Abstract
Objective
Insulin access for people with diabetes is a growing public health concern and particularly important for people with type 1 diabetes (T1D) who depend on insulin for survival. However, few studies have examined the psychosocial contexts in which people with T1D confront, navigate, and attempt to resolve insulin access barriers (IABs). We conducted a qualitative study to: 1) describe factors affecting insulin access among adults with T1D, 2) characterize behavioral and emotional responses to IABs, and 3) understand the overall impact of IABs on the lives of adults with T1D.
Methods
We recruited a geographically and age diverse sample of U.S. adults with T1D (n = 21) from online diabetes support groups who self-identified as facing IABs. We conducted semi-structured phone interviews lasting 45–60 min between April and October 2017. We followed an inductive coding approach to identify concepts and themes related to participants' experiences with IABs.
Findings
Participants conceptualized the experience of being without insulin as a “life or death” emergency, which significantly influenced their subsequent behavioral and emotional responses to compromised insulin access. Participants also described multiple IABs including unaffordable health care, institutional unresponsiveness, and major life transitions. Unable to consistently depend on the U.S. healthcare system to address their insulin needs, participants described taking strategic actions to maximize their existing insulin supplies, obtain more insulin, and create long-term security against future IABs. These strategies were not always successful and often negatively impacted participants’ health, finances, careers, relationships, and future opportunities.
Conclusions
Disruptions in insulin access or the threat of future disruption, a concept we term “insulin insecurity,” is a barrier to health and well-being among people with T1D. Our findings suggest the U.S. healthcare system is ill-equipped to address insulin needs among adults with T1D.
Keywords: Type 1 diabetes, Insulin insecurity, Insulin access, Access to medicine, Essential medicines
Abbreviations: T1D, Type 1 diabetes; IAB(s), Insulin access barrier(s); T2D, Type 2 diabetes; DKA, Diabetic ketoacidosis
Highlights
-
•
“Insulin insecurity” is a significant barrier to well-being among U.S. adults with type 1 diabetes (T1D).
-
•
High costs of insulin and healthcare in the U.S. are major barriers to insulin access.
-
•
Insulin insecure people with T1D may resort to extreme, risky measures to access insulin.
-
•
Existing policies, resources, and programs are inadequate for addressing insulin insecurity.
-
•
Immediate measures should be taken to create a safety net for insulin insecure Americans with T1D.
Introduction
Type 1 diabetes (T1D) is an incurable autoimmune disease characterized by the body's inability to produce insulin; a hormone essential for blood glucose regulation and survival (Centers for Disease Control and Prevention [CDC], 2018). An estimated 1.3 million U.S. adults are living with T1D and about 40,000 new cases are diagnosed annually (Bullard, Cowie, & Lessem et al., 2018). Following the breakthrough discovery of insulin as a treatment for diabetes in 1921, T1D was transformed from a fatal condition into a manageable, yet chronic disease (Nathan, 2014). While only 10 to 20 percent of adults with type 2 diabetes (T2D) use insulin to control their blood glucose levels, all people with T1D require insulin replacement therapy to survive (CDC, 2014). Without insulin, people with T1D will die from hyperglycemia within days or weeks (Beran, Ewen, & Laing, 2016). Over time, even short episodes of hyperglycemia can precipitate microvascular complications including heart disease, kidney failure, blindness, nerve damage, lower limb amputations, and potentially fatal diabetic ketoacidosis (DKA) (Nathan, 2014, Umpierrez, Murphy, & Kitabchi, 2002).
Considering these acute and long-term health risks, it is vital that people with T1D have uninterrupted access to insulin. Yet millions of people with diabetes around the world still struggle to procure this life-saving medication (Beran et al., 2016; Cohen, 2011). In low- and middle-income countries, high prices, duties, markups, and transportation and storage costs all create insulin access barriers (IABs) (Beran et al., 2016; Volman, 2008). IABs have also been identified in high-income countries. In the United States (U.S.), rising list prices, high out-of-pocket costs, complex insulin supply chain dynamics, and limited generic alternatives create IABs (Cefalu, Dawes, & Gavlak et al., 2018; Beran et al., 2016).
Over the last two decades, insulin prices in the U.S. have risen exponentially. From 2002 to 2013, the average price per milliliter of insulin nearly tripled from $231 to $736 (Hua, Carvalho, Tew, Huang, Herman & Clarke, 2016). For uninsured or underinsured Americans with diabetes, rising list prices mean higher out-of-pocket costs in the form of prescription co-pays, co-insurance, or deductibles, while uninsured individuals must pay the full cost of their insulin (Cefalu et al., 2018). Between 2012 and 2016, the average annual out-of-pocket cost of insulin per T1D patient increased from $2864 to $5705 (Health Care Cost Institute, 2019). In tandem, insulin utilization has shifted from cheaper human insulin predecessors to more expensive analogs (Cefalu et al., 2018). To date, no competitive generic (i.e., biosimilar) analog or human insulins have been developed; thus, people with T1D are often forced to pay higher prices for brand name insulins (Greene & Riggs, 2015). With 8.5 percent of the U.S. population uninsured and an estimated 29 percent underinsured, inadequate insurance and limited access to healthcare providers can also create IABs (Berchick, Barnett, & Upton, 2019; Collins, Herman, & Doty, 2019).
The U.S. market trends for insulin compounded by limited treatment alternatives and lack of universal healthcare likely have implications for patient self-management and outcomes. Financial barriers to insulin access are prevalent among certain subpopulations of people with T1D and T2D hospitalized for DKA (Randall, Begovic, & Hudson et al., 2011; Musey, Lee, & Crawford et al., 1995) and 30 percent of Americans with T1D or T2D engage in “cost-related insulin underuse” (Herkert et al., 2019).
