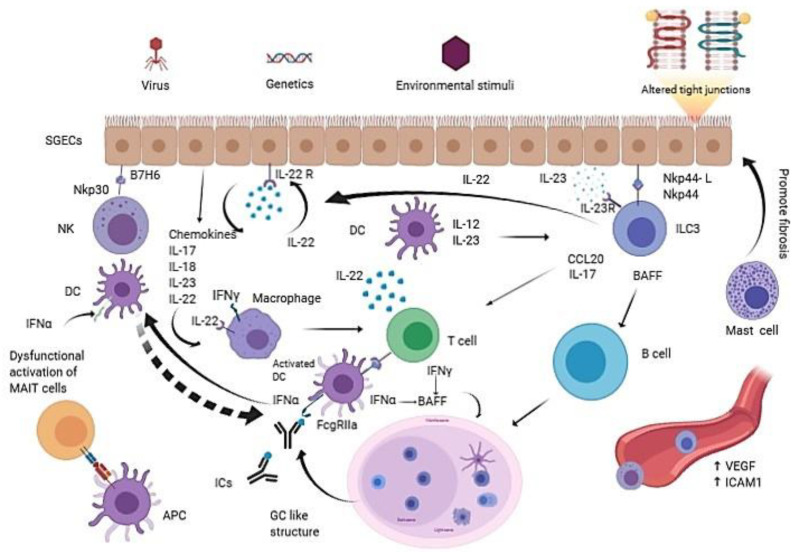
Figure 1.
The interplay between innate immune cells and the inflammation prone microenvironment in Primary Sjogren Syndrome (pSS). pSS is a multifactorial rheumatic disease: environmental stimuli, in genetic susceptible subjects, may trigger Salivary gland epithelial cells (SGECs) to express ligands, receptors and cytokines, such as IL-22, that act in a paracrine and autocrine way when determining the activation of several innate immune cells like NKs, ILC3s, DCs and macrophages. SGECs exhibit a subverted architecture mainly characterized by altered tight junctions. The pro-inflammatory milieu, boosted by a huge production of cytokines and chemokines, promotes the recruitment of more innate immune cells and finally drives the formation of GC-like structures, which are responsible for the in situ autoantibodies release. The aberrant production of VEGF determines chaotic neoangiogenesis; activated endothelial cells express ICAM-1 that mediates immune innate cells tissue infiltration. Mast cells contribute to fibrosis and fatty infiltration of salivary glands. MAIT cells display a dysfunctional activation with a consequent impaired production of protective cytokines. The overall immune response appears to be Th17 polarized, suggesting a pivotal role for this cytokine in pSS. APC: Antigen presenting cell; BAFF: B-cell activating factor; DC: Dendritic cell; GC: Germinal center; ICs: Immunecomplexes; ICAM-1: Intercellular adhesion molecule 1; IL-22R: IL-22 receptor; ILC3: Type 3 innate lymphoid cell; MAIT: Mucosa-associated invariant T cell; SGECs: Salivary gland epithelial cells; VEGF: Vascular endothelial growth factor.