Abstract
Coronavirus disease 2019 (COVID-19) is a highly contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Infection with SARS-CoV may cause coronary plaque instability and lead to acute coronary syndrome (ACS). Management of ACS in patients with COVID-19 needs more consideration of the balance between clinical benefit and transmission risk of virus. This review provides recommendations of management strategies for ACS in patients with suspected or confirmed COVID-19 in Taiwan.
Keywords: Acute coronary syndrome, Acute myocardial infarction, Coronavirus disease 2019, Non ST-Segment elevation acute coronary syndrome, ST-Segment elevation myocardial infarction
Introduction
On 12 March, 2020, the World Health Organization (WHO) declared the infection caused by coronavirus disease 2019 (COVID-19) a pandemic due to rapidly spreading outbreaks around the world. The pathogen causes pneumonia and is officially named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the WHO. COVID-19 resulted in a lower case-fatality rate but a stronger transmission capacity compared with the severe acute respiratory syndrome coronavirus (SARS-CoV) that caused an outbreak in 2003.1 In addition to respiratory symptoms and pneumonia, cardiac complications, including acute cardiac injury, heart failure and arrhythmia, could occur in patients with COVID-19.2 , 3 It is reported that 7–17% patients developed acute cardiac injury with elevation of cardiac troponin in hospitalized patients with COVID-19.2 , 3 The risk of cardiac complications of COVID-19 are approximately comparable with other coronavirus disease, such as severe acute respiratory syndrome (SARS) or middle east respiratory syndrome (MERS).4 Previous study reported that SARS-CoV may trigger coronary plaque instability and lead to ACS.5 In patients with COVID-19, increased interleukin-6 and D-dimer indicated enhanced systemic inflammation and augmented coagulation response,3 both of which have linked to plaque instability and occurrence of ACS.
Based on previous SARS experiences, several actions were taken immediately by Taiwan Government and effectively prevents large-scale community outbreaks of COVID-19 in Taiwan so far.6 Strict infection control measures were implemented early in hospitals in Taiwan to protect first-line health care workers and avoid in-hospital transmission.7 Recent study indicated that, in addition to droplet, fomite could be an important nosocomial transmission pathway of SARS-CoV-2 because the virus can remain viable on surfaces up to days.8 Timely percutaneous coronary intervention (PCI) and adequate antithrombotic therapy are the major treatment modalities for ACS.
Management of ACS in patients with suspected or confirmed COVID-19 need to balance the risk of nosocomial virus transmission and benefit of PCI. If PCI is necessary, designated routes for transferring patients into and out of catheterization laboratory are necessary. Adequate personnel protection during intervention with personal protective equipment, including eye protection, face shielding, gown and gloves, is necessary and regulations should be followed according to the infection control team's suggestions in the hospital. Post-procedural sterilization protocol to avoid virus transmission is important. Based on these considerations, this statement from experts in Taiwan Society of Cardiology provides suggestions about management strategy for ACS in patients with suspected or confirmed COVID-19 in Taiwan. Suspected COVID-19 cases were defined as people suffered form an acute respiratory tract infection or other illness similar with COVID-19, or asymptomatic people with close contact to any confirmed COVID-19 patient. Confirmed COVID-19 cases were defined as any person with positive COVID-19 polymerase chain reaction testing.
ST-segment elevation myocardial infarction
Primary PCI is the major reperfusion strategy for ST-segment elevation myocardial infarction (STEMI) in Taiwan.9 , 10 Fibrinolytic therapy could be considered first when primary PCI cannot be performed rapidly for any reason after STEMI diagnosis.11 According to database of ACS registries established by the Taiwan Society of Cardiology, primary PCI was performed in 98.2% of STEMI cases, whereas fibrinolysis therapy was used in only 1.8%.10 , 12
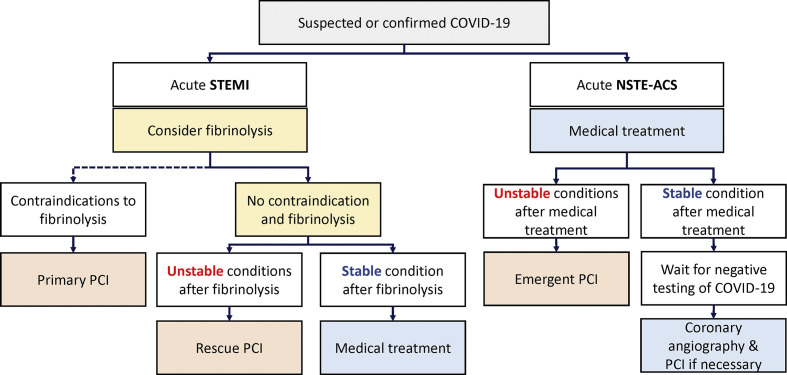
Preliminary study showed strict infection control measures in COVID-19 outbreak delayed door to device time and catheterization laboratory arrival to device time of primary PCI for STEMI.13 When STEMI is encountered in patients with suspected or confirmed COVID-19 in Taiwan, the suggested revascularization strategy is shown in Fig. 1 . Considering the time needed for patient transportation to catheterization laboratory and preparation of personnel protection, it is not easy to achieve optimal door to device time. Fibrinolysis is suggested as the first-line therapy if there is no contraindication, which was also recommended in recent publication.14, 15, 16, 17 In Taiwan, the fibrin-specific agent, human recombinant tissue plasminogen activator (Alteplase, t-PA), is recommended with 15 mg intravenous bolus followed by 0.75 mg/kg over 30 min then 0.5 mg/kg over 60 min intravenous infusion.11 The total t-PA dose should not exceed 100 mg. PCI can be considered if there are contraindications to fibrinolytic therapy or appearance of signs or symptoms indicating failure of fibrinolytic therapy, including unstable hemodynamics, acute pulmonary edema, severe tachy- or bradyarrhythmias or severe ischemia with refractory angina. Otherwise, the patients could be treated medically with secondary preventive medications according the current guideline for STEMI.11
Figure 1.