While these studies illuminate some of the factors that can compromise insulin access and health outcomes for people with T1D and T2D, IABs are likely more problematic for people with T1D. Lacking the same glucose management alternatives available to those with T2D—such as dietary changes, weight loss, exercise, and oral antihyperglycemic medications (CDC, 2019)—it is possible that adults with T1D confront, navigate, and attempt to resolve IABs in meaningfully different ways than those with T2D. Given the unique vulnerability of this population, more research is needed to understand the experiences of IABs among adults with T1D in the U.S. We conducted a qualitative investigation to: 1) describe factors affecting insulin access among adults with T1D, 2) characterize behavioral and emotional responses to IABs, and 3) understand the overall impact of IABs on the lives of adults with T1D.
Methods
We conducted a qualitative study (Sandelowski & Barroso, 2007) recruiting 21 adults with T1D from across the U.S. who self-identified as having problems accessing insulin from April to October in 2017. Eligible participants were men and women ages 18 and older residing in the U.S. who met the following criteria: 1) a self-reported diagnosis of T1D; 2) primarily responsible for their insulin costs with or without health insurance; and 3) experienced ‘difficulties obtaining insulin’ at any point during the last 15 years. We operationalized ‘difficulties obtaining insulin’ as any experience wherein the individual required insulin but could not access their prescribed dosage. The 15-year recall period allowed us to capture a range of experiences that may have occurred during the time when U.S. insulin prices increased exponentially and to understand the long and short-term implications of these experiences on participants' lives. However, most participants described experiences occurring within the last 5 years.
Prior to recruitment, our study protocol was approved by the Yale University Human Investigation Committee. Recruitment advertisements were then posted in online T1D support groups across multiple social media sites including Facebook, Reddit, and Twitter, and on mobile phone applications targeting people with diabetes. Two T1D patient advocacy organizations—Beyond Type 1 and T1International—advertised the study on their social media platforms and webpages. Online advertising enabled us to reach a geographically diverse sample. Participants received a $20 Amazon gift card as compensation.
Data collection
The first author conducted semi-structured phone interviews lasting 45–60 min to explore participants' experiences with and behavioral responses to IABs. We used an interview guide to ensure that similar topics were covered in each interview, but also followed participants’ narratives to examine emergent concepts. The interview guide was informed by the existing literature around IABs and by the lived experiences of individuals with T1D on the research team and their engagement with T1D communities. The interview guide was reviewed by all authors prior to the first interview and refined after the first 5 interviews. All interviews began with the prompt, “Tell me briefly about your experience living with T1D," and then progressed toward specific topics related to insulin access including descriptions and perceptions of times when participants were unable to access insulin, and behavioral and emotional responses to IABs. All interviews were audio recorded using digital recording software and professionally transcribed. Using an approach developed from grounded theory (Corbin & Strauss, 2014), data collection and analysis occurred concurrently. The first author open-coded interview transcripts shortly after they were completed to identify concepts related to IABs. Interviews continued until no new concepts were identified (n = 21).
Data analysis
Our analysis was an ongoing, iterative process that co-occurred with data collection. The first author wrote summaries after each interview and open-coded transcripts to inductively identify initial concepts. Throughout the coding process, the authors held regular team meetings to identify recurrent themes, discuss divergent cases, and collaboratively identify emerging codes. We refined this list of codes to create a codebook. The first author, with input from the other authors, then applied the draft codebook to a small subset of transcripts, revising it twice before finalizing. The first author applied the final codebook to all transcripts using Dedoose software. In developing the themes described below, the first author reviewed coded excerpts and full transcripts to contextualize excerpts within participants’ broader narratives. Ongoing discussion among the authors throughout the analytic process, systematic coding, and systematic review of coded excerpts allowed us to check interpretations against the data and enhanced the rigor of our analysis.
Results
The majority of participants were female (66.7%) and age ranged from 21 to 55 years (Table 1). On average, participants had been living with T1D for 20.4 years (range: 6 months to 36 years). Nineteen participants identified as Caucasian and 2 identified as Hispanic. Participants were geographically dispersed across 14 states. At the time of interview, 10 participants reported having private, employer-based health insurance, 2 were temporarily covered by a continuation of their previous employer's insurance (COBRA), 2 had private, non-employer insurance, 1 was insured through the Affordable Care Act (ACA) marketplace, 2 had Medicaid and/or Medicare (public insurance), 1 had military insurance (TRICARE), and 3 were uninsured.
Table 1.
Characteristics of study population.
| Pseudonym | Gender | Age | Years Living w/T1D | Insurance Status | Race/Ethnicity | State |
|---|---|---|---|---|---|---|
| Patricia | Female | 54 | 17 | Temporary (COBRA) | Caucasian | TX |
| Carlos | Male | 33 | 18 | Private (Employer) | Hispanic | CA |
| Jennifer | Female | 31 | 19 | Temporary (COBRA) | Caucasian | OH |
| Eve | Female | 37 | 34 | Private (Employer) | Caucasian | FL |
| Matt | Male | 35 | 0.5 | Private (Employer) | Caucasian | NC |
| Elizabeth | Female | 21 | 1 | Uninsured | Caucasian | OH |
| Francesca | Female | 34 | 23 | Private (Employer) | Caucasian | OH |
| Lisa | Female | 29 | 17 | Private (Employer) | Caucasian | PA |
| Luis | Male | 27 | 11 | Uninsured | Hispanic | FL |
| Olivia | Female | 26 | 23 | Public (Medicaid) | Caucasian | IL |
| Jack | Male | 25 | 20 | Private (Non-employer) | Caucasian | CO |
| Stella | Female | 47 | 34 | Public (Medicare/Medicaid) | Caucasian | TX |
| Mary | Female | 35 | 27 | Private (Employer) | Caucasian | PA |
| Alecia | Female | 34 | 23 | Public (TRICARE) | Caucasian | GA |
| Rachel | Female | 37 | 26 | Private (Employer) | Caucasian | PA |
| Katherine | Female | 35 | 24 | Private (ACA Marketplace) | Caucasian | KY |
| Caroline | Female | 55 | 10 | Private (Employer) | Caucasian | MO |
| Sarah | Female | 30 | 18 | Private (Non-employer) | Caucasian | UT |
| Darren | Male | 39 | 23 | Uninsured | Caucasian | WA |
| Joseph | Male | 38 | 36 | Private (Employer) | Caucasian | FL |
| Daniel | Male | 31 | 24 | Private (Employer) | Caucasian | NY |
In the sections below, we first describe the “life-or-death” necessity of insulin, a central theme of the study that significantly shaped participants' experiences of IABs. Next, we examine factors that led to interruptions in insulin access and the coping strategies participants employed to navigate and prevent these interruptions. Finally, we illustrate the impact of these strategies on participants' lives, including their physical and mental health. To protect participants’ anonymity, we use pseudonyms in presenting our results.
