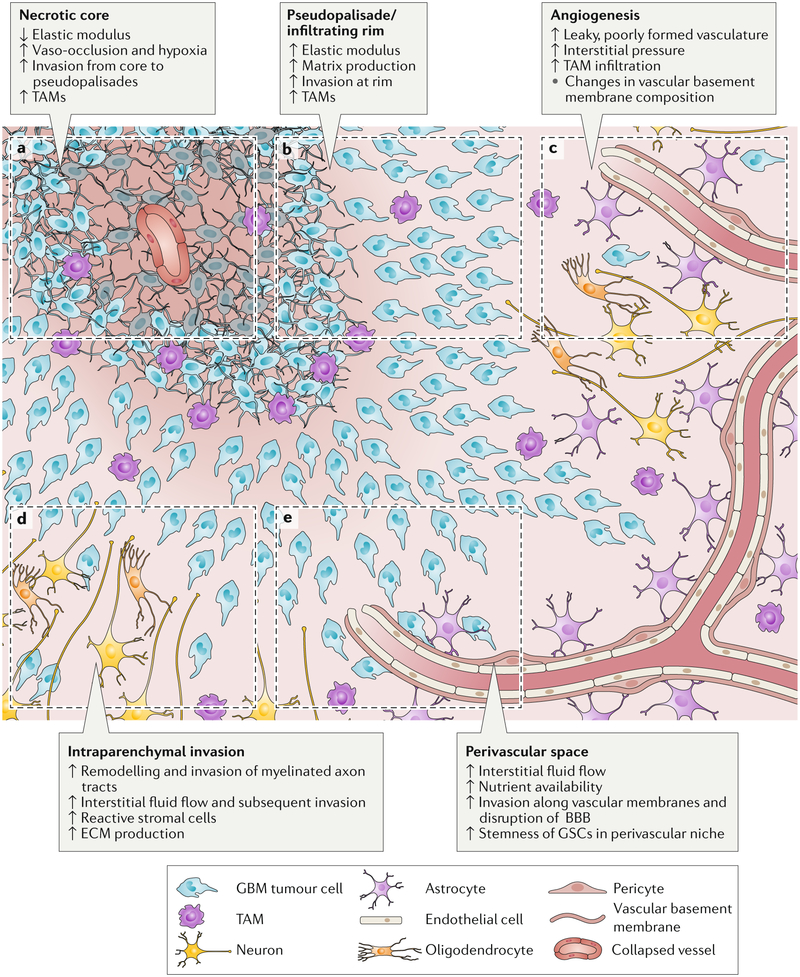
Figure 1. Schematic of gliobastoma (GBM) regions.
This GBM schematic illustrates changes during tumour progression in the different microenvironmental regions. a) The necrotic core is softer than surrounding tissue and is thought to form after increases in cell density beyond a certain threshold or vaso-occlusive events result in hypoxia. b) Psuedopalisades are regions of high cell density thought to form as cells migrate away from hypoxic regions. These zones have an increased elastic modulus and matrix production compared to healthy tissue and necrotic regions. GBM cells invade from the outer edge of the cell-dense tumour into healthy tissue at the infiltrating rim. c) GBM tumours show hypervascularity with increased angiogenesis compared to healthy brain tissue. Tumour-associated vasculature is poorly formed, leaky and leads to an increase in interstitial fluid pressure. d) Tumour cells invading through the parenchyma often follow and remodel the surface of myelinated tracts – a region in which high interstitial fluid flow may also drive invasion. e) Tumour cells rapidly invade the vasculature, where they are exposed to nutrients, high interstitial fluid flow and haptotactic cues in basement membranes. The perivascular niche also supports stemness and survival of glioblastoma stem cells (GSCs). TAM, tumour-associated macrophage; ECM, extracellular matrix; BBB, blood-brain barrier.