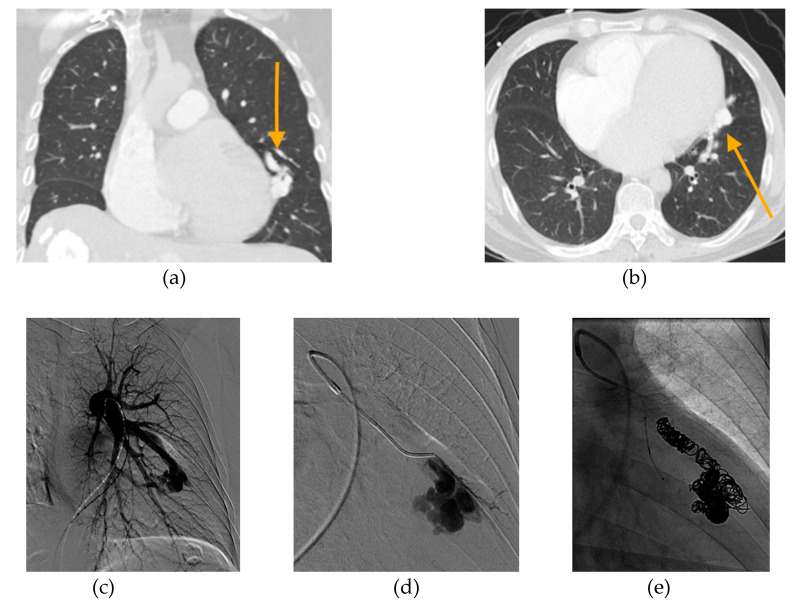
Figure 5.
49-year-old male with history of nonischemic cardiomyopathy, severe mitral and triscuspid regurgitation, PAVM, and PH presented with acute hypoxemic respiratory failure. (a) Axial and (b) coronal CT angiogram images revealing a large PAVM in the lingula (orange arrows). (c) Initial pulmonary angiogram of the left lung demonstrates that a large proportion of pulmonary arterial flow passes through the PAVM, acting as a “pop-off” valve. (d) Selective angiogram shows selection of the feeding artery with filling of the complex PAVM sac. Prior to embolization, patient’s oxygen saturation on 4 L nasal cannula was 89%. Pre-embolization main pulmonary artery pressure (PAP) was 53/21 mmHg (mPAP 33 mmHg). (e) Final pulmonary angiogram shows occlusion of PAVM with combined coiling and deployment of an 8 mm Amplatzer plug in the arterial feeder. Following embolization, PAP increased 72/37 mmHg (mPAP 50 mmHg). Oxygen saturation on 4 L nasal cannula improved to 99%. The patient was weaned to room air and discharged in good condition. Two years later, he was admitted on multiple occasions for acute decompensated heart failure. At 3.5 years after embolization, he died from acute renal failure secondary to cardiorenal syndrome.