Life or death
Participants collectively described insulin as a unique, life-saving medication and the experience or threat of being without insulin as a life-threatening emergency. For example, Lisa said, “…to just know that one hormone that you need to survive is out of your reach is really scary. And you know, I've always thought about insulin like this. People with [T1D] aren't taking something in addition to everything else in their bodies, so it's not like Metformin, which is an additional sort-of foreign substance that people with [T2D] or pre-diabetes take … it's like people with T1D are missing this essential hormone that everyone else makes …”
Participants emphasized the immediacy of their insulin needs and the imminent risk of health complications if left unaddressed. For example, Sarah said, “…when you have a medication like insulin, it is life or death, especially for type 1s. It can have immediate effects and we need immediate action no matter what … some medications you can wait overnight, but insulin … if you stop taking it, you immediately start getting sick.”
Given the immediate, life-or-death need for insulin, many participants expressed a willingness to take desperate measures to secure insulin and avoid health complications. For example, Carlos stated, “…we're dependent on insulin to live. When that insulin is taken away or you can't obtain it … you almost want to do anything to live … you look for any kind of method to get insulin.” Carlos's desperation to obtain insulin was echoed by other participants who reported engaging in risky or out-of-character behaviors when faced with IABs. For example, Daniel noted, “I'm someone who is very proud and would never ask for money or anything like that, but when it comes to insulin, something that is required to live, then all pride goes out the window.”
Participants also described how the life-or-death nature of their insulin dependency could contribute to significant psychological distress. For example, Patricia described the process of managing her insulin needs as “walking a tightrope.” She explained, “From the time I get up, to the time I go to bed, and in the middle of the night when I'm asleep, I'm still walking it. It's day in and day out, there's no relief.” Similarly, Alecia reported, “…if I didn't have to worry about the cost of insulin, I would probably actually be able to sleep in peace at night.”
Even when participants resolved their IABs, fear of future disruptions could also induce psychological distress. For example, Darren reported that his challenges accessing insulin left him with “post-traumatic stress disorder.” Similarly, Eve explained, “The stress level, it was unbearable … And I got depressed sometimes because, you know, I would be low on money or, you know, worried about when this good insulin was gonna come to an end …”
Notably, several participants commented that IAB-related stress could affect their blood glucose levels. As Alecia explained, “…stress-related issues make my blood sugar plummet and they either go really, really low or sometimes for some crazy reason they go really, really high. And … dealing with all of these crazy situations it gets really, you know, it gets stressful.”
These life-or-death circumstances encompassing the unique, essential need for insulin and feelings of fear, desperation, and psychological distress significantly influenced how participants experienced and subsequently managed IABs.
Insulin access barriers
Several factors prevented participants from accessing insulin including unaffordable health care, a lack of institutional responsiveness, and major life transitions.
Unaffordable health care
All participants cited the high cost of health care as a primary IAB. Self-reported out-of-pocket monthly costs for insulin ranged from $75 to over $2000 depending on participants' insulin requirements and insurance coverage. These expenses were often compounded by the cost of equipment necessary for dosing and delivering insulin such as glucose monitors, test strips, syringes, and insulin pumps. Luis, who was uninsured at the time of the interview said, “…even if I didn't have to pay my bills, I would never be able to afford just my insulin out-of-pocket, let alone my pump supplies, syringes, anything else.”
Some participants identified the costs of seeing a physician for their diabetes management as an additional IAB. For example, Carlos reported, “You need a doctor in order to give you a prescription … you need an endocrinologist to help you figure out the kind of dosage to take … all of this stuff is too expensive.”
Even participants with health insurance reported difficulties accessing insulin due to high premiums, deductibles, co-payments, and coverage limitations imposed by providers. For example, one participant reported that his employer-based health insurance required a $5000 deductible and only covered generic drugs, thereby excluding analog insulin. Another participant reported an allergy to the insulin brand covered by her insurer, which required her to pay out-of-pocket for an uncovered insulin brand.
Several participants also reported paying out-of-pocket for insulin when they exceeded the amount their insurance would cover. Many participants emphasized that their insulin needs fluctuated daily depending on their diet and activity levels, sometimes leading to using more insulin than prescribed. Participants also cited accidents—such as breaking, losing, or denaturing a bottle of insulin by exposure to extreme temperatures—as factors that could compromise their monthly supply. Some participants reported that insurance companies refused to cover additional refills in these situations. As Alecia recounted, “Three different occasions I've gotten the insulin and I've met the post office man, and guess what? The ice packs in there have been depleted … They're not cold at all, and the insulin's ruined, and [my insurer] will not replace it.”