Revascularization strategy for STEMI and NSTE-ACS in patients with suspected or confirmed COVID-19. NSTE-ACS, non-ST-segment elevation acute coronary syndrome; PCI, percutaneous catheter intervention; STEMI, ST-segment elevation myocardial infarction. Unstable conditions indicate unstable hemodynamics, acute pulmonary edema, severe tachy- or bradyarrhythmias and severe ischemia with refractory angina.
Non ST-segment elevation acute coronary syndrome
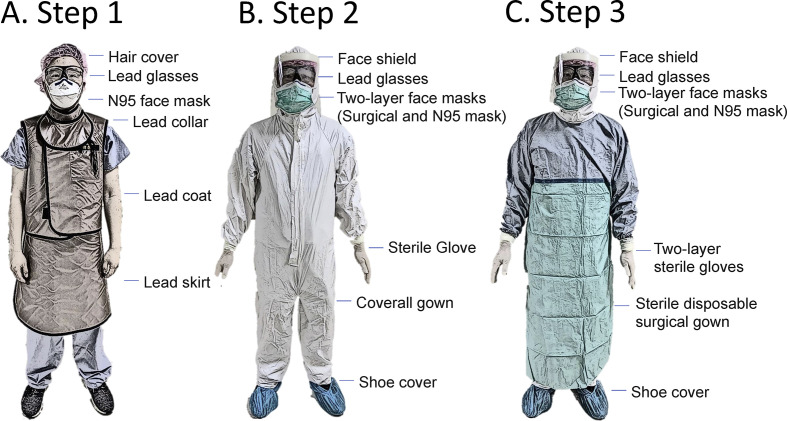
Fig. 1 also shows the recommended revascularization strategy for non ST-segment elevation ACS (NSTE-ACS) patients. Current NSTE-ACS guideline in Taiwan or Europe does not recommend routine coronary angiography for all NSTE-ACS patients.18 , 19 For NSTE-ACS in patients with suspected or confirmed COVID-19 but without symptoms after initial medical treatment, coronary angiography can be delayed until negative testing of SARS-CoV-2 assays are confirmed. However, in the very high risk patients with unstable hemodynamics, acute pulmonary edema, severe tachy- or bradyarrhythmias, and severe ischemia with refractory angina, coronary angiography and PCI should be considered and performed as soon as possible. In patients with COVID-19, sometimes, the clinical distinction maybe difficult between acute cardiac injury and true ACS with acute atherothrombotic event. When the ACS diagnosis is not clear after initial examinations, computed tomography coronary angiography (CTA) is a another diagnostic tool to define coronary anatomy and rule out severe coronary stenosis.20 The recommendations for strategies when treating patients with suspected or confirmed COVID-19 were summarized in Table 1 . Furthermore, personal protective equipment in cardiac catheterization lab was suggested in Fig. 2 , which showed more detailed steps to wear personal protective equipment with compared to previous publication.21
Table 1.
