Abstract
Objective
To describe a case of recurrent positive nucleic acid detection in a recovered coronavirus disease 2019 (COVID-19) patient and to provide clinical data for the further study of COVID-19.
Methods
A case of COVID-19 was retrospectively analyzed, and the relevant literature was reviewed.
Results
Based on the 6th edition of the COVID-19 treatment plan, the patient met the discharge standards after treatment and was discharged after consultation with the expert panel. Two weeks after discharge, nucleic acid testing of a sputum sample for severe acute respiratory coronavirus 2 (SARS-CoV-2) was positive again. There may be various reasons.
Conclusion
Recurring positive SARS-CoV-2 nucleic acid tests pose a formidable challenge, and more stringent discharge standards should be considered. When considering recurrent positive nucleic acid results in COVID-19 patients, the clinicians should have a rational judgment.
Keywords: COVID-19, Nucleic acid detection, Recovering positive
At the end of 2019, the outbreak of coronavirus disease 2019 (COVID-19) started in Wuhan, Hubei Province, China [1], and then quickly spread across the country. The number of infections has continued to increase in different cities at different rates. According to the clinical experience, the disease is highly contagious, and some patients develop respiratory failure within a short period. Based on the epidemiological and clinical characteristics of COVID-19, the National Health Commission expert group continuously updated the guidelines for the clinical diagnosis and treatment of the disease, optimizing their effectiveness. The guidelines provide detailed instructions and criteria for treatment and discharge. The severe acute respiratory coronavirus 2 (SARS-CoV-2) nucleic acid test plays a key role in the guidelines, as it is the gold standard for the diagnosis of COVID-19 and is the basis for the most important discharge standard. In this report, a young male patient was confirmed as having COVID-19 according to the sixth edition of the COVID-19 diagnosis and treatment plan [2] and was given standard treatment in a designated hospital. After treatment, the patient achieved the discharge standard. He was discharged from the hospital and received routine follow-up care 1 week after discharge. His sputum sample tested positive for SARS-CoV-2 nucleic acid. After the patient has been cured, a recurrent positive nucleic acid test poses a serious challenge for clinicians. This report provides a detailed analysis of the patient's disease and clinical characteristics, diagnosis and treatment with the aim of providing more data to support the effective control of COVID-19.
1. Case data
The patient, a 24-year-old male student, was admitted to “Shandong Provincial Chest Hospital affiliated with Shandong University” on February 12, 2020. His chief complaint was three days of positive SARS-CoV-2 nucleic acid tests. The patient's grandmother had been diagnosed with COVID-19 4 days prior. The patient was isolated because he had been in close contact in a local hotel. The SARS-CoV-2 nucleic acid test performed with a routinely collected pharyngeal swab was positive. The patient had no obvious cough, sputum production, chest tightness, fever, fatigue or night sweats. The patient was transferred to Shandong Provincial Chest Hospital affiliated with Shandong University for intensive treatment in isolation. The patient was in good health and had no relevant personal or family history. After admission, the physical examination showed a temperature of 36.8 °C, a pulse of 65 beats per minute, a respiration rate of 22 breaths per minute and a weight of 65 kg. In terms of his general condition, the examination showed that he had normal development, good nutrition, normal facial expressions, the ability to express himself, and the ability to independent maintain his body position; he was conscious and cooperative with the physical examination. No systemic superficial lymph nodes were enlarged. There was no wheezing or crackles, the results of auscultation were normal, and there were no dry or wet rales. The physical examination of his abdomen was negative for abnormalities. After admission, the results of the laboratory examinations showed the following: immune function (T cells, B cells and natural killer (NK) cells): T lymphocytes (CD3+) 58.3%↓, helper T cells (CD3+CD4+) 28.5%, auxiliary/inhibitory T lymphocyte ratio 1.11↓, and inhibitory T cells (CD3+CD8+) 25.7(%). The erythrocyte sedimentation rate was 8 mm/h. The routine blood examinations showed the following results: total leukocyte count 4.03×109/L, neutrophil percent 43.0%, lymphocyte percent 39.6%, neutrophil count 1.74×109/L, and lymphocyte count 1.60 ×109/L). His biochemical examinations and myocardial enzyme levels were all normal. On February 14, 2020, the chest high-resolution computed tomography (HRCT) showed that the right lower lung lobe had a limited amount of thin ground glass opacity with blurred edges. No obvious abnormalities were observed in the rest of the lung, and no obvious enlarged lymph nodes were observed in the mediastinum or hilum of the lung (see Fig. 1). According to the clinical symptoms and signs of the patients and the COVID-19 diagnosis and treatment protocol (sixth edition), the patient was diagnosed with mild COVID-19. After admission, the patient's breathing, heart rate, blood oxygen saturation level and other vital signs were monitored. The patient's treatment plan was as follows: human recombinant interferon α-2b (Beijing Cain Technology Co., LTD.) in 2 ml of sterilized water for aerosol inhalation bid for 10 days, oral Arbidol hydrochloride (Shiyao Group Pharmaceutical Co., LTD.) 0.2 for 10 days, oral Lianhua Qingwen Capsule (Shijiazhuang Yiling Pharmaceutical Co., Ltd.) 1.4 for 10 days, thymopentin 1.0 mg intravenous drip qd for 10 days, and charred oral Chinese medicine for 10 days. Test results for the SARS-CoV-2 ORF1ab, E gene and N gene were negative. On February 19, 2020 (24 hours after the first examination), the SARS-CoV-2 nucleic acid test of a pharyngeal swab was negative for ORF1ab, the E gene and the N gene. Chest HRCT was performed again on February 21, 2020, and the lung lesions were significantly more absorbed than at admission (see Fig. 2). According to the COVID-19 diagnosis and treatment plan (sixth edition) issued by the state health department, the patient met the discharge criteria. His body temperature had been normal for more than 3 days, and he had no obvious cough, chest tightness or other respiratory symptoms. Two consecutive SARS-CoV-2 nucleic acid tests of respiratory specimens were negative (at least 24 hours apart), and the patient met the discharge standard. After discharge, the patient was re-examined in the 2nd week (8th day), and the result of nucleic acid testing of a sputum specimen was positive for ORF1ab and the N gene). The patient had no obvious cough, sputum production, fever, chest tightness, fatigue, abnormalities on chest CT or changes on imaging. The patient was in good general condition, with normal diet, sleep, defecation and urination.
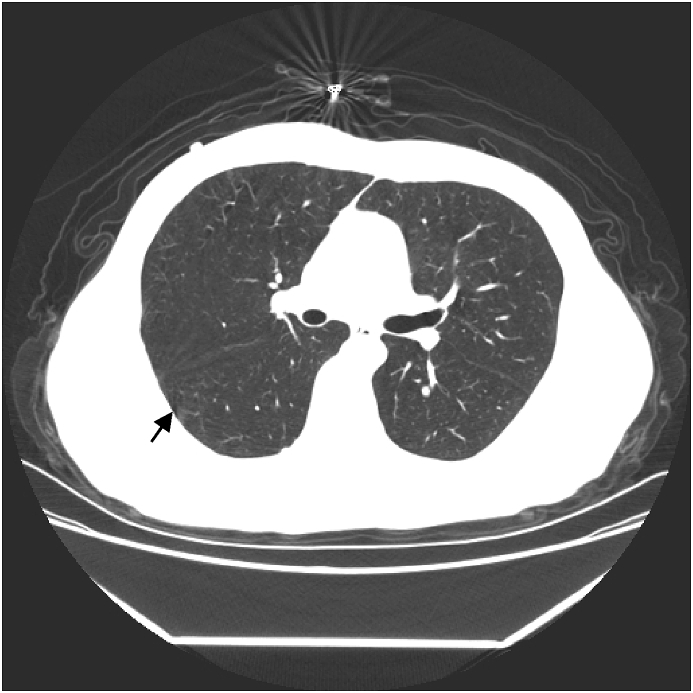
Fig. 1.
Limited ground-glass opacity is seen in the lower lobe of the right lung.
Fig. 2.
Ground glass opacity in the lower lobe of the right lung has clearly been absorbed.
The patient was admitted to the local designated hospital on the same day, and no obvious abnormalities were found in routine blood tests or related indicators, such as C-reactive protein.
At that time, the seventh edition guidelines had not been released, and the patient did not undergo testing for SARS-CoV-2 antibodies. After admission, the patient underwent treatment with interferon α-2b injection and Arbidol hydrochloride for 1 week. Then, two consecutive SARS-CoV-2 nucleic acid tests of respiratory specimens were negative (at least 24 hours apart). The tests for serum SARS-CoV-2 IgM and IgG antibodies were negative. The patient was isolated and rested at home after discharge. During follow-up 1 week later, the patient's condition was stable, but he often felt weak and experienced chest tightness and discomfort when climbing five floors consecutively.
2. Discussion
SARS-CoV-2 is a coronavirus in the β genus. It is enveloped and has round or elliptic virions. It is usually pleomorphic, with a diameter of approximately 60–140 nm, and its genetic characteristics are very similar to those of SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV) [3]. Originally called 2019 novel coronavirus (2019-ncov), it was renamed SARS-CoV-2 [4]. The virus has strong pathogenicity and infectivity. The general population is susceptible, and infected patients become a strong source of infection. The clinical features of this disease are fever, dry cough, and fatigue, and a few patients have a runny nose, sore throat, myalgia and diarrhea. Some patients quickly develop severe or critical cases, with clinical manifestations of respiratory failure and multiorgan failure requiring mechanical ventilation [2]. The National Health Commission expert group developed guidelines based on the characteristics of the disease and the current clinical experience. There are no specific drugs to treat COVID-19 other than general supportive therapies, oxygen therapy, and antiviral treatments with at least 2 antiviral drugs, combined with the careful use of antibiotics and the application of traditional Chinese medicine [2].