Finally, many participants highlighted how insulin costs competed with other expenses, including household bills, treatment for other health conditions, and the health needs of other family members. For example, Matt described the cost trade-offs of paying for insulin versus his pregnant wife's health care. He said, “Even with my insurance … this year alone, my out-of-pocket has been about $1200 in 6 months, which is a lot. I mean, my wife's entire prenatal care is going to be like $4000 … I'd much rather spend $4000 on a baby than $4000 on insulin.”
Several participants reported that insulin and diabetes supplies accounted for a large portion of their income. Daniel calculated his annual diabetes-related expenditures to be 10 percent of his salary. Similarly, Sarah reported that her monthly out-of-pocket costs for 4 vials of insulin was roughly equal to her housing expenses.
Institutional unresponsiveness
In addition to financial barriers, many participants reported a lack of institutional responsiveness to the life-or-death nature of disrupted insulin access. Participants described institutions such as hospitals, pharmacies, health insurance providers, pharmaceutical companies, pharmacy benefit managers (PBMs), and public health organizations as gatekeepers who could create IABs through bureaucratic errors, procedural delays, miscommunication, ineptitude, or failure to provide appropriate information. Many participants reported feeling that these institutions did not understand T1D or the immediacy of their insulin needs.
For example, when Rachel tried to access insulin after being mistakenly dropped from her insurance coverage, her insurance provider was not responsive to this emergency. She explained, “…when you call your insurance company, you get someone in customer service who doesn't know anything about diabetes and … just has their script. And so … I said, ‘Listen, I need to pick up my insulin. This is a medication that keeps me alive. I can't wait three days to resolve this … ’ And someone left a message for a manager. Someone said they'd call back and, in my experience, you don't really get return phone calls …”
In criticizing the customer service “script,” Rachel noted that existing insurance provider protocols were insufficient for resolving IABs. Emphasizing the lack of T1D knowledge, training, and experience of the managers tasked with helping her, she continued, “They have never had diabetes, they do not have a medical degree. They've probably never even talked to a diabetic … and how do you make your case to someone who is decidedly ignorant about your disease and what is required?”
Like Rachel, other participants described dismissive or indifferent responses when attempting to navigate bureaucratic IABs. For example, Alecia, whose insulin delivery was unexpectedly delayed by 2-weeks, recounted, “My insulin has yet to make it to me. I've called. I've cried. I've acted crazy. And you get a different answer depending on who you get to answer the phone … if I break a bottle of insulin, I have literally had [my PBM] tell me, ‘Well, it sucks to be you, doesn't it?’”
Luis described facing similar unresponsiveness and potentially dangerous delays at a local emergency room when he lacked insulin access. He said, “I walked in, I told them my blood sugar is over 600 [mg/dl]. The lady at the front desk looked at the lady next to her and was like, ‘um, shouldn't he be dead?’ … So I thought I was gonna get help and they left me sitting there for 4 hours. For 4 hours! I got up and I left.” Additionally, many participants reported being denied hospital treatment because their glucose levels were still in a normal range and no immediate medical emergency existed. Others described being placed on a temporary insulin drip to stabilize their glucose levels but were not allowed additional vials to take home.
Some participants reported that public health and patient assistance programs were also unresponsive to IABs. For example, Olivia attempted to obtain insulin from several public assistance programs when she accidently froze her supply while traveling, but none were able to help. She said, “…we called the public health [department] for her county, we called the pharmacy to see if they had any samples or coupons or anything. We called UNICEF … and we actually called the insulin company. And we explained the situation and we asked if they could give us a coupon code for one single bottle. That's all we needed, right? And it was like, every time we turned around, it was like, ‘Sorry, we don't do that. Sorry, we can't help you.’”
Life transitions
Major life transitions including job loss, divorce, death of a family member, changes in insurance provider or level of coverage, geographic relocation, and loss of social security benefits also affected participants’ insulin access. These changes often exposed participants to a greater proportion of their insulin costs or additional institutional barriers.
For example, Jennifer described a time when she was unable to access insulin after moving. She explained, “…I had a gap in time where I had moved away from my endo[crinologist], and I had moved into the city, and I was, like, ‘Wow, I don't have access to anything, or lined up like I did right before’ … it was just a gap between moving, getting a job, and I had a couple months' gap in-between when my insurance start[ed].”
Multiple participants described the loss of parental health insurance as a transition that disrupted their insulin access. While the Affordable Care Act (ACA) expanded access to care by allowing young adults to remain on parents' insurance until age 26, even with an additional 8 years of coverage, some participants were still unable to afford insulin once that coverage ended. As Lisa explained, “…when you're in high school hopefully you're covered by your parents' insurance and that's okay, you never have to think about the cost of insulin … the ACA coverage was extended until age 26, but at 26 you're cut off from parents' [insurance] coverage and you're either having to buy an exchange plan, which is super expensive, or hopefully get a job that has health insurance coverage, and people with diabetes are just kind-of on the backburner in these life transitions.”
Some participants also described the transition from pediatric to adult care as an IAB. For example, in recounting her first time seeing an adult endocrinologist after being dropped from her parent's health coverage, Eve explained, “I remember the first endocrinologist I went to, as a maybe, like, 18 or 19-year-old … he had no idea what to do with me. I remember sitting there, and he's trying to give me advice … he clearly had no idea what he was talking about. And I'm like, ‘He doesn't know shit about type 1—this guy's an idiot!’ … I was probably one of the few type 1s that he saw … and then on top of it I'm explaining to him, ‘Look, I'm having trouble getting insulin, you know, I can't afford it.’ And again, this is a problem he probably was never really faced with.”
Coping strategies & consequences
Participants responded to these various categories of IABs with creative and strategic actions intended to: 1) maximize existing insulin supplies; 2) obtain more insulin; and 3) prevent future disruptions in insulin access. These coping strategies were not always successful and often resulted in consequences to participants’ health, finances, relationships, and future opportunities.