Recommendation for strategies when treating patients with suspected or confirmed COVID-19.
| Preliminary Settings |
| 1. Identify SARS-CoV-2 via available kits in local institute and exclude COVID-19 infection as possible before intervention. |
| 2. For STEMI and NSTEMI patient with very-high-risk, repeated COVID-19 sampling and testing are still needed after PCI considered that assay of take times to display result. |
| 3. Delay PCI if possible until COVID-19 virus screen tests show negative for twice. |
| 4. Reserve a fixed catheterization laboratory for these patients. Negative pressure isolation catheterization lab is suggested if available. |
| 5. Designate specific and fixed routes for entry and out of catheterization laboratory. |
| 6. Reserve at least two groups of interventional cardiologists, nurses and technicians for duty shift. |
| 7. Experienced intervention cartologists and medical staffs are recommended in PCI for AMI patients suspected COVID-19 infection. |
| 8. Keep the staffs in catheterization laboratory as few as possible during the procedure. |
| 9. Prohibit other staffs entry catheterization laboratory area during the procedure. |
| 10. Strict personal protective equipment, including gloves, eye and face protection, N95 mask, and isolation gown, is necessary. |
| 11. Disposable gowns and medical supplies are suggested during PCI. |
| 12. After the procedure, the catheterization laboratory and lead coats should be disinfected according to the suggestions from infection control team. Ultraviolet light disinfection and 500 ppm diluted bleach or other disinfectants can be considered |
| 13. Hand hygiene before or after PCI is critical to protect medical staffs. |
| 14. Use of a high-flow nasal cannula or non-invasive ventilation during PCI is not suggested to prevent aerosol spreading. |
| 15. Negative pressure isolation room for intensive care is recommended in all AMI patients suspected COVID-19 infection. |
| 16. During transport before or after hospitals, emergent medical services should be equipped with adequate protective gear. |
| 17. Transfer for urgent PCI among hospitals is suggested only in patients with unstable hemodynamics, acute pulmonary edema, severe tachy- or bradyarrhythmias or contraindication to fibrinolysis. |
| 18. All medical staffs involved in PCI should be closely monitor for 14 days. |
| ST-segment elevation myocardial infarction (STEMI) Patients |
| 1. Fibrinolysis before feasible intervention in all patients except contraindications. |
| 2. Fibrinolytic therapy is suggested within 12 h of symptom onset if primary PCI is not feasible and there are no contraindications, and fibrin-specific agent (i.e. tenecteplase, alteplase, or reteplase) is preferred compared to non–fibrin-specific agent (i.e. Streptokinase). |
| 3. Primary PCI is suggested in patients contraindicated fibrinolysis. |
| 4. Urgent rescue PCI is considered in patients who fail fibrinolysis with unstable hemodynamics, acute pulmonary edema and severe tachy- or bradyarrhythmias. |
| 5. Delay angiography could only be considered after COVID-19 virus screen negative for twice. |
| Non ST-segment elevation acute coronary syndrome Patients |
| 1. Repeated sampling and testing from lower respiratory specimen are strongly recommended before intervention except very-high-risk patients. |
| 2. For very-high-risk NSTE-ACS patients with unstable hemodynamics, acute pulmonary edema and severe tachy- or bradyarrhythmias, intervention is suggested within 2 h from hospital admission. |
| 3. Early coronary angiography is suggested within 24 h for high risk patients, until COVID-19 virus screen tests show negative for once or twice. |
| 4. Invasive intervention is suggested in 72 h for intermediate risk patients until COVID-19 virus screen tests show negative for twice |
| 5. Selective intervention can be considered for low risk patients until COVID-19 virus screen tests show negative for twice, if there is evidence of inducible ischemia in a non-invasive stress test. |
AMI: Acute myocardial infarction; COVID-19: coronavirus disease 2019; NSTE-ACS Non ST-segment elevation acute coronary syndrome; PCI: percutaneous coronary intervention; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; STEMI: ST-elevation myocardial infarction.
Figure 2.
Personal protective equipment suggested in cardiac catheterization lab. The 3 steps were recommended for staffs to wear personal protective equipment in cardiac catheterization. Step 1: Hair cover, lead glasses, collar, coat and skirt were suggested as daily practice. N95 face mask should be worn at this step. Step 2: Face shield, shoe cover, sterile glove and coverall gown were suggested. Two-layer face masks should be worn with surgical on N95 face masks. Step 3: Disposable surgical gown and two-layer sterile gloves were suggested.
Conclusions
The outbreak of COVID-19 causes great impact on the health care system and practicing behaviors of medical profession. For management of ACS in patients with suspected or confirmed COVID-19, fibrinolysis could be administered first and reserve PCI for those with failed fibrinolysis in STEMI. For NSTE-ACS, coronary angiography and PCI are considered only for very high risk patients that symptoms cannot be stabilized after adequate medical treatment. Personnel protection to avoid in-hospital viral transmission is crucial in catheterization laboratory. Since the pandemic is still ongoing and scientific data are limited, the protocols recommended in this review only reflect the viewpoints at current stage. More information is needed to determine which way could provide optimal care for these patients and protect healthcare workers at the same time.
