context shaping the pace and mode by which information is shared [2–7]. Hazard information conveyed by experts includes facts and information on the transmission, mechanisms, and severity of disease. This is all set within the context of feelings and emotions that are shaping public outrage. The public perception of risk from COVID-19, as an unknown and emerging hazard, is considerably shaped by outrage. Key factors shaping outrage toward COVID-19 include catastrophic potential, familiarity, understanding, scientific uncertainty, personal control, voluntariness, trust in institutions, and media attention (Table 1). Outrage is an emotional response shaped not only by factors surrounding the nature and characteristics of hazards, but the degree to which individuals and communities deem risks as unsafe, unacceptable, or something to be feared—which in turn influences how individuals and communities respond to and adhere to important public health messages regarding risk mitigation [1]. It also shapes the public’s acceptability of and the adherence to COVID-19 risk mitigation strategies such as social distancing and use of face masks [1, 3, 10].
Figure 1.
Crisis communication: addressing hazard + outrage during the COVID 19 pandemic. Abbreviation: COVID-19, coronavirus disease 2019.
Table 1.
Outrage Factors Influencing Public Perceptions of Risk and Acceptability of Risk Mitigation Strategies Over Timea
| Factors Influencing Public Perceptions of Risksb | Directionality of Increased Risk Perception (Increased Outrage, Lower Acceptability of Risk) | Changing Public Risk Perception Over Time in the US Regarding COVID-19 Pandemic (December 2019- April 2020) | ||
|---|---|---|---|---|
| Prevention | Precrisis | Crisis | ||
| High catastrophic potential | Fatalities and injuries grouped in time and space rather than random and scattered | Low | Low/med | High |
| Familiarity | Unfamiliar | High | Med | Low |
| Understanding | Difficult to understand | High | High | High |
| Scientific uncertainty | High scientific uncertainty | High | High | High |
| Controllable | Lack of personal control and agency | High | High | High/low |
| Voluntariness | Involuntary vs voluntary | Low | High | Low |
| Trust in institutionsb | Lack of trust | Low | High/Low | High/low |
| Media attention | High vs low media attention | Low | High | High |
Abbreviation: COVID-19, coronavirus disease 2019.
aAdapted from below from Appendix C— in Covello et al [3].
bNote that the perception of risk can vary by context and cultural beliefs of the public audience.
When there were only a few cases of COVID-19 scattered across the United States, public perception of COVID-19 risk was low. Despite early warnings by experts regarding the catastrophic potential of COVID-19, over 25% of Americans felt that they had a <1% chance of becoming infected [13]. This perception was reinforced by some government leaders. Consequently, early attempts by public health authorities and experts to mitigate risk by encouraging social distancing and wearing masks were seen as invasive, alarmist, too much government interference, and an unnecessary burden on economic growth. At the same time, early research from California also found that, although individuals disagreed on the true nature of the hazard or risk of exposure and adverse outcomes related to COVID-19, the acceptability and adherence to social distancing increased as more information on the nature of the hazard emerged [14].
The lack of familiarity around COVID-19 has also shaped public perception and response, with some in the public becoming extremely anxious, although others downplayed risks by equating it to something more familiar such as influenza [10]. Others who are fortunate to have few personal experiences with the illness or deaths are also willing to downplay societal risks. Adding to the challenge is the difficulty in understanding the complex and constantly changing scientific uncertainty surrounding COVID-19. Early in the outbreak, the public was willing to accept uncertainty; as we move forward, the pandemic presents challenges that make specific, actionable timelines and strategies for risk mitigation difficult. This uncertainty can again increase anxiety, stress, and fear, causing the public to dismiss risk altogether, or become angry about mitigation strategies. Communicating actionable steps for the public to take can help to reduce this anxiety and fear by increasing a sense of agency and personal control [2, 3].
The shifting voluntariness of COVID-19 exposure and risk of severe illness across the population also has played an important role in shaping risk perceptions. Initially, the involuntary nature of social distancing, forced isolation, and loss of personal freedom imposed by social distancing exacerbated anxiety and stress, and increased public outrage among many. This was particularly the case for individuals who perceived themselves at low risk of becoming infected and/or developing severe COVID-19, as the benefits of social distancing did not outweigh the costs of compliance with social distancing. However, as the pandemic rapidly spread, the involuntary nature of COVID-19 viral exposure shifted public perception to more acceptance of social distancing as a new and necessary normal. Furthermore, face masks also were perceived as unnecessary and alarmist by some early on. Experts recommended against the use of face masks by the public as an unnecessary and ineffective intervention before fully understanding the true nature of hazards, more specifically, the mechanisms by which the virus was spread and the high infection rates. With the change to authorities recommending the wearing of face masks, some individuals are relieved because wearing a face mask may provide perceived personal control over the involuntary risk of exposure, although others are perplexed, stressed, or angered by this scientific uncertainty.