Maximizing insulin
Participants described several strategies to maximize or ration their existing insulin and diabetes supplies, often risking short and long-term health consequences for a few extra days or weeks of insulin access. For example, Patricia reported using less insulin than prescribed to extend her supply. She explained, “...I was skimping on insulin … I was trying to make that vial last a week-and-a-half, so instead of taking what I should have taken, I was using less, you know?”
When Caroline was homeless and unable to afford medications, she resorted to using insulin that was denatured by high temperatures, explaining, “I made sure that I just took whatever insulin I could get in me. I mean, it sat in my car while it was hot in the middle of summer, and I still took it ‘cause I figured even a little potency was better than no insulin.” Other participants reported using expired insulin when unable to access new refills.
In her efforts to maximize insulin stores, Sarah extracted old insulin from her used pump cartridges to avoid wasting the small amount that would otherwise be thrown away. She explained, “…when you change your [insulin] pump cartridge, there's always at least 20 units of insulin left in that cartridge, even though the pump is reading at zero. And so, I would pull the extra insulin out of that cartridge to push into a new cartridge. And that would help me save on insulin.”
Several participants also attempted to maximize their insulin by minimizing their daily insulin requirements. They reported eating low-carbohydrate foods, skipping meals, or exercising excessively. For example, Lisa described carefully limiting her carbohydrate intake noting, “…my insulin was easily $300 or $400 every time I would fill it and so I found myself rationing insulin, and I think probably that's really when my low-carb diet started to get really extreme because I'm like, ‘Well I can eat this piece of cake and take 7 units [of insulin] or I cannot, and have those 7 units for tomorrow … ’”
As Lisa reported, these dietary adjustments could be extreme. For example, to maximize the single vial of insulin that he received after being discharged from the hospital with DKA, Luis severely reduced his food intake explaining, “…I barely ate just to stretch it out to about two weeks, because one vial would usually last me … between like four and eight days, and after that vial ended, that's when things got really rough. I was living off water and an eight-pack of crackers for about four days.”
In addition to maximizing insulin, participants also reported strategies to ration their insulin dosing supplies. For example, Lisa reported, “I wouldn't test [my blood sugar] because I would have, like, 100 test strips and, in my mind … it was like, 100 test strips is $100.”
While maximizing strategies allowed some participants to temporarily extend their insulin supplies, participants also described how these behaviors could have negative health consequences. For example, Olivia was admitted to the hospital with life-threatening hyperglycemia after going without insulin for several days after her supply was stolen. She said, “…in my head I was like, ‘Oh, I just won't eat very much. I'll eat lunch meat and stuff that doesn't have carbs in it and it'll be okay for a little bit, at least,’ and then I ended up in the hospital and my blood sugar was, like, 700-and-something.”
Some participants also reported experiencing long-term health issues related to their maximizing strategies. For example, Patricia described how years of insulin rationing led her to develop permanent diabetes-related complications. She explained, “I literally would spend 3 to 6 hours a day walking, and as long as I walked, my blood sugar was generally under 140[mg/dl]. But in the evenings … I would still be up around 300 a couple hours later, so … I do believe that my health suffered some during that time. I started developing neuropathy in my feet.”
Strategically obtain insulin
In tandem with maximization strategies, many participants strategically activated financial, social, and institutional resources to obtain more insulin. In activating financial resources, participants charged insulin costs to credit cards, took out loans, sacrificed other expenses, and sold assets. For example, Sarah took on debt to pay for insulin, explaining, “…stuff like overdrawing my accounts knowing I don't have the funds there, but taking the hit to my account anyways, you know, using a credit card I know that I can't really afford to pay off …” Similarly, Alecia explained, “I have racked up credit card debts like you wouldn't believe to the point we're talking to the tune of a little over $40,000 of things … for my diabetes that I needed to live. And I just spoke yesterday to a bankruptcy attorney and that's the best idea is to just file bankruptcy.”
Along with drawing on financial resources to purchase insulin, some participants sought free insulin samples through clinics, hospitals, emergency rooms, and patient assistance programs. Some participants were able to temporarily receive free or reduced-cost insulin through these programs. However, others reported being denied assistance due to strict eligibility criteria. Others noted the limitations of this temporary aid. For example, Patricia explained, “…for a short period of time, about a year, I got my insulin free through the patient assistance program. But then that came to an end, and I was right back where I started.”
In attempting to obtain insulin with less impact to their financial resources, some participants also sought cheaper, alternative sources abroad. For example, Eve said, “I got hooked up with a relatively reputable Canadian pharmacy … and my doctor would give me the prescription, I would fax it to this online pharmacy, and they would mail me insulin.” Others reported switching to over-the-counter human insulins, which could be obtained at Walmart for around $20 to $25 a vial. For example, Jennifer said, “…I didn't have access to Humalog or insurance or my Lantus. So, [I began] using over-the-counter [human] insulin, which is, you know, that 40-year-old insulin from Walmart, which, I mean, saves your life, but it's not the same stuff that's keeping us alive and healthy for a long time, but it's kind of a … desperate measure type thing.” As Jennifer noted, switching from analog to human insulin was considered undesirable and a few participants reported poorer glucose control while using it.
In seeking to obtain insulin, participants also leveraged their relationships with health care providers, friends, family members, and fellow members of the diabetes community. For example, Carlos obtained free insulin through a long-time relationship with his physician. He explained, “I would drive out to my endocrinologist's office and it would be kind of like we were doing a drug deal except there was no money being exchanged. They would put the insulin in, like, a brown paper bag, very nondescript, and hand it to me as I went into their office, and then … I would have this insulin, and I would be able to live for the next couple of months.”
Similarly, after Alecia maxed out her credit cards, her family and friends stepped in to provide her with additional financial resources at the expense of her father's own medical needs. She explained, “… my dad would do without his heart and cholesterol medicine before he would let me do without insulin.” However, this arrangement was also a source of psychological distress for Alecia who reported, “... I feel guilty for what my family and my friends … how they come together and help. It makes me feel bad because I'm like, what are they giving up in their life to help me?”