Funding
This study was supported by grants from the Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, i.e., Grant Nos. VGHKS 19-CT10-04 and the Ministry of Science and Technology, i.e., Grants 108-2314-B-075B-007 -MY2.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
References
- 1.Deng S.Q., Peng H.J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020;9:E575. doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. J Am Med Assoc. 2020;323:1060–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y., Li J., Feng Y. Critical care response to a hospital outbreak of the 2019-nCoV infection in Shenzhen, China. Crit Care. 2020;24(1):56. doi: 10.1186/s13054-020-2786-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020 May;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsui K.L., Leung T.C., Yam L.Y., So L.K.-Y., Poon E., Lung K.-C., et al. Coronary plaque instability in severe acute respiratory syndrome. Int J Cardiol. 2005;99:471–472. doi: 10.1016/j.ijcard.2003.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. J Am Med Assoc. 2020 Mar 3;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz J., King C.C., Yen M.Y. Protecting health care workers during the COVID-19 coronavirus outbreak -lessons from Taiwan's SARS response. Clin Infect Dis. 2020 Mar 12 doi: 10.1093/cid/ciaa255. ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 Mar 17;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y.H., Chiu Y.W., Cheng J.J., Hsieh I.C., Lo P.H., Lei M.H., et al. Changing practice pattern of acute coronary syndromes in Taiwan from 2008 to 2015. Acta Cardiol Sin. 2019;35:1–10. doi: 10.6515/ACS.201901_35(1).20180716B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu C.K., Juang J.J., Chiang J.Y., Li Y.H., Tsai C.T., Chiang F.T. The Taiwan Heart Registries: its influence on cardiovascular patient care. J Am Coll Cardiol. 2018;71:1273–1283. doi: 10.1016/j.jacc.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Li Y.H., Yeh H.I., Tsai C.T., Liu P.Y., Lin T.H., Wu T.C., et al. 2012 Guidelines of the Taiwan Society of Cardiology (TSOC) for the management of ST-segment elevation myocardial infarction. Acta Cardiol Sin. 2012;28:63–89. [Google Scholar]
- 12.Chou L.P., Zhao P., Kao C., Chen Y.H., Jong G.P. Women were noninferior to men in cardiovascular outcomes among patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention from Taiwan acute coronary syndrome full-spectrum registry. Medicine (Baltim) 2018;97(43) doi: 10.1097/MD.0000000000012998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam C.F., Cheung K.S., Lam S., Wong A., Yung A., Sze M., et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcome. 2020 Mar 17 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han Y. A treatment strategy for acute myocardial infarction and personal protection for medical staff during the COVID-19 epidemic: the Chinese experience. Eur Heart J. 2020 Jun 14;41(23):2148–2149. doi: 10.1093/eurheartj/ehaa358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jing Z.C., Zhu H.D., Yan X.W., Chai W.Z., Zhang S. Recommendations from the Peking union medical college hospital for the management of acute myocardial infarction during the COVID-19 outbreak. Eur Heart J. 2020 May 14;41(19):1791–1794. doi: 10.1093/eurheartj/ehaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Welt F.G.P., Shah P.B., Aronow H.D., Bortnick A.E., Henry T.D., Sherwood M.W., et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC's interventional council and SCAI. J Am Coll Cardiol. 2020 May 12;75(18):2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szerlip M., Anwaruddin S., Aronow H.D., Cohen M.G., Daniels M.J., Dehghani P., et al. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic perspectives from the society for cardiovascular angiography and interventions emerging leader mentorship (SCAI ELM) members and graduates. Cathet Cardiovasc Interv. 2020 Mar 25 doi: 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 18.Li Y.H., Wang Y.C., Wang Y.C., Liu J.C., Lee C.H., Chen C.C., et al. 2018 Guidelines of the Taiwan society of Cardiology, Taiwan society of emergency medicine and Taiwan society of cardiovascular interventions for the management of non ST-segment elevation acute coronary syndrome. J Formos Med Assoc. 2018;117:766–790. doi: 10.1016/j.jfma.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Roffi M., Patrono C., Collet J.P., Mueller C., Valgimigli M., Andreotti F., et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of Cardiology (ESC) Eur Heart J. 2016;37(3):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 20.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020 Mar 16 doi: 10.1093/eurheartj/ehaa190. ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chieffo A., Stefanini G.G., Price S., Barbato E., Tarantini G., Karam N., et al. EAPCI position statement on invasive management of acute coronary syndromes during the COVID-19 pandemic. Eur Heart J. 2020 May 14;41(19):1839–1851. doi: 10.1093/eurheartj/ehaa381. [DOI] [PMC free article] [PubMed] [Google Scholar]