In the case of COVID-19 the conflicting information and changing messages from experts that alter public perceptions is especially challenging [9, 15]. For example, many state officials, clinicians, and epidemiologists are currently investigating factors that influence immunity, and recommendations for when and how to relax social distancing measures. Given significant scientific uncertainty around COVID-19 immunity and asymptomatic infection rates and transmission, experts are examining local trends and data to develop plans for the current (and potential future) waves of infections. At the same time, the public is aware on social media that some states are relaxing social distancing steps to a wide-ranging degree, although others continue to maintain stringent measures. Furthermore, a large portion of the public is now facing “quarantine fatigue” in which many have been social distancing with little to no familiarity of risk, while suffering real economic consequences, all of which increase outrage or a more emotional response. At the same time, some communities and workers, such as meat packers, face insurmountable risks. A lack of understanding and voluntariness around the public’s participation in social distancing measures can contribute to decreased trust in institutions and shape the public’s willingness or lack thereof to maintain social distancing.
Public trust in institutions that are perceived to be providing reliable information is important in crisis and risk communication [6, 10]. Early messaging by public officials that the COVID-19 pandemic was “under control” reduced the authority and messaging being delivered by technical experts regarding the true nature of risk. Similarly, the changing messaging from public officials around social distancing and use of face masks is likely to reduce trust in governmental institutions. Relative differences in media attention around the risk posed by COVID-19 differentially influenced the public’s perception of the risk and mitigation strategies necessary to appropriately contain COVID-19 [7].
Responding to COVID-19 in the Era of Social Media
The media has always played a critically important role in informing the public during crises and emergencies disasters; social media now also plays a large and growing role in shaping outrage and thus the public’s perceptions of risks and mitigation [5–9]. Social media offers opportunities for both experts and the general public to quickly spread information to a large number of individuals [7, 12, 16]. Social media is therefore both an asset and barrier to developing effective risk communication strategies and response.
Clinicians can play a critically important role as trusted sources on social media to support the spread of new information as it becomes available and address individuals patient concerns as they evolve, knowing that public perceptions of risk will vary greatly across individuals. The general public tends to choose select media channels for news, often in the context of political preference based on sources of news they trust [12, 15]. Social media can create an “echo chamber” of media attention, with individuals sharing messages and news with like-minded followers. Some consumers of social media will work to sort through the different information; however, this process increases the chances of encountering conflicting news and messages, and additional potential of finding material aiming to discredit reliable experts and news sources. Contradicting information can again increase a lack of understanding and reduce individuals’ perceptions of their agency and control regarding risk and mitigation.
Although our current social media era poses challenges in supporting the public’s perceptions of risk, it can also offer experts many advantages [16]. If clinicians and public health experts can get ahead of the public in shaping messages, social media offers an almost immediate opportunity to spread information, become a trusted source, and to build relationships with the public. Experts can also use social media to quickly contradict misinformation with accurate information, for example, by offering links to trusted healthcare providers and/or public health sources providing the same or similar messaging.
Responding to the COVID-19 Crisis as Information and Knowledge Evolves Over Time
The dynamic nature of pandemics means that experts and public officials need to address different aspects of both hazard and outrage as information evolves [11, 16]. The actions required by the public to respond to pandemics also vary over time. The World Health Organization and Centers for Disease Control and Prevention have developed guidance to address the hazards and outrage shaping public perceptions of risk as crises unfold from precrisis to mid-crisis to post-crisis [8, 16]. In the case of COVID-19, there will likely be multiple phases of outbreaks and messaging that will need to be continually modified to meet these ongoing-communication challenges and shape new goals for engaging the public, reducing fear, and supporting ongoing preparedness and response. Even in this challenging context, the cardinal principles of risk communication stay the same whether using a social media platform or communicating in a clinician’s office. To develop clear, simple, and appropriate messages for effective communication, it is important to plan and respond to public audience needs and to directly address sources of fear, anxiety, and misinformation. Monitoring various communication channels (social media, news outlets, personal communication, press briefings) and consistency across them will also be important. Knowing what information is being conveyed can help practitioners in how to be proactive in communicating mitigation strategies and offering empathy. Table 2 outlines key principles that may be useful in planning such communication at the individual, health system, or population level including knowing your audience, engaging audience as partners, developing a plan, speaking with compassion, being transparent and honest, and evaluating frequently.
Table 2.