Other participants drew on relationships within the T1D community to access insulin. For example, Olivia described intentionally befriending a woman with T1D to access her insulin supply, which ultimately led to a mutually agreed upon insulin sharing arrangement. She explained, “I would go over there roughly three times a week. And every time … I would find a way to get myself a shot [of her insulin] … She just caught me using it and she was like, ‘What the f*ck are you doing?’ And I explained to her that I didn't have medication … and then she was like, ‘You could have just asked me.’ And so, after that it was an arrangement because she understood where I was at.”
Notably, multiple participants reported obtaining insulin illegally from other patients through alternative online markets. As Patricia explained, “…there's all this underground, kind-of, quiet stuff going on … but some of it's not quite legal … in that [diabetes supply trading] group, there are people who will post saying … ‘I have these test strips’—and they'll list the strips they have— ‘and I also have a vial of Humalog and a couple vials of NovoLog. If you want to trade, let me know.’” However, some participants expressed concern that these individuals might be selling contaminated or fake insulin. For example, Alecia said, “I want my stuff from a pharmacy. That's all I know. I don't want it from Billy Bob that lives in California …”
Creating long-term security
Given the vital need for insulin, many participants worked to create long-term security against future IABs. Some participants took steps to acquire a surplus of insulin to prevent future shortages. For example, Darren explained, “After that experience in Ohio, where I couldn't find the insulin, it kind of put me in a mode where I was like, ‘I need to get as much of this as I possibly can … so I tell my doctor I take four vials of insulin a month. I usually take maybe about two, two-and-a-half, maybe, a month, so that leaves me like one-and-a-half vials … to have for spare, and then if something happens … I'll have something to get me through until I can figure something else out.”
Given the pervasiveness of factors that could interrupt insulin access, many participants systematically organized their lives to prevent these interruptions. For example, one participant reported secretly marrying her fiancé earlier than planned so she could be covered by his insurance. Similarly, Eve's decision about which college to attend was shaped by insulin access concerns. She explained, “I didn't go to a school that I wanted to go to for undergrad because I knew that I would have to take out money to pay for insulin and medical care. So, I went to a lower-ranked college because they were willing to give me pretty much a complete scholarship.”
In some cases, the necessity of having adequate insurance dictated employment decisions. For example, Carlos said, “…the only reason that I'm working my job currently—it's a job that I don't hate, but I dislike it—and the only reason I'm there is because I'm afraid to get off of it because there goes my insurance, there goes my method to get any kind of insulin or supplies for anything.”
Similarly, Rachel described how the need for insulin shaped her career choices, causing her to leave one job for another to receive better benefits. She said, “…my career is being dictated by the fact that I have a preexisting condition … at this point and for the foreseeable future, I'm not going to be able to have the career that I want because I have to put the need to pay for insulin first.”
Discussion
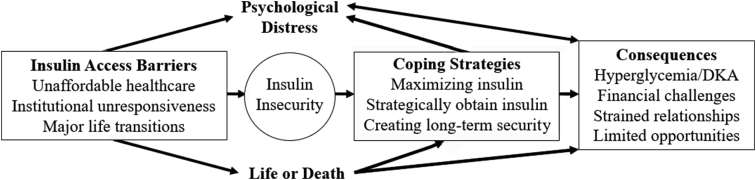
High costs of insulin and health care in the U.S. present significant barriers to insulin access for adults with T1D (Beran et al., 2016; Cefalu et al., 2018). Given the life-or-death necessity of insulin and the distress associated with disruptions in insulin access, participants in this study responded in creative and strategic ways to maximize their existing supplies of insulin, obtain more insulin, and guard against future IABs. However, these strategies were not always successful at securing insulin access and often had negative consequences for participants’ health, finances, careers, and relationships. Fig. 1 summarizes the relationship between the IABs that participants encountered, the coping strategies employed to navigate them, and the consequences of those strategies, all of which contributed to psychological distress. As Fig. 1 illustrates, the life-or-death nature of compromised insulin access affected both the coping strategies participants utilized and the consequences they were willing to accept.
Fig. 1.
Relationship between study themes.
Our findings suggest that uncertain access to insulin, a concept we refer to as “insulin insecurity,” is a significant and immediate threat to health and well-being among individuals with T1D. We define insulin security as having consistent access to sufficient and safe supplies of insulin without anxiety about future loss of access. In comparison, many participants in our study were insulin insecure, experiencing significant disruptions in access, resulting in high levels of anxiety and distress, and often the inability to adequately control their blood glucose levels. While our study was not designed to examine the prevalence of these experiences, we observed insulin insecurity among participants from different geographic locations and with varying insurance coverage levels.
Unable to consistently rely on the healthcare system to facilitate insulin access, participants turned to non-traditional and sometimes dangerous alternatives to maximize, obtain, or maintain insulin security. Among these concerning behavioral responses, participants’ reliance on underground markets to purchase or trade insulin and diabetes supplies from other people with T1D raises several safety and regulatory issues. Litchman and colleagues (Litchman, Oser, Wawrzynski, Walker, & Oser, 2019), who identify “diabetes-specific financial stress” as a key predictor of engagement in underground supply trading, suggest the existence of alternative markets indicates a failure of the U.S. healthcare system to support access to essential medicines for people with diabetes. Furthermore, strategies like rationing or using expired or denatured insulin simultaneously placed participants at high-risk of developing hyperglycemia, DKA, and long-term complications. These strategies may contribute to the already high burden of diabetes and diabetes-related complications in the U.S. (American Diabetes Association [ADA], 2018). Finally, our findings demonstrate that insulin insecurity can lead participants to sacrifice career opportunities and compromise their relationships, safety, values, and goals in their attempts to reduce the risk of future insulin access disruptions. While T1D is considered a qualified and protected disability under the Americans with Disabilities Act (ADA, 2013), people with T1D may still be disenfranchised in several domains based on their need for insulin.