This patient was a young man with no chronic diseases and no typical symptoms, such as fever, dry cough, or weakness. Laboratory tests showed that his white blood cell and lymphocyte counts were in the normal ranges, and his chest CT showed limited ground glass opacity. According to COVID-19 diagnosis and treatment guidelines, the patient was diagnosed with mild COVID-19. After admission, the patient's condition was stable, with no discomfort. Antiviral treatment and other oral medicines were administered, and treatments intended to strengthen his immune system were given. After 10 days of treatment, the chest CT was repeated, and the pulmonary lesions had clearly been absorbed. According to the discharge standards in the guidelines, the patient was discharged. The patient continued to be isolated in one location after discharge. During quarantine, a routine reexamination was conducted in the second week, and the sputum sample was positive for SARS-CoV-2 nucleic acid.
The COVID-19 pandemic started in late 2019. Based on current clinical experience, we know that the effect of treatment for this disease is positive. Most of the patients have no obvious sequelae and can be cured. However, as of March 2020, in some parts of China, many cured patients’ nucleic acid tests become positive again. Lan [5] reported four cases. After 3 days, repeated tests were positive, even after performing quality control on the kits and standards. However, the four patients had no obvious clinical manifestations, such as cough, fever, fatigue and digestive tract discomfort, and no ground-glass opacities were observed on chest CT. Because the four patients were isolated, whether they were contagious was not verified. Recovery has been reported in many places in China, such as Shandong, Sichuan, Tianjin, and Guangdong [6,7]. To a certain extent, this phenomenon suggests the need for more stringent requirements for clinicians and causes many researchers and clinicians to experience doubts. According to the current published literature and the clinical characteristics of recurrent positive SARS-CoV-2 nucleic acid tests in patients, this phenomenon may be related to the following factors.
First, the drug treatment guidelines from the National Health Commission expert group never mention the duration of treatment with Arbidol and interferon in the first to the fifth versions, and the antiviral effects of the two drugs are not clear. In the subsequent 6th version, chloroquine phosphate was recommended as an additional treatment, but the duration of antiviral treatment was limited to no more than 10 days [8,9]. In this case, the patient received medical treatment for 10 days, and the entire treatment process involved the administration of Arbidol and interferon. Therefore, in this analysis, it is possible that the treatment during hospitalization reduced the viral load below the limit of detection, resulting in false-negative results. With the continued replication of the virus, the test may become positive again once the viral load reaches the lower limit of detection. Such speculation is based on the fact that both Zika and Ebola viruses have these characteristics. Therefore, the National Health Commission expert group should consider extending the course of antiviral drugs instead of limiting it to 10 days.
Second, some sample-related factors could affect the results [10]. There are two main aspects. First, nucleic acid testing requires sophisticated technology. Nucleic acid is very fragile, but damage to the sample cannot be visualized. In addition, many factors during and after specimen collection, such as accuracy of obtaining the sample, transportation of the specimen, nucleic acid extraction, the quality and purity of the detection reagents and the surrounding laboratory environment, can affect the results [11,12]. Second, for test specimens, which include swab specimens, nasal swabs, sputum samples, tracheal aspirates and so on, the most accurate results are obtained with specimens from the lower respiratory tract. For most COVID-19 patients with dry cough, sputum and lower respiratory tract specimens are more difficult to obtain; in addition, sputum specimens are of poor quality. Due to endotracheal intubation in severely and critically ill patients, standard specimens from the lower respiratory tract can be obtained; however, most COVID-19 patients have mild or moderate cases. Therefore, low-quality specimens may lead to false negatives in patients who are discharged early. Therefore, for some patients, even if the test is negative, the discharge standard should be strictly followed [13].
Third, the immune function status of the patients can affect the results. Many researchers have mentioned the clinical significance of immunity with regard to nucleic acid detection [14,15]. When immune function is low, people are usually relatively more susceptible to COVID–19, and their antibody production time will be extended. This patient was a young man, and while the chest CT showed that there were few lung lesions, the CD4/CD8 ratio was clearly reduced. When immune suppression occurs, the nucleic acid test may become positive again.
