Figure 2: Selected case examples of checkpoint inhibitor associated pneumonitis.
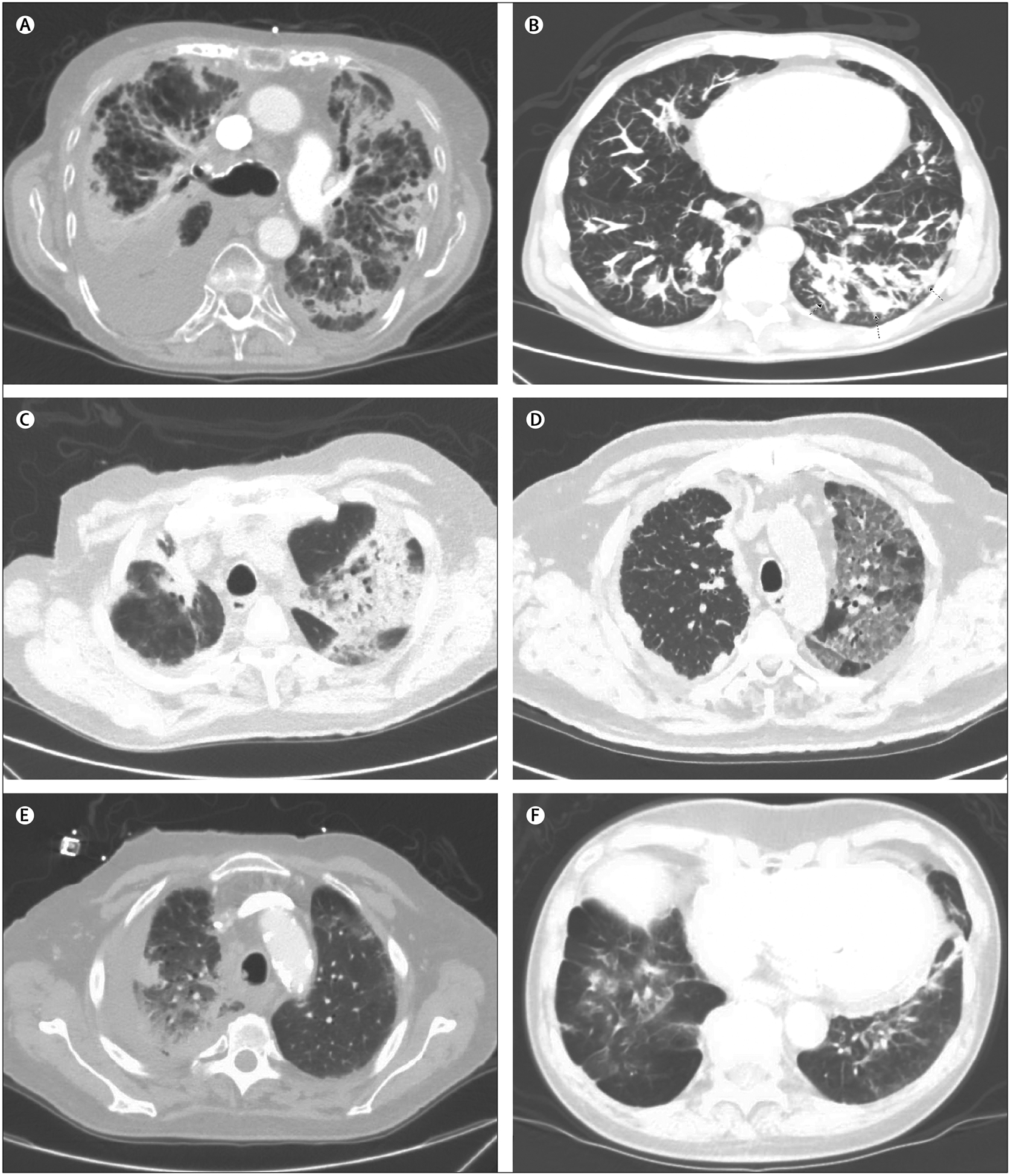
toxicity Case listings include: demographics, cancer type, immunotherapy type, pneumonitis onset, and radiographic appearance. (A) 87-year-old man, non-small-cell lung cancer (NSCLC), anti-programmed cell death ligand 1 (PDL1), 9 weeks, reticulonodular opacities, and septal thickening. (B) 60-year-old man, renal cell carcinoma, antiprogrammed cell death protein 1 (PD1), 5 months, nodular opacities. (C) 77-year-old man, melanoma, combination anti-PD1 and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitor, 6 weeks, patchy ground glass and nodular consolidation, cryptogenic organising pneumonia. (D) 71-year-old man, NSCLC, anti-PD1, 2 weeks, mosaic attenuation of ground glass opacities. (E) 70-year-old man, NSCLC, anti-PD1, 1 month, consolidation. (F) 78-year-old man, NSCLC, anti-PDL1, 4 months, consolidations and ground glass densities in the bases.