Ultimately, our findings suggest a failure of the U.S. healthcare system to guarantee access to insulin and an urgent need to protect insulin insecure adults with T1D. Preliminary steps might include disseminating timely and relevant information, training, and resources for addressing IABs among gatekeepers. For example, physicians, pharmacists, hospital personnel, and advocacy groups could educate adults with T1D about less expensive over-the-counter human insulins as an emergency alternative to avoid hyperglycemia and DKA. Many participants were unaware of the existence of these earlier generation insulins or how to use them effectively; however, a few participants reported poorer glucose control while taking human insulins.
In tandem, steps should be taken to improve the accessibility of analog insulins for people with T1D. Some possible strategies include the creation of emergency insulin dispensaries in hospitals and pharmacies and amending prescription regulations to allow analog insulins to be accessed over the counter. Such policies have precedent. For example, after a young man with T1D died due to lack of insulin refills in Ohio, drug policies were amended to allow pharmacists to dispense up to a 30-day supply of insulin with an expired prescription (HB 188, 2016). Furthermore, insurance providers could make insulin a deductible-exempt medication and eliminate caps on monthly insulin refills. Special resources and programs are also needed to help young adults with T1D navigate the transition from pediatric to adult care without disrupting insulin access.
While these solutions would be important first steps in creating a temporary safety net for insulin insecure Americans with T1D, they do not overcome all IABs described by participants in this study, particularly the long-term unaffordability of insulin. Since our data were collected, some state laws have been passed to cap out-of-pocket insulin costs for insured people with diabetes (Romo, 2019). Additionally, insulin manufacturers have recently announced analog price reductions after decades of increases (Jacobsen and Erman, 2019). However, in the absence of regulatory intervention, greater generic competition, and more widespread healthcare reform, additional strategies need to be developed to improve insulin affordability and guarantee insulin security for all people with T1D in the U.S., irrespective of geography or insurance status. As Beran, Hirsch, and Yudkin (2018) suggest, access to insulin should be framed within the wider healthcare system and both governments and advocacy groups can play an important role in lowering medication prices.
Beyond insulin pricing, our data suggest that expanded health care access is critical to addressing insulin insecurity. For many participants, IABs were related to lack of adequate insurance benefits. While most of our participants experienced IABs despite having health insurance, IABs are likely to be more pronounced among the 27.5 million Americans who lack any form of health insurance (Berchick et al., 2019).
While this paper provides important insights into the experiences of adults with T1D in the U.S., it has limitations. First, our data may not capture the full range of experiences of insulin insecure adults with T1D or those of diverse race and ethnicity. For example, participants who were highly insulin insecure may have been particularly motivated to participate. Second, as with all interview-based studies, our results are based on participants’ accounts of their behaviors, rather than direct observation. Third, though not the purpose of qualitative data, our study does not allow us to quantify the burden of insulin insecurity among people with T1D in the U.S. Future studies may want to use our findings to quantify and expand on the concept of insulin security.
Finally, our data may not speak to the experiences of individuals with T1D in non-U.S. contexts. Indeed, many of the barriers that our participants described may not exist in countries with universal healthcare or restrictions on insulin pricing. For example, a 2018 survey of individuals with T1D from 90 countries found that 25 percent of U.S. participants reported rationing insulin in the last year compared to 6 percent of participants from other high-income countries (T1International, 2018). Nonetheless, 22 percent of participants in low- and middle-income countries reported insulin rationing, suggesting that some of our participants’ experiences may not be entirely unique to the U.S. Further qualitative research is needed to examine experiences of IABs in other countries.
Despite these limitations, our results provide novel insight into the barriers that prevent adults with T1D from accessing insulin and the strategies they employ to overcome these barriers, which can inform advocacy efforts, public policy, and clinical practice.
CRediT author statement
Samantha Willner, MPH: Conceptualization, Methodology, Formal Analysis, Investigation, Funding Acquisition, Writing – Original Draft, Writing– Review & Editing, Visualization. Robin Whittemore PhD, APRN, FAAN: Conceptualization, Supervision, Writing – Review & Editing, Danya Keene, PhD: Conceptualization, Methodology, Formal Analysis, Supervision, Writing – Original Draft, Writing -Review & Editing
Funding
This research was funded with a grant from the Society for the Psychological Study of Social Issues (SPSSI).
Declaration of competing interest
None.
Contributor Information
Samantha Willner, Email: samanthaWillner@aya.yale.edu.
Robin Whittemore, Email: Robin.Whittemore@yale.edu.
Danya Keene, Email: Danya.Keene@yale.edu.