Of course, there is not yet a clear explanation for the recurrence of positive nucleic acid tests. Many researchers have analyzed different samples and the clinical characteristics of COVID-19 patients. There are regional differences, indicating that there may be multiple explanations for this phenomenon. A detailed analysis of a large number of samples is needed. With regard to the patient we reported in this paper, the three conjectured explanations are all possible. Although the patient had recurrent positive nucleic acid test results, he still had no clinical symptoms and no changes on chest imaging. Given his current condition, the possibility of this patient being contagious is relatively low. To determine why the nucleic acid test became positive after discharge, an analysis of a large sample of patients is still needed.
To support the diagnosis of COVID-19, in the seventh edition of the diagnosis and treatment guidelines, antibody detection was included. IgM and IgG antibodies can be detected in the serum at different stages after infection with SARS-CoV-2. The positive rate for the diagnosis of COVID-19 can reach 90% and 95% based on IgM and IgG antibodies, respectively [16], and the test is safe and effective, greatly reducing the risk of infection in medical staff. Usually, the test can be completed in half an hour, reducing the test duration and making it useful for screening personnel, including those suspected of having COVID-19. At the end of treatment, the tests for both antibodies were negative in this patient, which confirmed that the patient had been cured and indicated that protective antibodies were not produced by the patient. The relevant mechanism is still unclear.
There is a global pandemic of COVID-19, and thus far, we do not know much about the characteristics of the disease. An increasing number of researchers need to devote more effort to providing better data to support the effective control of COVID-19.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Contributor Information
Teng Geling, Email: tenggeling@163.com.
Hu Hua, Email: huhua2751@126.com.
References
- 1.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health commission PRC. Notice on the issuance of covid-19 diagnosis and treatment plan (trial version 6) http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df35- 1d7da8aefc2.shtml
- 3.Lur Zhao X., Li J. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu N., Zhang D.Y., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.L U.D., Ye G. Positive RT-PCR test results in patients recovered from COVID- 19. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tianjin municipal health commission Two more confirmed cases in tianjin were transferred to the sea after positive nucleic acid reexamination A previous case of fu Yang was discharged from river hospital today. http://wsjk.tj.gov.cn/art/2020/3/2/art_14_71758.html [2020-03-02]
- 7.The south net The press office of the guangdong government held 31 press conferences on epidemic prevention and control. http://gdio.southcn.com/g/2020-02/25/content_190429333.htm [2020-02-25]
- 8.Che K K, Liu X M, Hu C H. Retrospective analysis and pharmaceutical care of anti-novel coronavirus drugs based on the latest diagnosis and treatment scheme [J/OL]. J. Southwest Univ. (Nat. Sci. Ed.):1-9[2020-03-17].http://kns.cnki.net/kcms/detail/50.1189.N.20200305.1427.002.html.
- 9.Zou Q M, Li H B, Zeng H. Research status and countermeasures of covid-19 drugs [J/OL]. J. Third Mil. Med. Univ.:1-6[2020-03-17]. 10.16016/j.1000-5404.202002233. [DOI]
- 10.Morsy Qin W., Fu Q.H. The influence factors of novel coronavirus nucleic acid detection. Chin. J. Lab. Med. 2020;43 doi: 10.3760/cma.j.issn.1009-8158.2020.0002. (00);E002-E002. [DOI] [Google Scholar]
- 11.Kuang H.H., Yu M., Yu S.H. Method and practice of nucleic acid testing in novel coronavirus laboratory. http://kns.cnki.net/kcms/detail/11.3456.R.20200222.1005.002.html 1-4[2020-03-17]
- 12.He C, Jiang H , Xie Y, et al. Study on the laboratory test route for the diagnosis and treatment of covid-19 [J/OL]. J. Respir. Crit. Care China:1-3[2020-03-17].http://kns.cnki.net/kcms/detail/51.1631.R.20200221.1322.002.html.
- 13.Wang D, Dong L, Qing S, et al. Thinking errors in novel coronavirus nucleic acid detection [J]. J. Chin. Hosp. Infectiousness:1-4[2020-03-17]http://kns.cnki.net/kcms/detail/11.3456.R.20200310.0931.002.html.
- 14.Hu J G, Jiang Z S, Li X , et al. Changes and significance of T lymphocyte subsets in peripheral blood of 16 patients with covid-19 [J/OL]. Guangdong Med.:1-3[2020-03-17] 10.13820/j.cnki.gdyx.20200588. [DOI]
- 15.Liu X.P., Wang H.Y., Zhang S.S. Clinical evaluation and analysis of nucleic acid "fu Yang" in discharged covid-19 patients. Henan Med. Res. 2020;29(9):1537–1541. [Google Scholar]
- 16.Health commission PRC. Notice on the issuance of covid-19 diagnosis and treatment plan (trial version 7) http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df35- 1d7da8aefc2.shtml