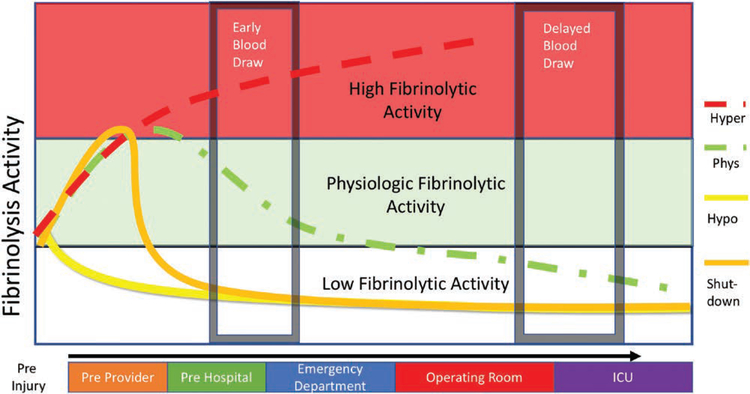
Figure 3.
Timing of blood draw and fibrinolysis phenotypes. The theoretical time course of fibrinolysis changes of the various phenotypes of fibrinolysis after severe injury. With severe injury and shock, the expected response is activation of the fibrinolytic system to counterbalance early hypercoagulability. This occurs early after injury and often before prehospital providers arrive on the scene. After initial prehospital resuscitation, the phenotypes of postinjury fibrinolysis emerge. Patients who develop acute fibrinolysis shutdown will have a rapid transition to a low fibrinolytic state, while patients with physiologic fibrinolysis will have a more gradual decline in fibrinolytic activity. The hypofibrinolytic phenotype will have a blunted response to trauma and retain low fibrinolysis activity early after injury. Early blood draws (within hour of injury) can stratify patients into respective phenotypes except for hypofibrinolysis and fibrinolysis shutdown. After resuscitation, all phenotypes converge into a low fibrinolytic state due to a postresuscitation acquired fibrinolysis resistance from plasminogen activator inhibitor 1 (PAI-1) elevation. Patients who have sustained hyperfibrinolytic after initial in-hospital resuscitation efforts are unlikely to be alive several hours after injury. Obtaining blood samples several hours after provides a feedback on successful resuscitation efforts, but differentiating a patient’s initial fibrinolytic phenotype based on viscoelastic hemostatic assays (VHA) is not possible as all prior phenotypes have converged to a fibrinolytic resistant state. This postresuscitation fibrinolytic resistant state is not associated with increased mortality, but the duration that these patients remain in fibrinolysis shutdown predicts adverse outcomes. ICU indicates intensive care unit.