References
- ADA . 2013, September 27. Fact sheet: Diabetes, discrimination, and public places and government programs.http://main.diabetes.org/dorg/PDFs/Advocacy/Discrimination/factsheet-diabetesdiscriminationandpublicplacesandgovernmentprograms.pdf Retrieved October 28, 2019 from. [Google Scholar]
- American Diabetes Association (Ada) Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. doi: 10.2337/dci18-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beran D., Ewen M., Laing R. Constraints and challenges in access to insulin: A global perspective. The Lancet Diabetes & Endocrinology. 2016;4(3):275–285. doi: 10.1016/s2213-8587(15)00521-5. [DOI] [PubMed] [Google Scholar]
- Beran D., Hirsch I.B., Yudkin J.S. Why are we failing to address the issue of access to insulin? A national and global perspective. Diabetes Care. 2018;41(6):1125–1131. doi: 10.2337/dc17-2123. [DOI] [PubMed] [Google Scholar]
- Berchick E., Barnett J., Upton R. Vols. 60–267. US Census Bureau; 2019. https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf (Health insurance coverage in the United States: 2018, current population reports). Retrieved May 22, 2020 from. [Google Scholar]
- Bullard K.M., Cowie C.C., Lessem S.E., Saydah S.H., Menke A., Geiss L.S.…Imperatore G. Prevalence of diagnosed diabetes in adults by diabetes type — United States, 2016. Morbidity and Mortality Weekly Report. 2018;67(12):359–361. doi: 10.15585/mmwr.mm6712a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cdc . 2014. National diabetes statistics report.https://www.cdc.gov/diabetes/pdfs/data/2014-report-estimates-of-diabetes-and-its-burden-in-the-united-states.pdf 2014. Retrieved April 21, 2018 from. [Google Scholar]
- Cdc . 2018. March 28). Type 1 diabetes.https://www.cdc.gov/diabetes/basics/type1.html Retrieved 23 March, 2018 from. [Google Scholar]
- Cefalu W.T., Dawes D.E., Gavlak G., Goldman D., Herman W.H., Nuys K.V.…Yatvin A.L. Insulin access and affordability working group: Conclusions and recommendations. Diabetes Care. 2018;41(6):1299–1311. doi: 10.2337/dci18-0019. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (Cdc) 2019, May 30. Type 2 diabetes.https://www.cdc.gov/diabetes/basics/type2.html Retrieved 24 October 2019 from. [Google Scholar]
- Cohen D. The prickly problem of access to insulin. BMJ. 2011;343 doi: 10.1136/bmj.d5782. D5782-D5782. [DOI] [PubMed] [Google Scholar]
- Collins R., Herman B., Doty M. The Commonwealth Fund; 2019. Health insurance coverage eight years after the ACA: Fewer uninsured Americans and shorter coverage gaps, but more underinsured. [DOI] [Google Scholar]
- Corbin J.M., Strauss A.L. 4th ed. Sage Publications; Los Angeles, CA: 2014. Basics of qualitative research: Techniques and procedures for developing grounded theory. [Google Scholar]
- Greene J.A., Riggs K.R. Why is there no generic insulin? Historical origins of a modern problem. New England Journal of Medicine. 2015;372(12):1171–1175. doi: 10.1056/nejmms1411398. [DOI] [PubMed] [Google Scholar]
- Health Care Cost Institute . 2019. January). Spending on individuals with type 1 diabetes and the role of rapidly increasing insulin prices.https://healthcostinstitute.org/research/publications/entry/spending-on-individuals-with-type-1-diabetes-and-the-role-of-rapidly-increasing-insulin-prices Retrieved 28 October, 2019 from. [Google Scholar]
- Herkert D., Vijayakumar P., Luo J., Schwartz J.I., Rabin T.L., Defilippo E., Lipska K.J. Cost-related insulin underuse among patients with diabetes. JAMA Internal Medicine. 2019;179(1):112. doi: 10.1001/jamainternmed.2018.5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua X., Carvalho N., Tew M., Huang E.S., Herman W.H., Clarke P. Expenditures and prices of antihyperglycemic medications in the United States: 2002-2013. Journal of the American Medical Association. 2016;315(13):1400. doi: 10.1001/jama.2016.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen S., Erman M. 2019, September 6. Novo Nordisk to cut insulin prices in the U.S.https://www.reuters.com/article/us-novo-nordisk-usa/novo-nordisk-to-cut-insulin-prices-in-the-u-s-idUSKCN1VR1JO Retrieved November 26, 2019, from. [Google Scholar]
- Litchman M., Oser T., Wawrzynski S., Walker H., Oser S. The underground exchange of diabetes medications and supplies: Donating, trading, and borrowing, oh my! Journal of Diabetes Science and Technology. 2019 doi: 10.1177/1932296819888215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musey V.C., Lee J.K., Crawford R., Klatka M.A., Mcadams D., Phillips L.S. Diabetes in urban African-Americans: Cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Diabetes Care. 1995;18(4):483–489. doi: 10.2337/diacare.18.4.483. [DOI] [PubMed] [Google Scholar]
- Nathan D.M. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: Overview. Diabetes Care. 2014;37(1):9–16. doi: 10.2337/dc13-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall L., Begovic J., Hudson M., Smiley D., Peng L., Pitre N.…Umpierrez G. Recurrent diabetic ketoacidosis in inner-city minority patients: Behavioral, socioeconomic, and psychosocial factors. Diabetes Care. 2011;34(9):1891–1896. doi: 10.2337/dc11-0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revises Pharmacist Consult Agreements Dispensing drugs No Rx, HB 188, GA 131. 2016. https://www.legislature.ohio.gov/legislation/legislation-summary?id=GA131-HB-188 March 23). Retrieved from.
- Romo V. Colorado caps insulin Co-pays at $100 for insured residents. 2019, May 24. https://www.npr.org/2019/05/24/726817332/colorado-caps-insulin-co-pays-at-100-for-insured-residents Retrieved November 25, 2019, from.
- Sandelowski M., Barroso J. Springer; New York: 2007. Handbook for synthesizing qualitative research. [Google Scholar]
- T1International . 2018. Costs and rationing of insulin and diabetes supplies: Findings from the 2018 T1International patient survey.https://www.t1international.com/media/assets/file/T1International_Report_-_Costs_and_Rationing_of_Insulin__Diabetes_Supplies_2.pdf Retrieved May 22, 2019, from. [Google Scholar]
- Umpierrez G., Murphy M., Kitabchi A. Diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Diabetes Spectrum. 2002;15(1):28–36. doi: 10.2337/diaspect.15.1.28. [DOI] [Google Scholar]
- Volman B. Direct costs and availability of diabetes medicines in low-income and middle-income countries. World Health Organization, Health Action International. 2008 http://digicollection.org/hss/documents/s18387en/s18387en.pdf [Google Scholar]