Communicating Risks During COVID-19
| Risk Communication Strategy | COVID-19 Patient Communication | Address Hazard | Address Outrage |
|---|---|---|---|
| Plan carefully | Careful planning can help. For example, establish communication goals. EXAMPLE Communication goals: Face covering in public spaces can reduce risks. Context: Individuals who support use: fearful of infection, altruistic. Individuals who are resistant—afraid, find them annoying and feel that their rights are taken away. | Provide data driven transparent decision making. For example, face masks used by the public have been shown to reduce infection rates in some areas by as much as 50% [11]. The most common way for infection to spread is through droplets released during sneezing, coughing, or even talking. | Individuals who support their use: Thank patients for doing their part, protecting their health and others. Individuals who are resistant: Facemasks can be a challenge, many times wearing a facemask is your choice—but they do work. It can protect you, your family, and friends. |
| Accept the public as partners. | Ask patients concerns, ask about fears, respond. EXAMPLE: Patient states they want to exercise outside, but are afraid of exposures. | Respond with facts: Exposures and risk of infection seem to be worse indoors than outdoors. If the weather is nice, you can safely go outside for a walk. If your street is crowded wear a mask. | Be empathetic: Exercising outside can feel scary, but it can be really helpful. Try to find times when you feel there are less people and you can keep your distance, and you can always wear a mask. |
| Be transparent and honest. Acknowledge the uncertainty. | Trust is built on recognizing what is and is not known. Information evolves over time, pretending to know everything discredits authority over time. | If you as the expert do not know an answer, be candid. | Offer credible information and sources by which individuals can do their own research if warranted. |
| Speak with compassion. | As clinicians and public health practitioners, it is important to be empathetic with patients. | Acknowledge that the uncertainty of COVID-19 is challenging for everyone. | Vulnerability opens the door to support patients with credible resources, information, and opportunities to seek additional help. |
| Evaluate and reassess strategies | There is a need to continually assess new information, and evaluate the accuracy and effectiveness of information across time. | Stay informed about how messages are being perceived and refine them to reach the right audience and consider cadence to avoid information overload while providing substantive updates. | Know your audience and develop new messages that address their changing concerns in a language that is relatable. |
Abbreviation: COVID-19, coronavirus disease 2019.
Months into the COVID-19 pandemic in the United States, public outrage remains high with significant uncertainty around public perception of risk, the need for mitigation strategies, and the individual actions to take for appropriate mitigation. There are no rights or wrongs, but we do have much that can be learned from the past. Understanding the fundamentals of risk perception is critical for clinicians and public health experts to be a collective and effective voice to mitigate risk and save lives.
Notes
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial support. N. S. is supported by the National Institute Of Allergy And Infectious Diseases of the National Institutes of Health under award number DP2AI144244.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Slovic P Perception of risk. Science 1987; 236:280–5. [DOI] [PubMed] [Google Scholar]
- 2. Sandman PM Risk communication: facing public outrage. EPA Journal. 1987;November 1987; 2:21–22. [Google Scholar]
- 3. Covello VT, Sandman PM, Slovic P.. Risk communication, risk statistics, and risk comparison: a manual for plant managers. Washington, DC:Chemical Manufacturers Association, 1988. [Google Scholar]
- 4. Sandman PM Hazard versus outrage in the public perception of risk. In: Covello VT, McCallum D, MT P, eds. Effective risk communication: contemporary issues in risk analysis. Vol 4 Boston, MA: Springer, 1989. [Google Scholar]
- 5. Eisenman DP, Cordasco KM, Asch S, Golden JF, Glik D. Disaster planning and risk communication with vulnerable communities: lessons from Hurricane Katrina. Am J Public Health 2007; 97Suppl 1:S109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Glik DC Risk communication for public health emergencies. Annu Rev Public Health 2007; 28:33–54. [DOI] [PubMed] [Google Scholar]
- 7. Ophir Y Coverage of epidemics in American newspapers through the lens of the crisis and emergency risk communication framework. Health Secur 2018; 16:147–57. [DOI] [PubMed] [Google Scholar]
- 8. Quinn P Crisis communication in public health emergencies: the limits of ‘legal control’ and the risks for harmful outcomes in a digital age. Life Sci Soc Policy 2018; 14:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rossmann C, Meyer L, Schulz PJ. The mediated amplification of a crisis: communicating the A/H1N1 pandemic in press releases and press coverage in Europe. Risk Anal 2018; 38:357–75. [DOI] [PubMed] [Google Scholar]
- 10. Fischhoff B The realities of risk-cost-benefit analysis. Science 2015; 350:aaa6516. [DOI] [PubMed] [Google Scholar]
- 11. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med 2020; 8:434–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sandman PM Crisis communication best practices: some quibbles and additions. J Appl Commun Res. 2006; 34:257–262. [Google Scholar]
- 13. Miller J, Key J. Slightly more than 1 out of 4 Americans believe they have almost no chance of being infected with coronavirus in next 3 months. Coronavirus (COVID-19). University of Southern California, USC Leonard D. Schaeffer Center for Health Policy and Economics, 2020. [Google Scholar]
- 14. Bruine de Bruin W, Bennet D. USC study finds increasing actions and risk perceptions for coronavirus. Coronavirus (COVID-19). University of Southern California, USC Leonard D. Schaeffer Center for Health Policy and Economics, 2020. [Google Scholar]
- 15. Hills TT The dark side of information proliferation. Perspect Psychol Sci 2019; 14:323–30. [DOI] [PubMed] [Google Scholar]
- 16. Lwin MO, Lu J, Sheldenkar A, Schulz PJ. Strategic uses of Facebook in Zika outbreak communication: implications for the crisis and emergency risk communication model. Int J Environ Res Public Health. 2018; 15:1974. doi: 10.3390/ijerph15091974 [DOI] [PMC free article] [PubMed] [Google Scholar]